2025 was one of the most turbulent years in modern U.S. healthcare. The headlines were explosive, the rhetoric dramatic and the controversies nonstop. Yet for all the hoopla and upheaval, the medical care Americans received this month looked almost identical to what they experienced on January 1 — except more expensive.
That yearlong pattern (of intense disruption followed by little improvement) played out across nearly every major healthcare storyline.
Luigi Mangioli is preparing to stand trial almost exactly twelve months after the fatal shooting of UnitedHealth CEO Brian Thompson. The killing sparked fears for major health insurers and raised questions about the fragility of the nation’s largest payer. In a February article, I called it a defining moment for UnitedHealth: an opportunity for the company to start competing on health, not denials. But despite the initial shock and ongoing scrutiny, nothing has shifted in how UnitedHealth pays for (or denies) medical care.
Then, in late fall, the nation endured the longest government closure in U.S. history, driven largely by conflicts over healthcare spending and the Affordable Care Act’s health exchanges. However, the eventual resolution to reopen the government came with no respite for the 24 million Americans currently enrolled in an exchange.
For a broader view of the year, here are five major areas of healthcare that generated chaos, confusion and conflict in 2025 – but little meaningful improvement.
1. Political chaos: Turning science into a battleground
No aspect of healthcare saw more volatility in 2025 than in the political arena. The tone was set in January when President Trump returned to office and began reshaping federal health agencies with unprecedented speed.
Within days, he issued a record flurry of executive orders targeting the Affordable Care Act, Medicaid waivers, Medicare Advantage oversight, prior-authorization rules and federal nutrition standards.
He replaced long-entrenched leaders at HHS, NIH, CDC and FDA with political outsiders, many of whose views on vaccines, chronic disease and scientific evidence diverged sharply from the career experts they superseded. The nomination of RFK Jr. to lead HHS became a flashpoint. His reluctance to confront the measles outbreak in Texas, combined with mixed messaging on vaccine policy, have deepened concern for public health.
The result has been rapid turnover of expert clinicians and a revolving door of leaders in the FDA, CDC and NIH. Senior scientists continue to resign, key programs remain stalled and career staff report growing political interference in decisions that previously rested on data and expert consensus.
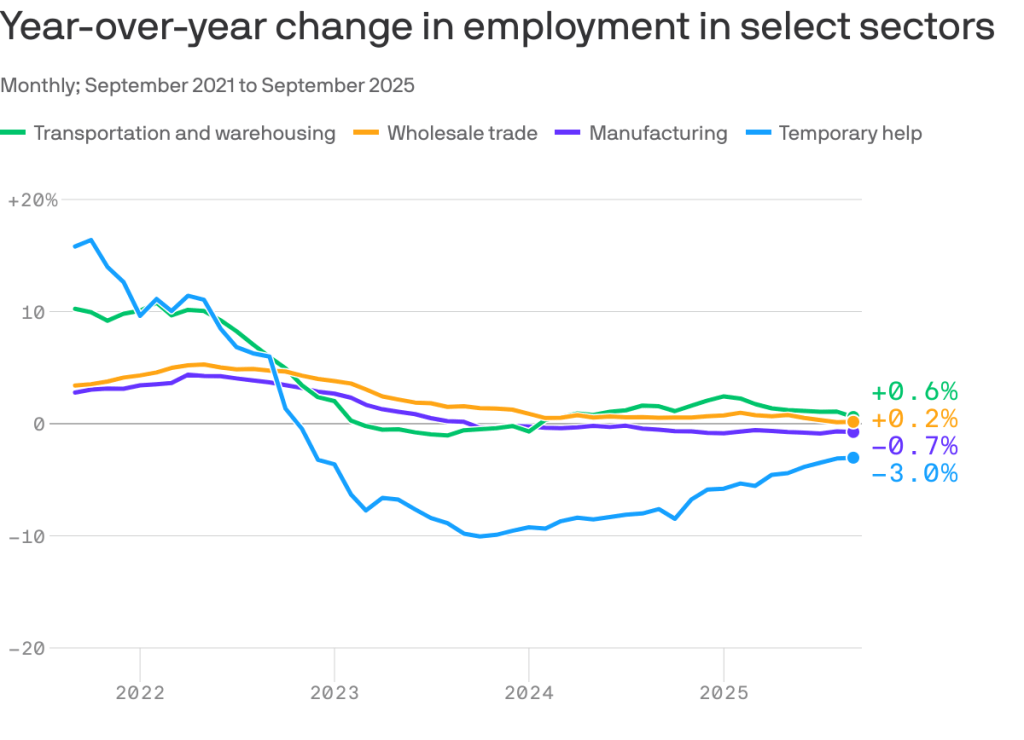
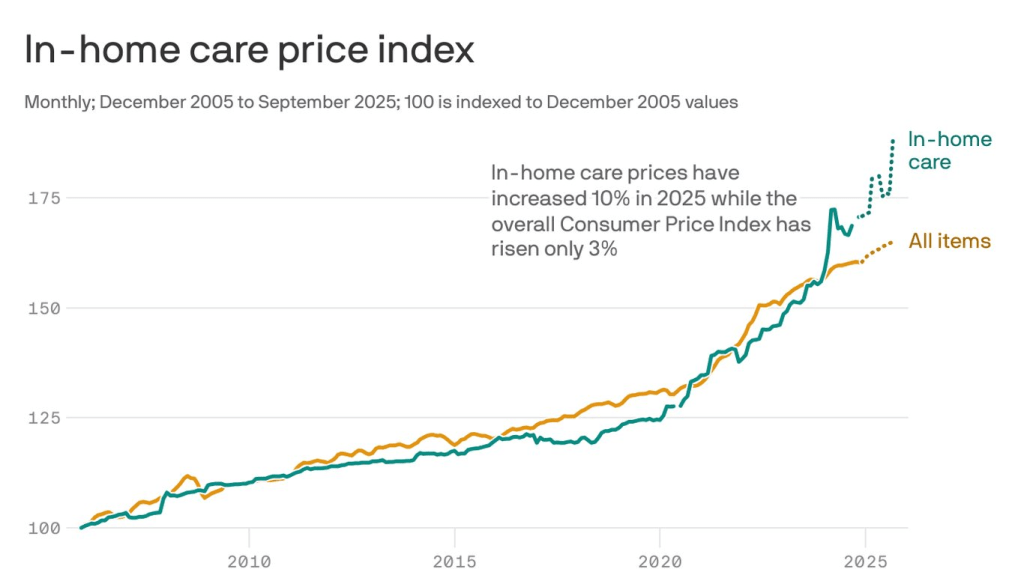
2. Economic crisis: Costs soar as coverage grew more fragile
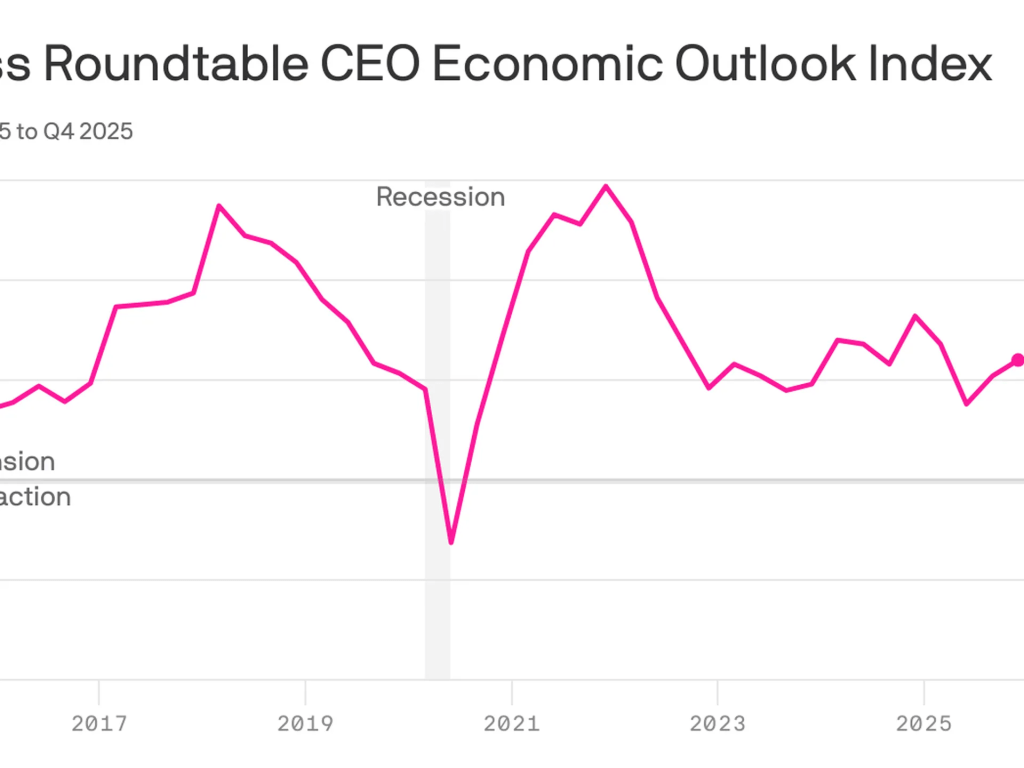
Beneath the political theatrics of 2025 was a sobering reality: Americans will once again pay far more for healthcare next year than the year before. And for many, the financial protections that once softened those increases are disappearing.
