President Joe Biden last night highlighted several healthcare priorities during his State of the Union address, including efforts to reduce drug costs, a universal cap on insulin prices, healthcare coverage, and more.
COVID-19
In his speech, Biden acknowledged the progress the country has made with COVID-19 over the last few years.
“Two years ago, COVID had shut down our businesses, closed our schools, and robbed us of so much,” he said. “Today, COVID no longer controls our lives.”
Although Biden noted that the COVID-19 public health emergency (PHE) will come to an end soon, he said the country should remain vigilant and called for more funds from Congress to “monitor dozens of variants and support new vaccines and treatments.”
The Inflation Reduction Act
Biden highlighted several provisions of the Inflation Reduction Act (IRA), which passed last year, that aim to reduce healthcare costs for millions of Americans.
“You know, we pay more for prescription drugs than any major country on earth,” he said. “Big Pharma has been unfairly charging people hundreds of dollars — and making record profits.”
Under the IRA, Medicare is now allowed to negotiate the prices of certain prescription drugs, and out-of-pocket drug costs for Medicare beneficiaries are capped at $2,000 per year. Insulin costs for Medicare beneficiaries are also capped at $35 a month.
“Bringing down prescription drug costs doesn’t just save seniors money,” Biden said. “It will cut the federal deficit, saving tax payers hundreds of billions of dollars on the prescription drugs the government buys for Medicare.”
Caps on insulin costs for all Americans
Although the IRA limits costs for seniors on Medicare, Biden called for the policy to be made universal for all Americans. According to a 2022 study, over 1.3 million Americans skip, delay purchasing, or ration their insulin supply due to costs.
“[T]here are millions of other Americans who are not on Medicare, including 200,000 young people with Type I diabetes who need insulin to save their lives,” Biden said. “… Let’s cap the cost of insulin at $35 a month for every American who needs it.”
With the end of the COVID-19 PHE, HHS estimates that around 15 million people will lose health benefits as states begin the process to redetermine eligibility.
The opioid crisis
Biden also addressed the ongoing opioid crisis in the United States and noted the impact of fentanyl, in particular.
“Fentanyl is killing more than 70,000 Americans a year,” he said. “Let’s launch a major surge to stop fentanyl production, sale, and trafficking, with more drug detection machines to inspect cargo and stop pills and powder at the border.”
He also highlighted efforts by to expand access to effective opioid treatments. According to a White House fact sheet, some initiatives include expanding access to naloxone and other harm reduction interventions at public health departments, removing barriers to prescribing treatments for opioid addiction, and allowing buprenorphine and methadone to be prescribed through telehealth.
Access to abortion
In his speech, Biden called on Congress to “restore” abortion rights after the U.S. Supreme Court overturned Roe v. Wade last year.
“The Vice President and I are doing everything we can to protect access to reproductive healthcare and safeguard patient privacy. But already, more than a dozen states are enforcing extreme abortion bans,” Biden said.
He also added that he will veto a national abortion ban if it happens to pass through Congress.
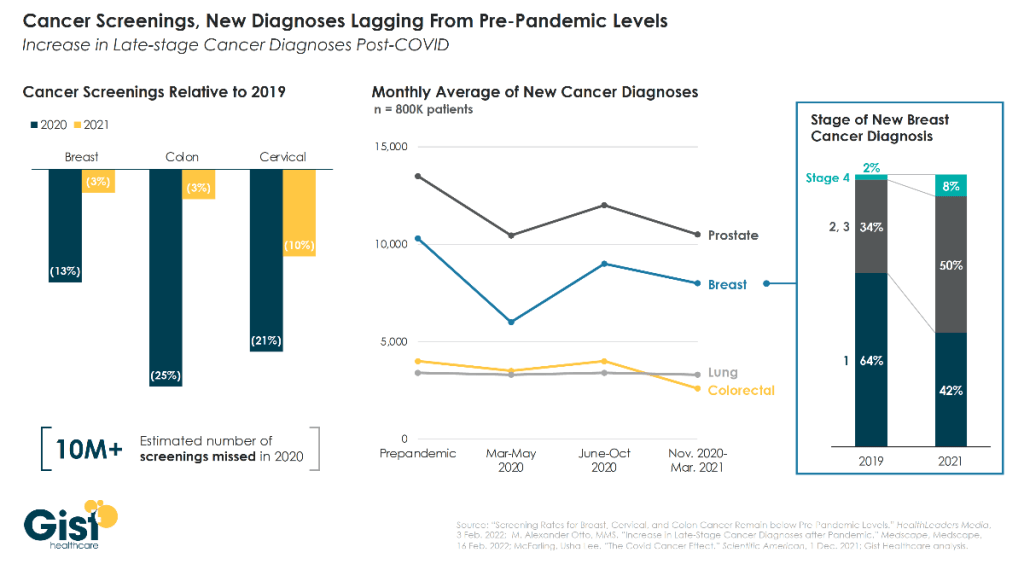
Progress on cancer
Biden also highlighted the Cancer Moonshot, an initiative launched last year aimed at advancing cancer treatment and prevention.
