https://www.yahoo.com/news/united-states-pandemic-phase-fauci-094908627.html

The United States is finally “out of the pandemic phase,” the country’s top infectious disease expert said, as cases and hospitalizations are notably down and mask mandates are all but extinct.
While there are still new infections spreading throughout the country – an average of 50,000 per day as of Tuesday – the country is far from the heights of the pandemic, when daily case counts surpassed 1 million. Restrictions, too, are easing as many Americans appear to be putting the pandemic behind them. Masking requirements have been lifted across most of the country, and officials stopped enforcing a federal mask mandate in transportation settings after a judge struck down the requirement.
“We are certainly right now in this country out of the pandemic phase,” Anthony Fauci, President Joe Biden’s chief medical adviser, said Tuesday evening on PBS’s “NewsHour.”
Fauci said the United States was no longer seeing “tens and tens and tens of thousands of hospitalizations and thousands of deaths. We are at a low level right now.”
During the pandemic’s darkest moments, many wondered when the country would officially declare itself past the nationwide disaster, which has killed nearly 1 million Americans.
Fauci’s comments are likely to fuel debate about whether this is truly the moment: New cases are on the rise in the United States, and deaths are down, though they often lag spikes in cases. The Centers for Disease Control and Prevention said Tuesday that as of the end of February, nearly 60 percent of Americans – including three out of every four children – have been infected with the coronavirus. But officials cautioned that the data did not indicate that Americans have widespread immunity against the virus because of their prior infections.
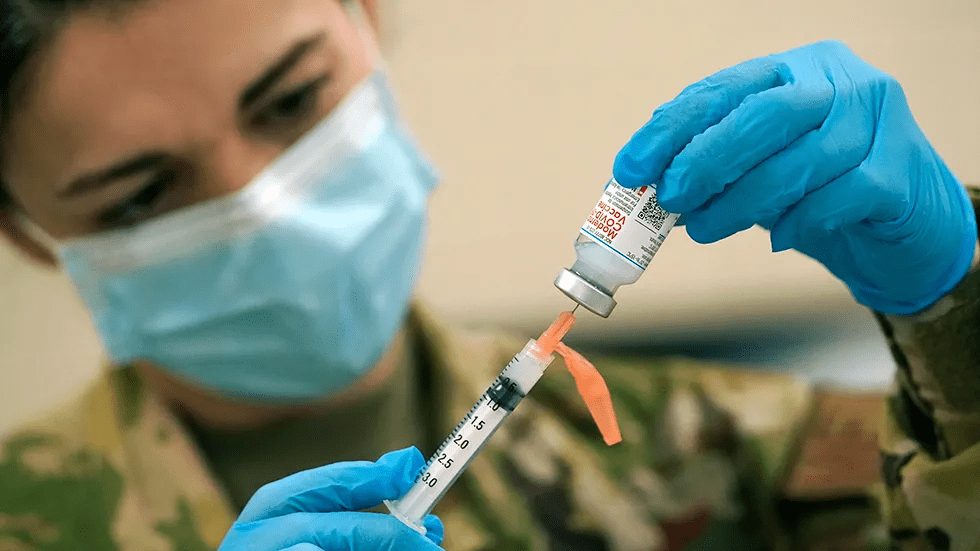
While previous infections are believed to offer some protection against serious disease for most people, health experts say the best protection against infection and serious disease or death from the coronavirus is vaccination.
The coronavirus will not be eradicated, Fauci said, but can be handled if its level of spread is kept “very low” and people are “intermittently” vaccinated, though he said he did not know how frequently. And Fauci echoed warnings from the World Health Organization and the United Nations this month that worldwide, the pandemic is far from over as vaccinations lag, particularly in developing nations.
The Biden administration, meanwhile, is appealing a ruling by a Trump-appointed federal judge that struck down the federal mask mandate on transit, including on planes, though it is unclear whether they will be successful, and likely face an American public that could be unwilling to comply again.
And in a less-than-subtle reminder that the coronavirus is still hanging around, the White House on Tuesday announced arguably the nation’s highest-profile coronavirus infection since former president Donald Trump, saying that Vice President Kamala Harris had tested positive and was asymptomatic. She was not considered in close contact to Biden, the White House said.