Insurers on the Affordable Care Act (ACA) marketplace requested median premium hikes of 18% for 2026, the steepest jump since 2018 and well above this year’s 7% hike. If Congress fails to extend the enhanced ACA subsidies, families who once paid affordable monthly premiums will see their costs double or even triple.
The broader economic picture makes these pressures unavoidable. The United States is now spending $5.6 trillion annually on healthcare. National health expenditures are projected to climb another 7.1% this year, far outpacing economic growth. At the same time, federal debt service continues to soar, consuming more of the national budget than Medicaid itself.
The result is an economic crisis hiding in plain sight, one that will increasingly strain the financial, physical and mental health of Americans in the year to come.
3. Regulatory confusion: Agencies rebooted but didn’t improve health
This year shook the foundations of America’s public-health architecture and left yawning gaps where trust, clarity and expert oversight once stood. Politics has replaced science as the primary driver of healthcare policy.
The Centers for Disease Control and Prevention lost its director just weeks after her confirmation. Within days, top-level scientists and center heads resigned en masse, citing political interference and a collapse of scientific independence. Months later, there still is no permanent CDC head.
At the Food and Drug Administration, career reviewers say they’ve been forced to reconsider or abandon scientific best practices. Across both the CDC and FDA, advisory committees that once evaluated evidence through rigorous, peer-driven processes now rely on anecdote and ideology. One striking example is the FDA’s decision to stop requiring hepatitis B vaccination at birth, a move that public-health experts warn could lead to tens of thousands of additional infections for a disease that had been reduced to fewer than 20 annual cases.
Meanwhile, the administration’s sweeping “health-freedom agenda” (under the banner Make America Healthy Again) has identified food packaging, additives, school-lunch standards and “ultra-processed” diets as public-health priorities. But the proposals to improve nutrition remain largely unformed, as the likelihood of meaningful improvements fade.
What remains at year’s end is a set of agencies still functioning, but with public trust weakened and no clear path to rebuilding it.
4. Technological contradiction: AI leapt ahead while medicine stood still
No field generated more excitement, or exposed more contradictions, in 2025 than generative artificial intelligence.
In the broader economy, GenAI models transformed finance, logistics, law, retail and customer service. New large language models, including GPT-5, DeepSeek and Gemini 3, demonstrated near-expert performance on clinical reasoning, interpretation of complex symptoms and risk prediction. Ambient listening matured into a reliable documentation tool, and with the emergence of Artificial General Intelligence (AGI), Americans are relying on large language models when they have medical questions.
Yet inside traditional medicine, progress remains stalled. Clinicians continue to be encouraged to use AI for administrative shortcuts (coding, charting, prior authorization claims) but national specialty organizations haven’t pushed them to use GenAI for diagnosing disease, reducing medical errors or improving clinical outcomes.
Fear of liability has discouraged technology companies from offering GenAI tools that would allow patients to evaluate symptoms or manage their chronic diseases. Yet usage continues to grow. In polling I conducted this fall, 77% of patients and 63% of healthcare professionals reported using a generative-AI tool in the past three months for health-related information or decision support. Meanwhile, medical schools still teach pre-AI workflows, even as medical students and residents turn to GenAI for clinical knowledge and case analysis. The divide between institutional practice and the behaviors of patients and the next generation of physicians is expanding at an accelerating pace.
5. Cultural conflict: A growing divide between the public & the profession
If 2025 revealed anything about American healthcare, it was a widening cultural rift: between younger patients and medical professionals, and between science and public belief.
This rift is felt particularly among Gen Z and Millennials, generations that grew up online, accustomed to second-screen verification and skeptical of traditional authority. As I wrote in 3 Ways Doctors Can Win Back Gen Z And Millennial Patients, younger Americans expect shared decision-making, transparency and digital-first convenience — expectations medicine failed to fulfill in 2025.
At the same time, disinformation and political rhetoric seeped deeper into public life. Social media spread half-truths faster than public-health leaders could correct them. Vaccine skepticism rose thanks to political disinformation. Basic nutritional science became partisan, too. And the public’s confusion only intensified.
What 2025 reveals about the road ahead
By year’s end, one truth became impossible to ignore: despite unprecedented political turmoil, economic instability, scientific breakthroughs and cultural upheaval, the basic structure of American healthcare remained unchanged.
The incentives driving the system, the chronic diseases afflicting the population and the unaffordability confronting families all persist as we enter 2026. At the same time, as generative AI transforms nearly every other sector of the economy, the fax machine remains the most common method physicians use to exchange vital medical information.
The question now is whether mounting economic, political and cultural pressures will finally force American medicine to transform care delivery next year. For more on that, follow me on Forbes and look for my next article on January 5, featuring my healthcare predictions for 2026.