Over the last few years, I have written for the Rockefeller Institute about trends in healthcare. In 2023, I chose ten trends, including staffing challenges, the increasing role of non-traditional players in health, such as Walmart and CVS, as well as the increasing role of private equity in healthcare, the movement toward value-based care, and the growing use of digital health—all trends that I expect to continue. In 2024, I highlighted a mega trend specific to the provider community, in which a number of factors had combined to lead to the segmentation of the industry into three different categories of entities. Those included what I categorized broadly as “today” entities (i.e., those that we know as traditional providers, many of whom are fighting for their sustainability), “tomorrow” entities (i.e., non-traditional entities that are not necessarily healthcare entities but are in the healthcare space and are typically part of a larger conglomerate or backed with private equity), and “striving survivors” (i.e., today entities that are adapting radically or partnering with tomorrow entities to exist in the future).
The following January, I picked five issues to watch in healthcare in 2025. They were (1) the continued expansion of computational data technologies, especially artificial intelligence (AI); (2) insurance coverage shifts; (3) consolidation in the overall industry; (4) payment, costs, and coverage for pharmaceuticals; and (5) exponential advancements in life sciences.
This blog reviews the status of those 2025 trends and suggests one additional issue that may garner more attention in 2026: the overall cost, pricing, and affordability of healthcare. I discuss the factors pushing this issue into the spotlight and potential options for policymakers to counteract this trend.
A Status Review of the Five 2025 Trends
Before delving into the newly highlighted trend of the cost, price, and affordability of healthcare, it is worth briefly reviewing the status of the five trends that were identified in 2025, since all of them will continue to be important in 2026.
- The continued expansion of computational data technologies, especially AIIssue Updates. There has been no slowdown in the use of computational data technologies and AI in healthcare since I wrote about it in 2023, and as part of the trends last year. In April 2025, the healthcare AI company Innovacer did a survey of AI use in the sector. The company’s report noted that adoption of AI is expected to continue its growth as more tools become available for a variety of purposes, including quicker and more effective disease diagnosis, administrative process improvement, and electronic health record management. JP Morgan likewise reported in December 2025 that AI-focused deals now make up 75% of health tech funding. Some of the more interesting areas of advancement are in genomics, remote patient monitoring, medical imaging, and improved documentation. And the use of ambient products that help capture health data from conversation saw some of the biggest growth yet in 2025. On the consumer side, more and more patients (an estimated 40 million people) are using chatbots to help them with making decisions about their own care, while the integration of AI with robotics is increasingly being used to assist physicians with surgery. And very recently, in January 2026, OpenAI released a chatbot specifically for health care.Policy Responses and Options. In terms of policy, there have been different federal actions designed to accelerate AI adoption and use, including a handful of executive orders in 2025. In healthcare specifically, the Department of Health and Human Services issued its AI strategy on December 5, 2025. And there have been federal investments announced that support the use of AI to advance research and cancer treatment. In addition, on December 19, 2025, the Trump administration asked for public input on how technology adoption in healthcare—especially AI—could be accelerated. At the state level over the last year, 47 states issued more than 250 bills to regulate AI in healthcare (with at least 30 bills signed into law). The bills ranged from ones protecting minors from mental health AI-enabled chatbots to bills barring AI from making therapeutic decisions or interacting with patients without licensed oversight. And states like New York are incentivizing more use of AI in healthcare through the use of partners that improve care and strengthen operations, as well as evaluating best-in-class AI tools.
