Category Archives: Short Term Health Insurance
Cartoon – The Tin Plan (aka Short Term Health Insurance)
Tightening the Rules Around Short-Term Health Insurance Plans Won’t Lead to More People Going Without Insurance

Short-term, limited-duration insurance (STLDI) plans are exempt from the Affordable Care Act’s (ACA) essential benefit coverage requirements and from prohibitions on medical underwriting.
This means that consumers with preexisting conditions can be denied coverage and anyone who purchases such a plan may lack coverage for key services.
In August 2018, under the Trump administration, the U.S. Department of Health and Human Services revised the definition of short-term plans to include coverage with an initial term of less than 12 months that could be renewed for up to 36 months. While the purported goal of this change was to increase coverage and reduce uninsured rates, our analysis indicates that it did not accomplish this: coverage did not increase and the uninsured rate did not drop.
In July 2023, the Biden administration issued a notice to limit the initial duration of short-term plans to three months, with an option to renew for one additional month. This change was intended to ensure that people purchasing insurance coverage have meaningful protection and to preserve the preexisting condition protections in the ACA.
Critics feared and some cost estimates suggested that tightening the STLDI rules could leave many without any coverage at all.
In 2019, the Congressional Budget Office (CBO), using its forecast model (data were not yet available), estimated that 1.5 million people would purchase short-term plans and that 500,000 would gain coverage (relative to being uninsured). Our analysis suggests that these forecasts substantially overstated the effects of the rule change; far fewer people enrolled in STLDI plans and the enrollment that did occur was from people moving off marketplace coverage.
There is no evidence that the number of uninsured people declined because these plans became available.
Using data from the American Community Survey and marketplace enrollment from the Centers for Medicare and Medicaid Services (CMS), we assessed whether the loosening of STLDI regulations (under the Trump administration) led to increased enrollment in off-marketplace nongroup coverage in states that permitted sales compared to those that did not. Plans sold off the marketplace include STLDI as well as ACA-compliant plans, grandfathered coverage, health care sharing ministries, and fixed indemnity plans. Next, we looked to see whether the Trump-era regulations increased nongroup insurance coverage altogether (including marketplace coverage) in these states. Finally, we looked to see whether the broader availability of STLDI was associated with lower uninsured rates. We examined coverage patterns for adults ages 26 to 64 and then focused on young men ages 26 to 35, who may be most sensitive to the presence of regulations similar to those in the ACA because they are less likely to have preexisting conditions or to seek comprehensive coverage.
In 2017, 2.6 million adults ages 26 to 64, about 1.6 percent of that population, purchased private nongroup insurance outside the marketplace. By 2020, about 270,000 more people were enrolled in off-marketplace nongroup plans, across all states, than had been in 2017. There was a larger increase in off-marketplace nongroup enrollment among all adults and among young adults (we cannot separate young men in the CMS data) in states that permitted the sale of STLDI coverage, compared to those that prohibited it. This is consistent with the evidence of growth in sales of these plans. Across all states, about 160,000 more young adults, ages 26 to 34, held off-marketplace nongroup coverage in 2020 than in 2017.
The ACS data show that off-marketplace plans largely substituted for marketplace plans in states that permitted the sale of STLDI. Patterns of enrollment in nongroup plans overall were very similar in states with and without STLDI plans available for purchase over this period. While nongroup coverage was consistently more popular in states with no restrictions, between 2017 and 2020 enrollment in nongroup plans declined slightly more in states where STLDI plans were available for purchase than in those where they were not. The same pattern of marginally greater declines held for young men (and young adults) in states where STLDI plans were available.
Nongroup coverage was slightly higher in states where STLDI plans were available for sale, but the overall uninsured rate is much higher in these states, primarily because many did not expand Medicaid eligibility.
The gap in uninsured rates between states with STLDI plans available and those in which they were not available widened through 2018, narrowed slightly in 2019, and rose again in 2020. Patterns among young men were similar.
The lack of reliable information on STLDI plans and the small size of the market make it difficult to draw strong inferences about how changes in regulations affected participation. Nonetheless, by comparing states where the 2018 regulatory changes took effect and those where they did not, we are able to rule out any notable effects. A modest number of people — no more than one-fifth of the 1.5 million the CBO projected — are likely to have enrolled in STLDI plans that became available after the Trump administration’s regulatory change. This enrollment mainly appears to have displaced marketplace coverage.
