https://khn.org/news/california-hospitals-face-surge-with-proven-fixes-and-some-hail-marys/

California’s hospitals thought they were ready for the next big disaster.
They’ve retrofitted their buildings to withstand a major earthquake and whisked patients out of danger during deadly wildfires. They’ve kept patients alive with backup generators amid sweeping power shutoffs and trained their staff to thwart would-be shooters.
But nothing has prepared them for a crisis of the magnitude facing hospitals today.
“We’re in a battle with an unseen enemy, and we have to be fully mobilized in a way that’s never been seen in our careers,” said Dr. Stephen Parodi, an infectious disease expert for Kaiser Permanente in California. (Kaiser Health News, which produces California Healthline, is not affiliated with Kaiser Permanente.)
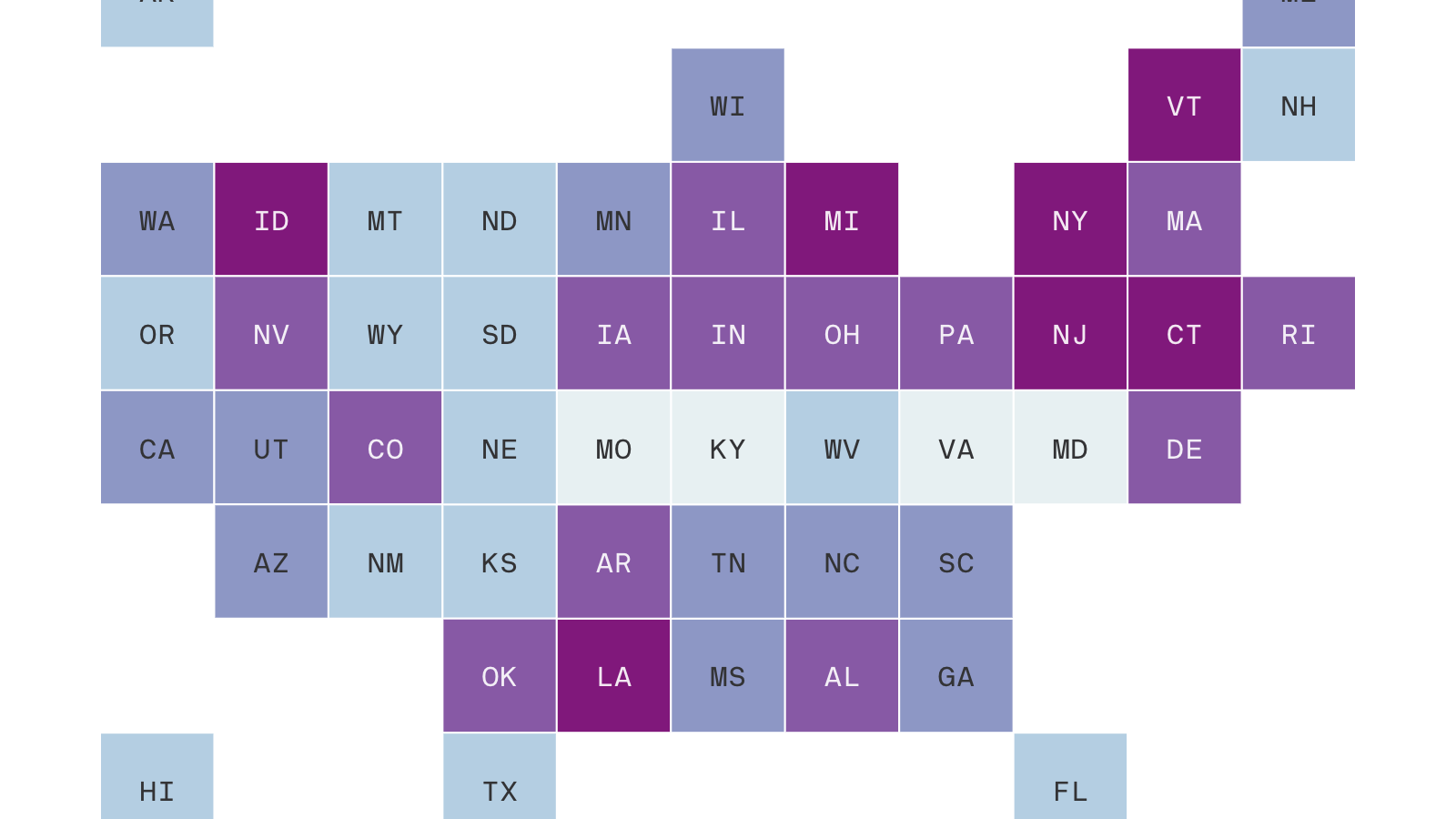
As California enters the most critical period in the state’s battle against COVID-19, the state’s 416 hospitals — big and small, public and private — are scrambling to build the capacity needed for an onslaught of critically ill patients.