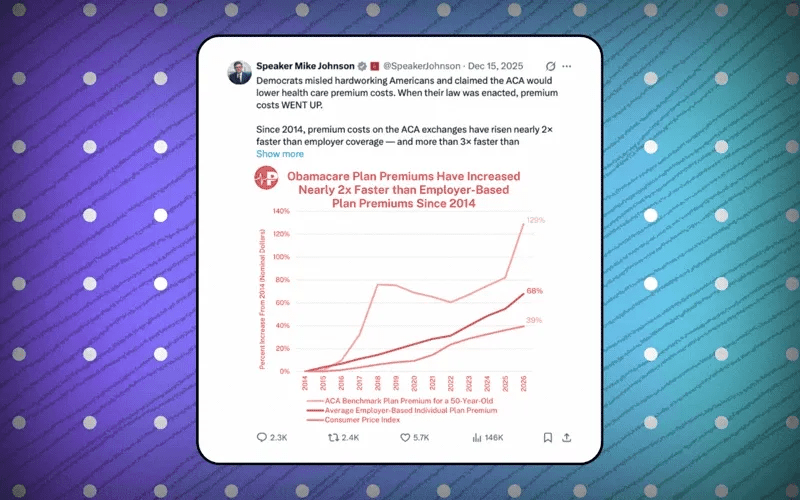
- Insurance coverage shifts Issue Updates. In January 2025, I noted the possibility that insurance coverage was likely to shift, in part, because of the possible expiration of the Enhanced Premium Tax Credits (EPTCs) at the end of 2025. The EPTCs were enhanced in 2021 under the American Rescue Plan Act and are sometimes referred to as the “Obamacare subsidies.” They were intended to reduce the cost that people pay when they obtain coverage from qualified health plans on the health exchanges. Although some proposals were made by both Democrats and Republicans at the end of 2025 to help mitigate the impact of the loss of the EPTCs, none of the proposals were able to gain enough bipartisan support to be signed into legislation in 2025, resulting in a spike in costs for premiums starting January 1, 2026. As this blog was being written, Congress was debating the possible partial extension of these credits in some form, although passage was not certain. Either way, it is likely that healthcare coverage will continue to be a topic of much debate in Congress in 2026.In addition, in 2025, changes made to Medicaid coverage in the One Big Beautiful Bill Act (otherwise known as HR1) are also likely to impact insurance costs and coverage in 2026. The changes to health insurance coverage in HR1 were outlined in a paper by the Institute in mid-2025 and will have varying impacts on both funding and coverage over the coming months and years. As I later wrote about with colleagues, additional federal rule changes in 2025 will also impact public insurance coverage in the future. The Urban Institute estimates that close to five million people may lose coverage in 2026, although the exact number who lose coverage versus those who choose cheaper and less expansive coverage options with fewer benefits has yet to be fully analyzed.Policy Responses and Options. With the expiration of the EPTCs and changes in federal reimbursement for coverage of immigrant populations, state policymakers will need to make decisions in 2026 about who and what may be covered with state-only dollars. States appear to be taking different approaches. By mid-2025, the Kaiser Family Foundation reported that of the 14 states that offer health coverage to at least some immigrants, at least three had proposed limits on coverage (some ending it altogether and others restricting it). For example, on January 1, 2026, Medi-Cal, which is California’s Medicaid program, will freeze any new enrollments for certain undocumented adults who receive state-funded full-scope services. In June 2025, the Minnesota legislature voted to limit eligibility for persons over age 18 who are undocumented. New York has applied to federal regulators seeking to change the authorization for its successful Essential Plan—that provides coverage to some 1.7 million New Yorkers, including certain legally present immigrants—from a revocable federal waiver to the Affordable Care Act (ACA) specified Basic Health Program. Expect to see many other states taking actions to either drop or preserve health insurance coverage in 2026. What impact these changes have on the extent of coverage and the number of newly uninsured people this year remains to be seen.
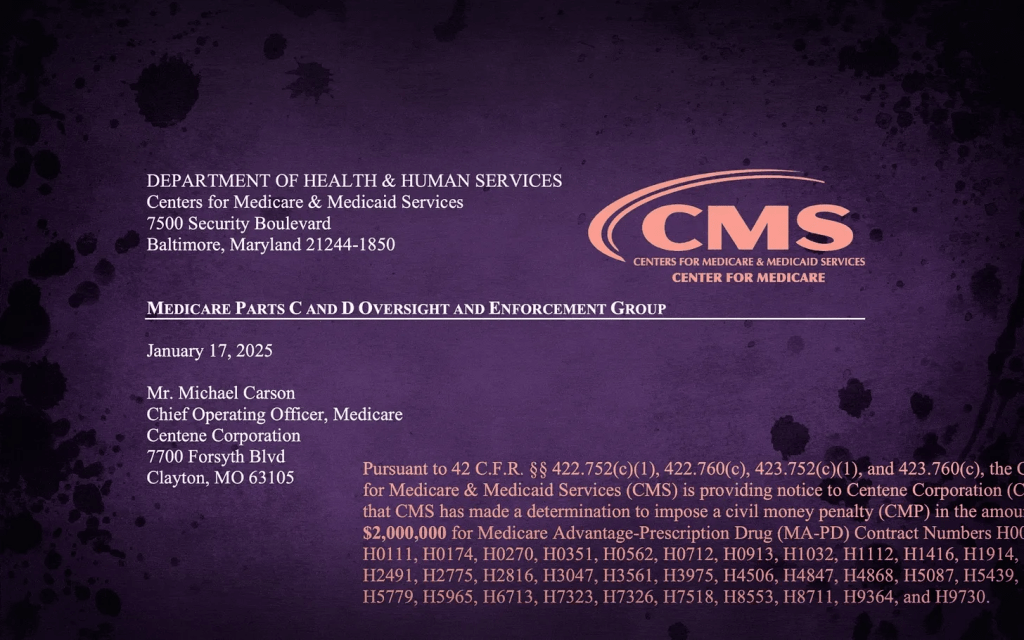
- Consolidation in the overall industry Issue Updates. Consolidations in healthcare, both vertical and horizontal, continue. In January 2025, we highlighted mergers, such as the one that created Risant Health. We also examined the continued integration of various companies with United Health Group under Optum Rx (a pharmacy business), Optum Insight (a health analytics company), and Optum Health (care management), as well as the integration of United Health Group and Change Healthcare in early 2024. The consolidation of the insurance industry continued in 2025, with the top 7 companies garnering 75% of the market. The Government Accountability Office also reported on the continued acquisition of physician groups by insurers, hospitals, and private equity firms. Overall, mergers and acquisitions (M&A) transactions among healthcare entities increased steadily from 2021-2024, and, in 2025, healthcare M&A was experiencing its most active M&A cycle in over a decade. Full-year trends were not yet fully assessed by the time of printing this blog, but Pitchbook, which tracks M&A deals across industries, expected that healthcare services M&A levels in 2025 would slightly exceed 2024 levels. This also includes the divestiture of assets from national chains like Ascension and CommonSpirit Health.Policy Responses and Options. At the federal level, shortly after last year’s blog on this trend was published, the federal HHS released a report on how consolidation in the industry continues. For the most part, the Trump administration has kept in place stricter guidelines for reviewing corporate mergers in healthcare, but that hasn’t stopped consolidation from happening. At the state level, we previously highlighted that state policymakers had proposed over 34 bills in 22 states designed to address such consolidations. As this blog was being written, the governor of New York indicated in her State of the State speech that the state planned to expand its monitoring of transactions by healthcare entities that increase revenues by over $25 million. Yet, market forces seem to be allowing such consolidations to continue, and financial and operational strains allow the continuation of mergers and acquisitions that are forcing some systems to divest in hospitals, while regional systems acquire those smaller assets that enable them to expand. Unless states can play a role in propping up financially challenged providers, prevent large insurers from becoming larger, or better regulate nontraditional actors in healthcare, consolidation appears likely to continue in the coming year.
- Payment, costs, and coverage for pharmaceuticals Issue Updates. By late 2025, it was reported that pharmaceutical companies were expected to raise prices on at least 350 drugs in 2026. That is higher than at the same time last year. Generally, many of the regulatory actions to control prices come from the federal level. Although states may feel somewhat constrained by the Commerce Clause on their ability to regulate pharmaceuticals across state lines, there are still ways for them to address cost issues, such as through rebate programs, limits on Pharmacy Benefit Managers (PBMs), or price negotiations for drugs purchased under the Medicaid program or for state employee benefit programs.Policy Responses and Options. At the federal level, the Trump administration issued an executive order in the spring of 2025 with suggested actions to lower drug prices. The administration also announced agreements to lower the cost of two of the most used drugs in the country, Ozempic and Wegovy. Then, at the end of 2025, the Centers for Medicare and Medicaid Innovation (CMMI) released a proposed model for controlling prescription costs called the Global Benchmark for Efficient Drug Pricing (GLOBE) Model, which is a mandatory model that would assess a rebate for certain drugs under Medicare Part B if the prices exceed those paid in economically comparable countries. It also released the Guarding US Medicare Against Drug Costs (GUARD) Model, which calculates international reference pricing benchmarks and requires manufacturers to pay a rebate if the Medicare net price is greater than the Model benchmark. Congress introduced bipartisan legislation in mid-2025 to lower drug prices by barring drug companies in the US from charging higher prices. State governments were also very active in 2025, passing legislation to lower drug prices, with 31 states passing nearly 70 bills by the end of the third quarter with the goal of lowering prices. I expect to see additional legislation in more states in 2026, including state efforts that mirror some of the federal actions that took place in 2025. As mentioned, such efforts might include building on existing state efforts, such as drug review boards, expanded rebates under Medicaid, and/or reducing administrative costs through third parties, like PBMs.