There is no evidence that the broader availability of STLDI plans had any meaningful effect on nongroup coverage in general or on uninsurance, either in the full population or among young men.
This suggests that the Biden administration’s proposed tightening of STLDI is unlikely to have substantial negative effects on nongroup coverage or uninsurance. Instead, limiting STLDI will likely strengthen the health insurance marketplaces that offer reliable, comprehensive nongroup coverage.
How Do Democrats and Republicans Rate Healthcare for 2024?

It feels as though November 5, 2024 is far away, but for both Democrats and Republicans, the election is now. On the issue of healthcare, the two parties’ approaches differ sharply.
Think back to the behemoth effort by Republicans to “repeal and replace” the Affordable Care Act six years ago, an effort that left them floundering for a replacement, basically empty-handed. Recall the 2022 midterms, when their candidates in 10 of the tightest House and Senate races uttered hardly a peep about healthcare.
That reticence stood in sharp contrast to Democrats who weren’t shy about reiterating their support for abortion rights, simultaneously trying hard to ensure that Americans understood and applauded healthcare tenets in the Inflation Reduction Act.
As The Hill noted in early August, sounds like the same thing is happening this time around as America barrels toward November 2024. The publication said it reached to 10 of the leading Republican candidates about their plans to reduce healthcare costs and make healthcare more affordable, and only one responded: Rep. Will Hurd (R-Texas).
Healthcare ‘A Very Big Problem’
Maybe the party thinks its supporters don’t care. But, a Pew Research poll from June showed 64% of us think healthcare affordability is a “very big problem,” superseded only by inflation. In that research, 73% of Democrats and 54% of Republicans thought so.
Chuck Coughlin, president and CEO of HighGround, an Arizona-based public affairs firm, told The Hill that the results aren’t surprising.
“If you’re a Republican, what are you going to talk about on healthcare?” he said.
Observers note that the party has homed in on COVID-lockdowns, transgender medical rights, and yes, abortion.
Republicans Champion CHOICE
There is action on this front, for in late July, House Republicans passed the CHOICE Arrangement Act. Its future with the Democratic-controlled Senate is bleak, but if Republicans triumph in the Senate and White House next year, it could advance with its focus on short-term health plans. They don’t offer the same broad ACA benefits and have a troubling list of “what we won’t cover” that feels like coverage is going backwards to some.
Plans won’t offer coverage for preexisting conditions, maternity care, or prescription drugs, and they can set limits on coverage. The plans will make it easier for small employers to self-insure, so they don’t have to adhere to ACA or state insurance rules.
CHOICE would let large groups come together to buy Association Health Plans, said NPR, which noted that in the past, there have been “issues” with these types of plans.
Insurance experts say that the act takes a swing at the very foundation of the ACA. As one analyst described it, the act intends to improve America’s healthcare “through increased reliance on the free market and decreased reliance on the federal government.”
Democrats Tout Reduce-Price Prescriptions
Meanwhile, on Aug. 29, President Joe Biden spoke proudly in The White House: “Folks, there’s a lot of really great Republicans out there. And I mean that sincerely…But we’ll stand up to the MAGA Republicans who have been trying for years to get rid of the Affordable Care Act and deny tens of millions of Americans access to quality, affordable healthcare.”
Current ACA enrollment is higher than 16 million.
He said that Big Pharma charges Americans more than three times what other countries charge for medications. And on that date, he announced that “the (Inflation Reduction Act) law finally gave Medicare the power to negotiate lower prescription drug prices.” He wasn’t shy about saying that this happened without help from “the other team.”
The New York Times said it feels this push for lower healthcare costs will be the centerpiece of his re-election campaign. The announcement confirmed that his administration will negotiate to lower prices on 10 popular—and expensive drugs—that treat common chronic illnesses.
It said previous research shows that as many as 80% of Americans want the government to have the power to negotiate.
The president also said that “Next year, Medicare will select more drugs for negotiation.” He added that his administration “is cracking down on junk health insurance plans that look like they’re inexpensive but too often stick consumers with big hidden fees.” And it’s tackling the extensive problem of surprise medical bills.