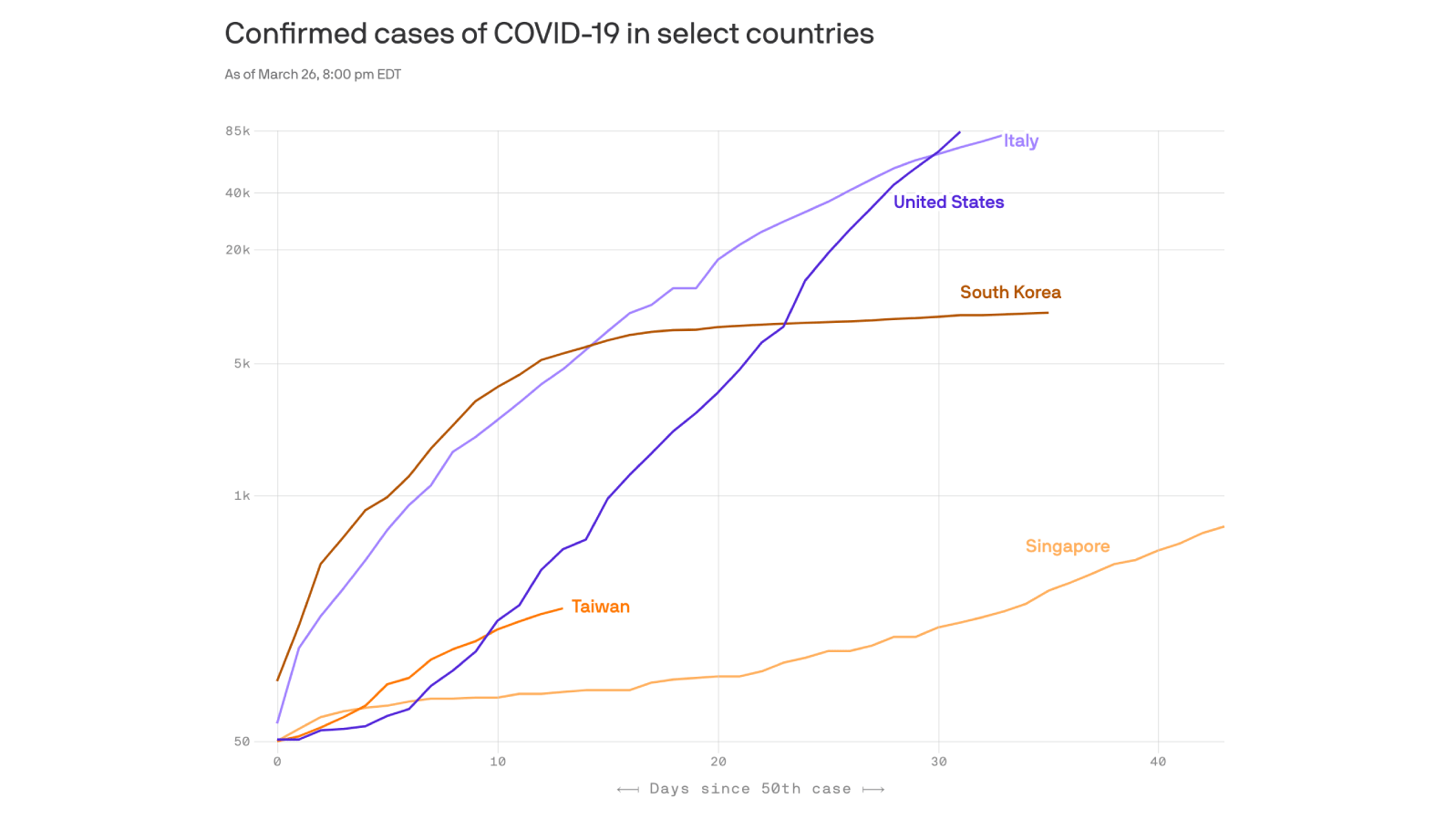
Hospitals from Los Angeles to San Jose are already seeing a steady increase in patients infected by the virus, and so far, hospital officials say they have enough space to treat them. But they also issued a dire warning: What happens over the next four to six weeks will determine whether the experience of California overall looks more like that of New York, which has seen an explosion of hospitalizations and deaths, or like that of the San Francisco Bay Area, which has so far managed to prevent a major spike in new infections, hospitalizations and death.
Some of their preparations share common themes: Postpone elective surgeries. Make greater use of telemedicine to limit face-to-face contact. Erect tents outside to care for less critical patients. Add beds — hospital by hospital, a few dozen at a time — to spaces like cafeterias, operating rooms and decommissioned wings.
But by necessity — because of shortages of testing, ventilators, personal protective equipment and even doctors and nurses — they’re also trying creative and sometimes untried strategies to bolster their readiness and increase their capacity.
In San Diego, hospitals may use college dormitories as alternative care sites. A large public hospital in Los Angeles is turning to 3D printing to manufacture ventilator parts. And in hard-hit Santa Clara County, with a population of nearly 2 million, public and private hospitals have joined forces to alleviate pressure on local hospitals by caring for patients at the Santa Clara Convention Center.
Yet some hospitals acknowledge that, despite their efforts, they may end up having to park patients in hallways.