- Exponential advancements in life sciences Issue Updates. Although AI has transformed medicine in different ways, in the case of life sciences, AI accelerated advancements especially for genomics, precision medicine, and medical imaging. In particular, as noted by MedEdge, life science based medicine like gene editing and CRISPR were better able to move out of the trial phase and into the treatment phase. AI is also augmenting drug discovery by making it easier to observe the interaction of drugs and understand how they fight disease. Molecular editing, lab-grown 3D bioprinting, mRNA vaccine use for cancer, and robotic surgery are all areas that MedEdge saw continued expansion in 2025. Private funding continued to pour into biotechnology in 2025, as tracked by Fierce Healthcare. The Fierce Healthcare tracker shows that many companies, such as Hemab Therapeutics, Electra Therapeutics, or Tubulis (an antibody drug conjugate), raised well over $100 million in venture capital and related funding in 2025.Policy Responses and Options. In contrast to the growing investments of private funding in life sciences, funding from the federal government specifically for life science research—especially from the NIH—was targeted for cuts in 2025 with disproportionate impacts across states depending on where that research was occurring. According to tracking done by The Sciences & Community Impacts Mapping Project, proposed federal funding cuts showed a potential economic loss of an estimated $16 billion. At the state level, policymakers in the Midwest, California, North Carolina, and a few other states are competing to advance major life sciences projects. The investments include supporting the workforce, developing shovel-ready sites or ones adjacent to major universities, and/or providing expedited permitting. Given the growing advancements and potential of life sciences, in the coming year, I expect to see state policymakers implementing more policy strategies that help grow the life sciences sector in their respective states under both the auspices of life sciences and economic development.
- An additional trend to watch in 2026Issue Background. Of the trends I noted in 2025, only one (efforts to control the costs of pharmaceuticals) is specifically targeted at addressing the cost and affordability of healthcare. The impact of the actions of state and federal policymakers to improve the affordability of drugs, however, does not seem to be enough yet to curb the overall cost growth in the industry. In fact, of the other trends noted in 2025, some might even be considered cost drivers. For example, mergers and acquisitions and overall consolidation can at times increase costs in some markets, depending on what those mergers include, and for some healthcare consumers who rely on insurance coverage, the loss of the subsidies to pay for healthcare makes that cost increase much more apparent. Although there is some optimism that AI, through process improvement, quicker diagnostics, and disease prevention, could make certain things more efficient, so far, there are mixed results as to whether AI is making healthcare more affordable. With costs for other basic necessities like housing being less affordable, the focus on healthcare affordability is likely to continue in 2026. This is because some consumers will more directly feel the cost of healthcare in 2026, but also because providers have experienced increasing challenges with expenses that contribute to affordability. Examples of areas of expense growth cited by providers include staffing and benefits, supplies, pharmacy, and technology.Industry Responses and Options. Although I previously noted the policy responses of federal and state governments as they relate to these trends, in the case of lowering costs, industry is also responding in new and creative ways. One of the new ways that health systems and providers are attempting to tackle rising prices and costs is through non-traditional partnerships that deliver care, treatments, and services more directly to patients. An example of this is a potential partnership between Humana, an insurance company, and Mark Cuban, co-founder of Cost Plus Drugs. The potential partnership would focus on direct-to-employer programs that cut out companies in the middle, such as PBMs. Another example was the launch of Northwell Direct, a provider system offering direct care to employers without an insurance company. This arrangement is the largest of its kind and recently added a partnership with the influential 32BJ Health Fund, which allows 170,000 participants in the 32BJ Health Fund in the general Northwell service area to have access to the full spectrum of health care services available through Northwell Direct, which is expected to produce significant administrative savings.Policy Responses and Options. One way government policy makers at both the federal and state levels can respond to the affordability crisis is to allow the industry itself to find creative solutions, such as those outlined above. A second way policymakers can respond is by using the authority granted under the ACA for the CMMI to create and experiment with new models of care delivery that could improve care and lower costs. In 2025, CMMI issued at least 6 new payment models, all designed to lower the costs of healthcare. They include some of the ones mentioned above on pharmaceutical cost control, like the GUARD and GLOBE models, but also ones specifically targeting chronic disease, such as the Advancing Chronic Care with Effective Scalable Solutions (ACCESS model), and healthier lifestyles, for example, the Better Approaches to Lifestyle and Nutrition for Comprehensive Health (BALANCE model).
Meanwhile, state governments and officials are proposing various ways to control costs, with over 750 related bills introduced in 2024 alone. Some states are more focused on particular strategies, such as pricing—including hospitals with reference-based pricing. In Indiana, the legislature passed a bill that does not allow hospital systems to exceed prices set before January 1, 2025, for two years. The hospitals would then have to lower prices by a certain percentage each year to reach a goal set by the state’s Office of Management and Budget. For several years now, states have been implementing price transparency policies with the aim of reducing costs. It is, of course, possible that some states will use a combination of these efforts (e.g., promoting industry-initiated efforts through incentives or less regulation to lower costs while also more closely monitoring prices).
Conclusion
The six trends to watch in 2026 noted in this blog are by no means all-encompassing, but they do highlight areas that are likely to garner a lot of attention from policymakers in the near term. As has been true throughout the country’s history, the Federalist system of government allows state and federal governments to develop varied policy approaches to improve how healthcare is funded and delivered. The Rockefeller Institute will be tracking these six trends and will report on any interesting findings, particularly as they relate to the additional trend of the cost and affordability of care in the coming year.