Earlier, on August 11, Biden and fellow Democrats celebrated the first anniversary of the PACT Act, legislation that provides healthcare to veterans exposed to toxic burn pits while serving. He said more than 300,000 veterans and families have received these services, with more than 4 million screened for toxic exposure conditions.
Push for High-Deductible Plans
Republicans want to reduce risk of high-deductible plans and make them more desirable—that responsibility is on insurers. According to Politico, these plans count more than 60 million people as members, and feature low premiums and tax advantages. The party said plans will also help lower inflation when people think twice about seeking unneeded care.
The plans’ low monthly premiums offer comprehensive preventive care coverage: physicals, vaccinations, mammograms, and colonoscopies, and have no co-payments, Politico said. The “but” in all this is that members will pay their insurers’ negotiated rate when they’re sick, and for medicines and surgeries. Minimum deductible is $1,500 or $3,000 for families—and can be even higher.
Members can fund health savings accounts but can’t fund flexible spending accounts.
Proponents cite more access to care, and reduced costs due to promotion of preventive care. Nay-sayers worry about lower-income members facing costly bills due to insufficient coverage.
Republican Candidates Diverge on Medicaid
The American Hospital Association (AHA) doesn’t love these high deductible plans. It explained that members “find they can’t manage the gap between what their insurance pays and what they themselves owe as a result,” and that, AHA said, contributes to medical debt—something the association wants to change.
An Aug. 3 Opinion in JAMA Health Forum pointed out other ways the two parties diverge on healthcare. For example, the piece cited Biden’s incentives for Medicaid expansion. In contrast, Florida Governor Ron DeSantis, a Republican presidential candidate, has not worked to offer Medicaid to all lower-income residents under the ACA. Former Governor Nikki Haley of South Carolina feels the same, doing nothing. However, former New Jersey Governor Chris Christie has expanded it, as did former Vice President Mike Pence, when he governed Indiana.
Undoubtedly, as in presidential elections past, healthcare will be at least a talking point, with Democrats likely continuing to make it a central focus, as before.
GOP allies drawing up health plans for a Republican administration
Influential conservative policy groups are sketching out health care plans for a potential Republican administration over a year before the election.
Why it matters:
Republicans have moved on from the “repeal and replace” — the Affordable Care Act didn’t even get a mention in the first GOP presidential debate last week — but still haven’t settled on new health care agenda.
- Republican-aligned groups are stepping in to build out ideas for a party platform that may not be as ambitious as an ACA replacement but could still shift health care policy in a conservative direction on everything from Medicaid to abortion to public health.
Context:
The early push to define the next GOP health agenda partly stems from Republicans’ inability to agree on an ACA alternative after former President Trump was elected, despite years of promises to overhaul the 2010 health care law. The GOP policy experts also said they want to avoid repeating the Trump administration’s failure to plan health care executive actions and key staffing decisions before taking office.
- “A large part of it comes from the experience of 2017. There wasn’t a clear agenda that was ready to go,” said Brian Blase, a former Trump administration health official who’s now president of the right-leaning Paragon Health Institute.
Details:
Conservative think tanks are looking to advance some long-held conservative goals like transforming Medicaid’s open-ended entitlement into block grants, but there’s also a new generation of Trump alumni who hope to revive some of his administration’s policies.
- These include initiatives like encouraging businesses to form association health plans, and pushing even further on price transparency and curbing higher payments to hospitals’ outpatient departments.
- Some are also drawing up plans for limiting the CDC’s power over public health policy in reaction to what they view as the agency’s failed response to the COVID-19 pandemic.
Zoom in:
Paragon Health, as well as the Heritage Foundation and America First Policy Institute, are the primary conservative think tanks now drafting health regulations, policy plans and recruiting personnel who could serve in a Republican administration.
- A roadmap from Paragon envisions a burst of rulemaking at the beginning of a new administration, mostly through the Department of Health and Human Services.
Meanwhile, the America First Policy Institute, founded by Trump administration alumni in 2021, has put forward a 12-part health policy agenda it describes as “radical incrementalism.”
