Category Archives: Denial
Cartoon – In Denial
Oklahoma hospital terminates Medicare Advantage contracts amid financial challenges

Stillwater Medical Center in Oklahoma has ended all in-network contracts with Medicare Advantage plans amid financial challenges at the 117-bed hospital, the Stillwater News Press reported Oct. 14.
Humana and BCBS of Oklahoma were notified that their members will no longer receive in-network coverage after Jan. 1, 2023.
“BCBSOK is willing to work with Stillwater Medical Center in finding solutions that will allow Payne County residents continued local access to Medicare Advantage providers,” a BCBS spokesperson told the newspaper.
The hospital said it made the decision after facing rising operating costs and a high prior authorization burden for the MA plans.
“This was a very tough financial decision for the Stillwater Medical leadership team. Our cost to operate has increased 26 percent over the past 2 years,” Tamie Young, vice president of revenue cycle at SMC, told the News Press. “Financial challenges are increased by a 22 percent denial of service rate from Medicare Advantage plans. This is in comparison to a less than 1 percent denial rate from traditional Medicare.”
Hospitals urge Justice Department to probe insurers over routine denials
The American Hospital Association, on behalf of its nearly 5,000 healthcare organizations, is urging the Justice Department to probe routine denials from commercial health insurance companies.
Specifically, the AHA is asking the Justice Department to establish a task force to conduct False Claims Act investigations into the insurers that routinely deny payments to providers, according to a May 19 letter to the department.
The request from the AHA comes after HHS’ Office of Inspector General released a report April 27 that found Medicare Advantage Organizations sometimes delayed or denied enrollees’ access to services although the provider’s prior authorization request met Medicare coverage rules.
“It is time for the Department of Justice to exercise its False Claims Act authority to both punish those MAOs that have denied Medicare beneficiaries and their providers their rightful coverage and to deter future misdeeds,” the AHA said in a letter to the Justice Department. “This problem has grown so large — and has lasted for so long — that only the prospect of civil and criminal penalties can adequately prevent the widespread fraud certain MAOs are perpetrating against sick and elderly patients across the country.”
Read the full letter here.
Cartoon – One Vaccine Prevents Disease & Another Conspiracy Theories
Cartoon – Anti Vaxx Message is Spreading
Cartoon – Vaccination from Making Decisions based on Politics

Cartoon – A Shot of Common Sense

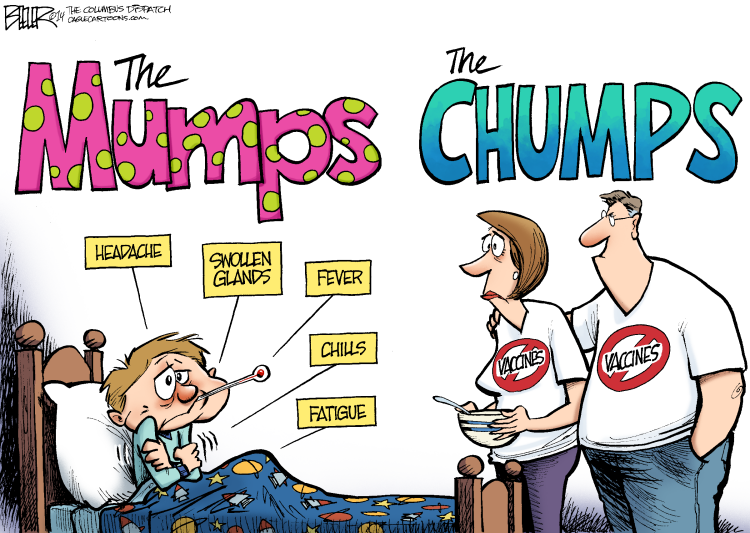
Cartoon – The Mumps vs Chumps
Cartoon – Things you can’t get vaccinated for

Hospital Volunteers Wanted