“Our goal is to cut the cancer death rate by at least 50% over the next 25 years,” Biden said. “Turn more cancers from death sentences into treatable diseases. And provide more support for patients and families.”
According to a White House fact sheet, the Cancer Moonshot has created almost 30 new federal programs, policies, and resources to help increase screening rates, reduce preventable cancers, support patients and caregivers and more.
“For the lives we can save and for the lives we have lost, let this be a truly American moment that rallies the country and the world together and proves that we can do big things,” Biden said. “… Let’s end cancer as we know it and cure some cancers once and for all.”
Healthcare coverage
Biden commended the fact that “more American have health insurance now than ever in history,” noting that 16 million people signed up for plans in the Affordable Care Act marketplace this past enrollment period.
In addition, Biden noted that a law he signed last year helped millions of Americans save $800 a year on their health insurance premiums. Currently, this benefit will only run through 2025, but Biden said that we should “make those savings permanent, and expand coverage to those left off Medicaid.”
Advisory Board’s take
Our questions about the Medicaid cliff
President Biden extolled economic optimism in the State of the Union address, touting the lowest unemployment rate in five decades. With job creation on the rise following the incredible job losses at the beginning of the COVID-19 pandemic, there is still a question of whether the economy will continue to work for those who face losing Medicaid coverage at some point in the next year.
The public health emergency (PHE) is scheduled to end on May 11. During the PHE, millions of Americans were forced into Medicaid enrollment because of job losses. Federal legislation prevented those new enrollees from losing medical insurance. As a result, the percentage of uninsured Americans remained around 8%. The safety net worked.
Starting April 1, state Medicaid plans will begin to end coverage for those who are no longer eligible. We call that the Medicaid Cliff, although operationally, it will look more like a landslide. Currently, state Medicaid regulators and health plans are still trying to figure out exactly how to manage the administrative burden of processing millions of financial eligibility records. The likely outcome is that Medicaid rolls will decrease exponentially over the course of six months to a year as eligibility is redetermined on a rolling basis.
In the marketplace, there is a false presumption that all 15 million Medicaid members will seamlessly transition to commercial or exchange health plans. However, families with a single head of household, women with children under the age of six, and families in both very rural and impoverished urban areas will be less likely to have access to commercial insurance or be able to afford federal exchange plans. Low unemployment and higher wages could put these families in the position of making too much to qualify for Medicaid, but still not making enough to afford the health plans offered by their employers (if their employer offers health insurance). Even with the expansion of Medicaid and exchange subsidies, it, is possible that the rate of uninsured families could rise.
For providers, this means the payer mix in their market will likely not return to the pre-pandemic levels. For managed care organizations with state Medicaid contracts, a loss of members means a loss of revenue. A loss of Medicaid revenue could have a negative impact on programs built to address health equity and social determinants of health (SDOH), which will ultimately impact public health indicators.
For those of us who have worked in the public health and Medicaid space, the pandemic exposed the cracks in the healthcare ecosystem to a broader audience. Discussions regarding how to address SDOH, health equity, and behavioral health gaps are now critical, commonplace components of strategic business planning for all stakeholders across our industry’s infrastructure.
But what happens when Medicaid enrollment drops, and revenues decrease? Will these discussions creep back to the “nice to have” back burners of strategic plans?
Or will we, as an industry, finish the job?