https://www.axios.com/2024/04/11/drug-shortage-record-high

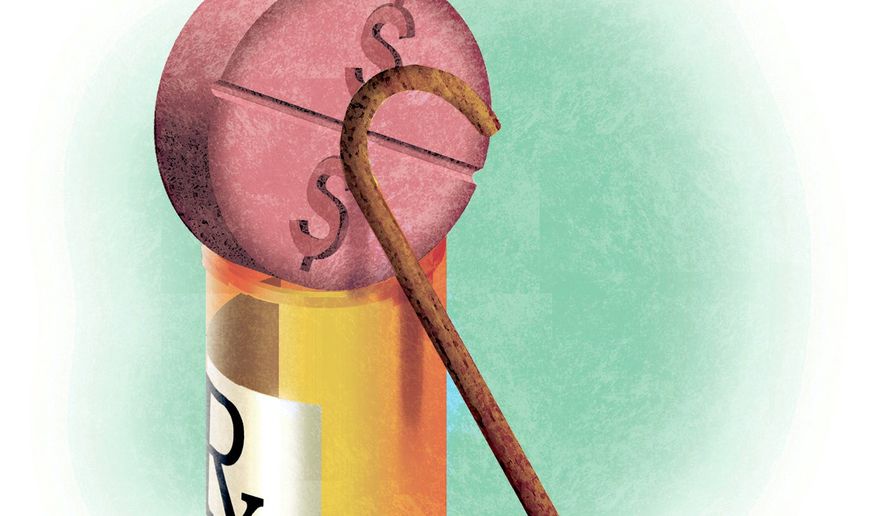
With 323 medicines in short supply, U.S. drug shortages have risen to their highest level since the American Society of Health-System Pharmacists began tracking in 2001.
Why it matters:
This high-water mark should energize efforts in Congress and federal agencies to address the broken market around what are often critical generic drugs, the organization says.
- The Biden administration last week issued a drug-shortage plan that called on Congress to pass legislation that would reward hospitals for maintaining an adequate supply of key drugs, among other measures.
- As a “first step,” Medicare yesterday proposed incentives for roughly 500 small hospitals to establish and maintain a six-month buffer stock of essential medicines.
The big picture:
Many of the issues behind shortages are tied to low prices for generics that leave manufacturers competing on price.
- “It’s been a race to the bottom. We need more transparency around quality so that buyers have a reason to not chase the lowest price,” said Michael Ganio, senior director at the ASHP.
- Drugmakers that can demonstrate safer, higher-quality manufacturing practices should earn a higher price, he said.
- Manufacturing quality concerns in particular have fueled shortages of chemotherapy drugs and some antibiotics.
Between the lines: Other factors are also driving drug shortages.
- Controlled substances, such as pain and sedation medications, account for 12% of active shortages, which are tied to recent legal settlements and Drug Enforcement Administration changes to production limits, per ASHP.
- Not surprisingly, the blockbuster category of anti-obesity drugs known as GLP-1s are in shortage largely because of outsized demand.
- That’s also the case for ADHD drugs and hormone therapies used in gender-affirming care.