Englewood, Colo.-based Catholic Health Initiatives embarked on a turnaround plan several years ago with the goal of improving its financial picture while providing high-quality care at its hospitals and other facilities across the nation. The system has made great strides toward its goal, yet there is still a lot of work to be done.
CHI has been laser-focused on performance improvement over the past three years, but rolling out a comprehensive turnaround plan across an organization with 100 hospitals is challenging, and progress is slow. The health system’s efforts just began to take hold in the second half of fiscal year 2017. Although CHI has encountered obstacles on its path to financial stability, the system is pleased with the headway it has made and expects more improvement in the coming months.
CHI’s cost-cutting initiative
To improve its finances, CHI set out to cut costs across the system. It put a great deal of energy into lowering labor and supply costs, which combined can make up two-thirds or more of the system’s operating expenses. CHI developed plans and playbooks focused on reducing these costs several years ago, knowing it would not immediately see results.
In the labor area, CHI President of Enterprise Business Lines and CFO Dean Swindle says the system had to incur costs to cut costs. “In the second half of the year [fiscal 2017] we began to see the benefits of our labor activities in the markets, but we also had cost,” he says. For example, CHI incurred the one-time expense of hiring advisers to help the system develop new labor management techniques. The system also cut jobs, which resulted in severance costs.
“When we got to the second half of 2017, we were very confident and felt very pleased that we were seeing benefit … but it was difficult for others to see it because it was for half of the year, and we had the one-time costs that were burdening that,” Mr. Swindle says.
After factoring in expenses and one-time charges, CHI ended fiscal year 2017 with an operating loss of $585.2 million, compared to an operating loss of $371.4 million in fiscal year 2016.
However, CHI saw its financial situation improve in the first quarter of fiscal year 2018. The system’s operating loss narrowed to $77.9 million from $180.7 million in the same period of the year prior. “What you were able to see in the first quarter [of fiscal 2018] … was the one-time costs had gone away for the most part; those weren’t burdening our results,” says Mr. Swindle.
He says although the system employed more physicians, its absolute labor costs were lower year over year. CHI’s supply costs, including drug costs, were also lower in the first quarter of fiscal year 2018 than in the first quarter of last year.
Mr. Swindle says CHI saw its finances improve in a difficult operating environment. Patient volume was lower in the first quarter of fiscal year 2018 than a year prior, and the system also experienced a nearly $26 million loss from business operations as a result of Hurricane Harvey.
“[This has] given us a level of confidence that we can move forward and address the difficulty that our industry is going to be facing over the next several years,” he says.
In early January, Fitch Ratings affirmed CHI’s “BBB+” rating and upgraded its credit outlook to stable from negative. The credit rating agency cited the health system’s strong start to the 2018 fiscal year and financial improvements in several markets as key reasons for the upgrade.
Preparing for new challenges
Although healthcare organizations are currently facing many challenges, including regulatory uncertainty and dwindling reimbursement rates, Mr. Swindle anticipates hospitals and health systems will face new obstacles over the next few years.
For example, hospitals will be challenged by changes to the 340B Drug Pricing Program. CMS’ 2018 Medicare Outpatient Prospective Payment System rule finalized a proposal to pay hospitals 22.5 percent less than the average sales price for drugs purchased through the 340B program. Medicare previously paid the average sales price plus 6 percent.
“I don’t think 340B was by chance and in isolation,” says Mr. Swindle. “I think we’re entering one of those cycles that the whole economic environment of our industry is going to be working against us.”
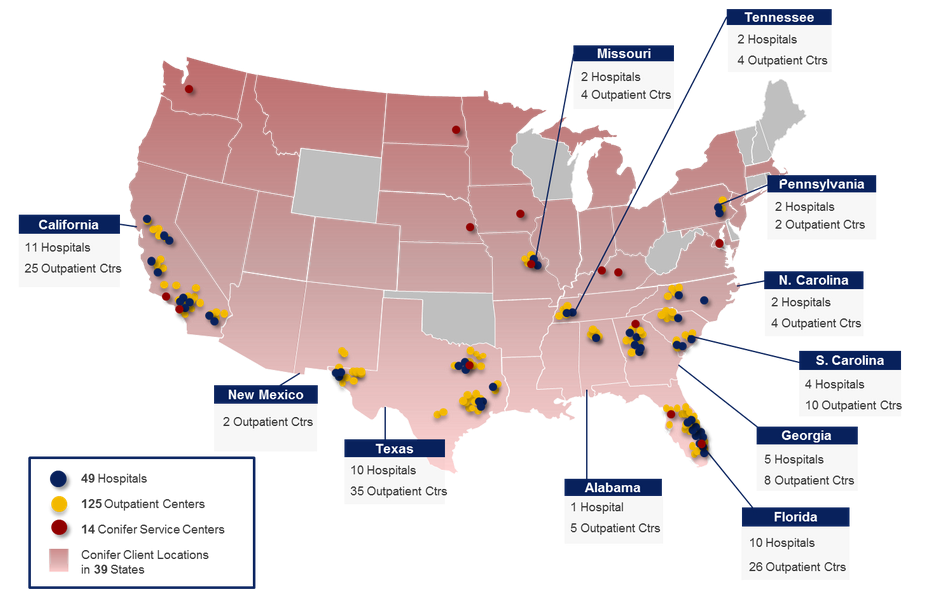
The pressures in the industry are driving hospitals and health systems to join forces. After more than a year of talks, CHI and San Francisco-based Dignity Health signed a definitive merger agreement in December 2017. The proposed transaction will create a massive nonprofit Catholic health system, comprising 139 hospitals across 28 states.
In the short term, the combination of the two systems is expected to drive synergies in the $500 million range, according to Mr. Swindle. In the coming months, the two systems will dive deeper into the synergies they expect to achieve over a multiyear period. “We do believe beyond the synergies there are some strategic initiatives we can put into place as a combined organization that we couldn’t do individually,” Mr. Swindle says. “You won’t see the benefit of those as much in the short term.”
“Take a deep breath”
Mr. Swindle knows firsthand that developing and executing an operational turnaround plan is no easy task. However, today’s healthcare landscape requires health systems to re-engineer their business models.
“Regardless of how good your results … have been over the last five to 10 years, we’re all going to have to transform ourselves in our own way to meet the characteristics of our organizations,” says Mr. Swindle.
When embarking on a performance improvement plan, the first thing health system CFOs should do is “take a deep breath,” he says. Then, they should focus on the things they have more control over. Mr. Swindle says it is critical for health systems to continue to drive improvement in patient experience and quality. They also need to be strategic cost managers.
“It’s not going to be as easy as just saying we’re going to take these [full-time employees] out or reduce this service. You’re really going to have to be very smart and very thoughtful about how you become a good cost manager that adds value to your communities,” says Mr. Swindle. “Don’t get too comfortable with your past success and your past models.”