- That’s an acknowledgement that they’re not planning a major health care overhaul, but a belief that significant changes are possible in the current structure, said former Louisiana Gov. Bobby Jindal, who chairs the group’s health policy division.
- “We are advocating specific policies that try to reform our health care system in a very specific direction that empowers patients … that makes health care more affordable, accessible, that improves outcomes by giving control back to individual patients working with their providers, not government agencies and programs. But, we’re not trying to write the next 3,000-page bill,” Jindal said.
- Some of those incremental ideas they hope could get bipartisan support, such as broadening health savings accounts for those with chronic conditions, expanding telehealth flexibilities for providers across state lines, implementing transparency for pharmacy benefit managers and speeding up deployment of biosimilars.
The Heritage Foundation has also detailed policy proposals and recently joined more than 70 other conservative groups to launch an initiative called Project 2025 to develop a governing agenda.
- One of those Heritage policy proposals laid out earlier this year illustrates how a future GOP president could overhaul HHS.
- Heritage’s plan contains the most detailed ideas for how the next GOP president — who would be the first since the demise of Roe v. Wade — could implement anti-abortion policies, cut off Medicaid funding to Planned Parenthood, and roll back Biden administration initiatives aimed at increasing access to abortion.
- The group also envisions splitting CDC into two agencies — one for research and data collection and another for making public health recommendations with “severely confined ability” to influence policy.
What we’re watching: The GOP presidential candidates themselves have said relatively little so far about their plans for the health care system. That could eventually change, given Americans’ concern over health care costs.
Biden administration proposes rollback of short-term health plan expansion
https://mailchi.mp/cc1fe752f93c/the-weekly-gist-july-14-2023?e=d1e747d2d8
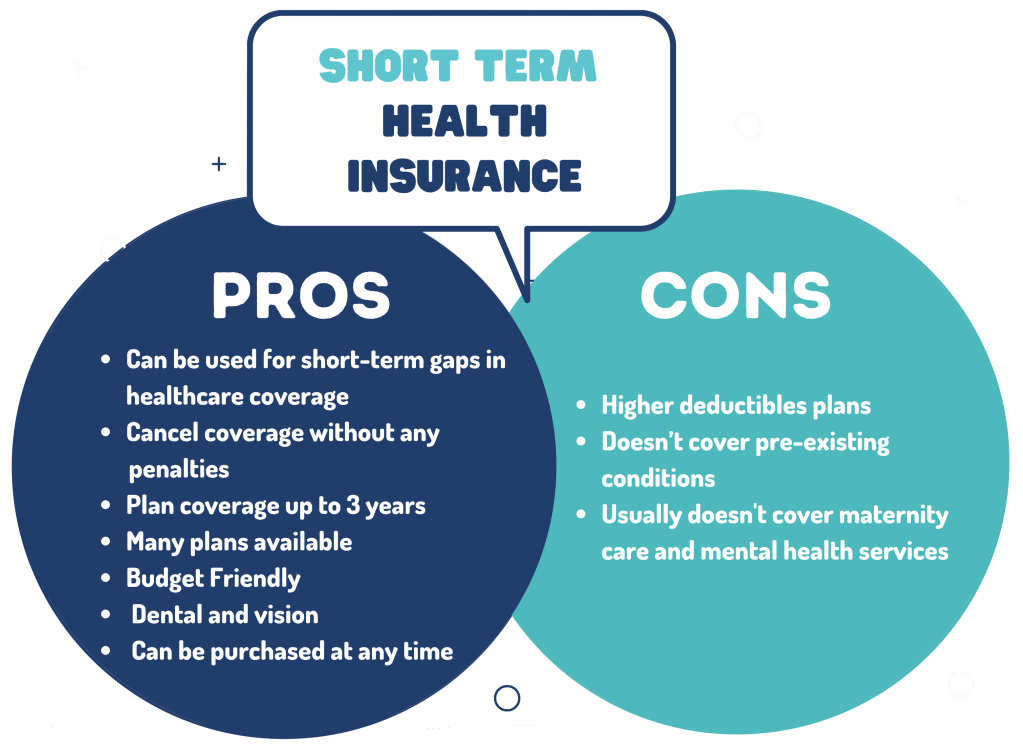
Last Friday, the Department of Health and Human Services, the Treasury Department, and the Department of Labor jointly issued several proposed rules to shore up consumer healthcare protections, including reversal of a Trump administration policy that allowed consumers to enroll in short-term health plans, which were intended to serve as limited coverage options during transitional periods, for up to three years. Approximately 3M people were enrolled in these plans in 2019.