“The need in this pandemic is so different and so extraordinary and so big that a hospital’s typical surge plan will be insufficient for what we’re dealing with in this state and across the nation,” said Carmela Coyle, president and CEO of the California Hospital Association.
Across the U.S., more than 213,000 cases of COVID-19 have been confirmed, and at least 4,750 people have died. California accounts for more than 9,400 cases and at least 199 deaths.
Health officials and hospital administrators are singling out April as the most consequential month in California’s effort to combat a steep increase in new infections. State Health and Human Services Secretary Mark Ghaly said Wednesday that the number of hospitalizations is expected to peak in mid-May.
Gov. Gavin Newsom said there were 1,855 COVID-19 cases in hospitals Wednesday, a number that had tripled in six days, and 774 patients in critical care. By mid-May, the number of critical care patients is expected to climb to 27,000, he said.
Newsom said the state needs nearly 70,000 more hospital beds, bringing its overall capacity to more than 140,000 — both inside hospitals and also at alternative care sites like convention centers. The state also needs 10,000 more ventilators than it normally has to aid the crush of patients needing help to breathe, he said, and so far has acquired fewer than half.
Newsom and state health officials worked with the Trump administration to bring a naval hospital ship to the Port of Los Angeles, where it is already treating patients not infected with the novel coronavirus. The state is working with the Army Corps of Engineers to deploy eight mobile field hospitals, including one in Santa Clara County. And it is bringing hospitals back online that were shuttered or slated to close, including one each in Daly City, Los Angeles, Long Beach and Costa Mesa.
The governor is also drafting a plan to make greater use of hotels and motels and nursing homes to house patients, if needed.
But the size of the surge that hits hospitals depends on how well the public follows social distancing and stay-at-home orders, said Newsom and hospital administrators. “This is not just about health care providers caring for the sick,” said Dr. Steve Lockhart, the chief medical officer of Sutter Health, which has 22 hospitals across Northern California.
While hospitals welcomed the state assistance, they’re also undertaking dramatic measures to prepare on their own.
“I’m genuinely very worried, and it scares me that so many people are still out there doing business as usual,” said Chris Van Gorder, CEO of Scripps Health, a system with five major hospitals in San Diego County. “It wouldn’t take a lot to overwhelm us.”
Internal projections show the hospital system could need 8,000 beds by June, he said. It has 1,200.
In addition to taking precautions to protect its health care workers — such as using baby monitors to observe patients without risking infection — it is working with area colleges to use dorm rooms as hospital rooms for patients with mild cases of COVID-19, among other efforts, he said.
“Honestly, I think we should have been better prepared than we are,” Van Gorder said. “But hospitals cannot take on this burden themselves.”
Van Gorder and other hospital administrators say a continued shortage of COVID-19 tests has hampered their response — because they still don’t know exactly which patients have the virus — as has the chronic underfunding of public health infrastructure.
Kaiser Permanente wants to double the capacity of its 36 California hospitals, Parodi said. It is also working with the garment industry to manufacture face masks, and eyeing hotel rooms for less critical patients.
Harbor-UCLA Medical Center, a 425-bed safety-net hospital in Los Angeles, is working to increase its capacity by 200%, said Dr. Anish Mahajan, the hospital’s chief medical officer.
Harbor-UCLA is using 3D printers to produce ventilator piping equipped to serve two patients per machine. And in March it transformed a new emergency wing into an intensive care unit for COVID-19 patients.
“This was a shocking thing to do,” Mahajan said of the unprecedented move to create extra space.
He said some measures are untested, but hospitals across the state are facing extreme pressure to do whatever they can to meet their greatest needs.
In March, Stanford Hospital in the San Francisco Bay Area launched a massive telemedicine overhaul of its emergency department to reduce the number of employees who interact with patients in person. This is the first time the hospital has used telemedicine like this, said Dr. Ryan Ribeira, an emergency physician who spearheaded the project.
Stanford also did some soul-searching, thinking about which of its staff might be at highest risk if they catch COVID-19, and has assigned them to parts of the hospital with no coronavirus patients or areas dedicated to telemedicine. “These are people that we might have otherwise had to drop off the schedule,” Ribeira said.
Nearby, several San Francisco hospitals that were previously competitors have joined forces to create a dedicated COVID-19 floor at Saint Francis Memorial Hospital with four dozen critical care beds.
The city currently has 1,300 beds, including 200 ICU beds. If the number of patients surges as it has in New York, officials anticipate needing 5,000 additional beds.
But the San Francisco Bay Area hasn’t yet seen the expected surge. UCSF Health had 15 inpatients with COVID-19 Tuesday. Zuckerberg San Francisco General Hospital and Trauma Center had 18 inpatients with the disease Wednesday.
While hospital officials are cautiously optimistic that local and state stay-at-home orders have worked to slow the spread of the virus, they are still preparing for what could be a major increase in admissions.
“The next two weeks is when we’re really going to see the surge,” said San Francisco General CEO Susan Ehrlich. “We’re preparing for the worst but hoping for the best.”