A new rule would limit consumer access to these plans to just three months, with an optional one-month extension, while also requiring payers to disclose clearly how their plans fall short of comprehensive health insurance.
The Gist: In an expected move, the Biden administration continues its unwinding of the Trump-era policies it sees as undermining the Affordable Care Act’s (ACA’s) mission of guaranteeing robust, accessible insurance for all.
Short-term plans, which were granted an exemption from the ACA requirement that health plans cover ten essential health benefits, have been found to discriminate against people with pre-existing conditions, revoke coverage for enrollees retroactively, and generate excess surprise bills due to their limited networks.
High-deductible and skinny health insurance plans drive medical debt
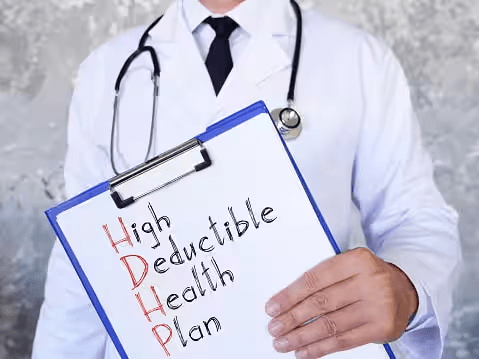
A recent Urban Institute report highlights the issue of medical debt but fails to examine two of the chief driving forces of this debt: inadequate enrollment in comprehensive health care coverage and high-deductible health plans that intentionally push more costs onto patients. It also fails to appreciate the looming crisis when the public health emergency ends and Medicaid enrollment could plummet.
As the extent of medical debt shows, both the government and the private market is failing too many patients, leaving too many either uninsured or with subpar plans that expose too many people to bills they cannot afford to pay. While hospital financial assistance is crucial to helping many individuals of limited means access care, it is no substitute for a solution that gets to the root causes of medical debt.
Affordable, comprehensive health care coverage is the most important protection against medical debt. While the U.S. health care system has achieved record rates of coverage, significant gaps remain and new threats are on the horizon. One of the gaps is the failure by some states to expand Medicaid, while the most imminent threat is the potential loss of Medicaid coverage for millions of people as the public health emergency ends. We must ensure that every individual has access to some form of comprehensive coverage.
In doing so, we must put an end to deceptively inadequate health plans. These include short-term limited duration health plans and health sharing ministries that often appeal to consumers because they are cheaper and often marketed to appear comprehensive. The reason they are cheaper is because when you read the fine print you discover they cover fewer benefits and include few-to-no consumer protections, like required coverage of pre-existing conditions and limits on out-of-pocket costs. Subscribers for these types of plans often find themselves responsible for their entire medical bill without any help from their health plan and can accumulate significant medical debt.
Many of the same concerns apply to high-deductible health plans. These plans are specifically designed to increase patients’ financial exposure through high cost-sharing – the amount the subscriber must pay out-of-pocket. Yet, many individuals enrolled in these plans find they can’t manage the gap between what their insurance pays and what they themselves owe as a result. It’s not a mystery why high-deductible health plans contribute to medical debt.
Hospitals and other providers do not determine how much insured patients owe for their care. Instead, that amount is set by the health plan. While every hospital has a financial assistance policy to help those most in need, they can only help so much and so many. And no matter how generous, hospital financial assistance will never be a substitute for a health plan that covers preventive and necessary care at an affordable price on the front and back end of coverage.
We must tackle the problem of medical debt, and we must do so at the root: ensuring all individuals are enrolled in comprehensive health care coverage and ending deceptive marketing of health plans and unaffordable cost-sharing.
Potential solutions include:
- Restricting the sale of high-deductible health plans to only those individuals with the demonstrated means to afford the associated cost-sharing.
- Prohibiting the sale of health sharing ministry products and short-term limited duration plans that go longer than 90 days.
- Lowering the maximum out-of-pocket cost-sharing limits.
- Eliminating the use of deductibles and co-insurance and rely solely on flat co-payments, which are easier for patients to anticipate.
- Removing providers from the collection of cost-sharing altogether and require that health plans collect directly from their enrollees the cost-sharing payments they impose. This approach would eliminate the vast majority of patient bills from providers altogether.
Moreover, the AHA has been actively engaged in identifying and promoting best practices in patient billing for decades. The AHA updated our voluntary patient billing guidance in 2020. The guidelines include assisting patients who cannot pay for the care they receive and protecting patients from certain debt collection practices, such as garnishment of wages, liens, interest on debt, adverse credit reporting and lawsuits. Most hospitals provide free care for patients with the most limited means as defined by income below 200% of the federal poverty limit. In the event of an unpaid bill, the Internal Revenue Service has prescribed an extensive series of steps and wait times that most hospitals must adhere to before taking any collection actions, which is a last resort.
Hospitals’ doors are always open to anyone who needs care, regardless of ability to pay. In total, hospitals and health systems of all types provided in 2020 more than $42 billion in uncompensated care, or care for which they received no payment.
Hospitals and health systems will continue to work to advance solutions that make care more affordable and accessible for all patients. But health plans must do their part by providing adequate coverage that does not subject patients to unaffordable bills and medical debt.
It’s time to protect patients from short-term health plans
https://www.lls.org/advocate/protecting-patients-junk-insurance
Leukemia Lymphoma Society (LLS) supports actions that regulate or prohibit “junk insurance” plans that discriminate against people with pre-existing conditions, offer no meaningful coverage in the case of a cancer diagnosis or neglect to cover essential healthcare services like prescription drugs
The problem
LLS advocate Sam Bloechl thought he was doing everything right. After experiencing back pain that wouldn’t go away, he spoke to an insurance broker about upgrading his insurance plan to better cover any treatment he might need. Sam’s broker insisted she had the perfect plan for him. It wasn’t.
A month later, Sam was diagnosed with non-Hodgkin lymphoma. After chemotherapy and radiation, Sam achieved remission. But his health plan refused to cover the bill, leaving Sam with more than $800,000 in medical debt. It turns out he was sold a short-term, limited-duration plan—a type of “junk insurance.”
Sam isn’t alone. Patients with pre-existing conditions are penalized by low-quality policies, known as “junk insurance” Because such plans are exempt from important consumer protections, they can leave patients vulnerable when they most need timely access to quality, affordable care.
The patient impact
Most short-term, limited-duration plans leave patients on the hook for thousands of dollars if they face serious health problems—much more than they’d face if they had traditional health insurance, a recent Milliman study funded by LLS reveals. The plans often rely on misleading marketing and are misunderstood by consumers who buy them. And patients have no right to appeal plan decisions.
Moreover, junk plans drive up more than a patient’s out-of-pocket costs—they threaten prices across the health insurance market. As younger and healthier individuals choose these cheaper “junk plans” over comprehensive insurance, premiums for comprehensive insurance are expected to rise.
Solutions
LLS supports actions that regulate or prohibit “junk insurance” plans that discriminate against people with pre-existing conditions, offer no meaningful coverage in the case of a cancer diagnosis or neglect to cover essential healthcare services like prescription drugs. These plans include:
• Short-term, limited-duration insurance
• Health care sharing ministries
• Farm Bureau plans
• Grandfathered plans
• Multiple employer welfare arrangements and association health plans
• Spurious single-employer self-insured group health plans
• Minimum essential coverage-only plans
• Excepted benefit plans
A report published by 30 patient organizations, including LLS, explains these types of plans in depth—and details how state and federal lawmakers can help protect patients and consumers from these dangerous plans.
LLS works to stop policy proposals that would allow insurers to reinstitute lifetime limits, eliminate the current cap on patient cost-sharing and cover fewer essential services for cancer patients.
Too Many Kids are Uninsured or Underinsured in the US

Access to healthcare in childhood has long term effects on health outcomes, but many children in the US are either uninsured or underinsured, meaning they often don’t have access to the care they need. Why is that and what can we do about it?
Cartoon – Skinny Health Plan Coverage



