Category Archives: High Prices
Hospitals charged employers and insurers 254% more than Medicare in 2022: study

Hospitals with larger market shares were among the worst offenders, the Rand Corporation found.
Dive Brief:
- Employers and private insurers continue to pay hospitals more for inpatient and outpatient services than Medicare would have reimbursed, according to a new study from policy think tank the Rand Corporation.
- In 2022, private insurers and employers paid on average 254% of what Medicare would have paid for the same care services — up from 224% two years prior.
- Health systems often argue they hike up commercial rates to offset losses from government underpayments, according to the study. However, a hospital’s market share, rather than population of Medicare or Medicaid patients, more accurately predicted pricing, with larger health systems charging higher prices.
Dive Insight:
Since 2021, health systems and insurers have been required to post pricing information for their 300 most common procedures as the government pushes to make healthcare prices more transparent.
However, researchers have accused hospitals and insurers of failing to fully comply with the regulations.
Only 34.5% of 2,000 hospitals reviewed by nonprofit watchdog organization Patient Rights Advocate were deemed fully compliant with price transparency rules as of January. But, the CMS had only issued 14 civil monetary penalty notices to noncompliant hospitals as of February, according to the nonprofit.
The Rand study found inpatient prices for hospital services were 255% above what Medicare paid in 2022 while outpatient hospital service prices averaged 289%, according to the report, which was based on an analysis of 4,000 hospitals across 49 states.
Prices for services at outpatient ambulatory surgical centers was slightly lower at 170% of Medicare payments.
There were also differences in pricing by geography. Arkansas, Iowa, Massachusetts, Michigan and Mississippi kept relative prices below 200% of Medicare prices during the study period. However, others had relative prices above 300% of Medicare. Hospitals in Florida and Georgia negotiated the highest relative rates.
Price transparency could be a tool for administrators of employer-sponsored plans to better negotiate employee benefits. Although employer-sponsored plans cover 160 million Americans, researchers said employers operate at a disadvantage when negotiating prices with providers and insurers due to a lack of detailed pricing information.
“The widely varying prices among hospitals suggests that employers have opportunities to redesign their health plans to better align hospital prices with the value of care provided,” said Brian Briscombe, lead researcher for the Rand hospital price transparency project, in a statement. “However, price transparency alone will not lead to changes if employers do not or cannot act upon price information.”
State and federal policymakers could rebalance negotiations by cracking down on noncompetitive healthcare markets, placing limits on payments for out-of-network hospital care or allowing employers to buy into Medicare or other public options, the report said.
The nation’s largest hospital lobby, the American Hospital Association, has rejected previous analyses of pricing data — including reports from Patient Rights Advocate.
On Monday, Molly Smith, AHA’s vice president for policy, pushed back against the Rand study, saying it was “suspiciously silent on the hidden influence of commercial insurers in driving up health care costs for patients, as evidenced by issues like the recent concerning allegations against MultiPlan.”
Last week, Community Health Systems filed suit against MultiPlan alleging it had colluded with insurers to raise prices for patients and lower payments to providers. The lawsuit is the third against MultiPlan in under a year.
Cartoon – Out of Pocket Experience
Cartoon – Ask Your Congressman
Unpacking one aspect of healthcare affordability
https://www.kaufmanhall.com/insights/blog/gist-weekly-april-12-2024
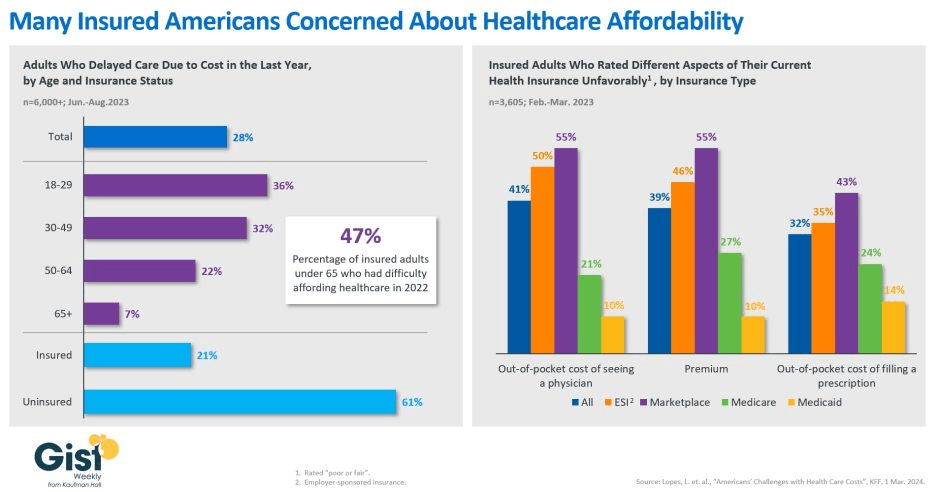
In this week’s graphic, we showcase recent KFF survey data on how healthcare costs impact the public, particularly those with health insurance.
Nearly half of US adults say it is difficult to afford healthcare, and in the last year, 28 percent have skipped or postponed care due to cost, with an even greater share of younger people delaying care due to cost concerns.
Although healthcare affordability has long been a problem for the uninsured, one in five adults with insurance skipped care in the past year because of cost. Insured Americans report low satisfaction with the affordability of their coverage.
In addition to high premiums, out-of-pocket costs to see a physician or fill a prescription are particular sources of concern. Adults with employer-sponsored or marketplace plans are far more likely to be dissatisfied with the affordability of their coverage, compared to those with government-sponsored plans.
With eight in ten American voters saying that it is “very important” for the 2024 presidential candidates to focus on the affordability of healthcare, we’ll no doubt see more attention focused on this issue as the presidential election race heats up.
Cartoon – Physician-Assisted Bankruptcy
How GoFundMe use demonstrates the problem of healthcare affordability
https://mailchi.mp/1e28b32fc32e/gist-weekly-february-9-2024?e=d1e747d2d8

Published this week in The Atlantic, this piece chronicles the increase in Americans using crowdfunding sites like GoFundMe to cover—or at least attempt to cover—their catastrophic medical expenses. Envisioned as a tool to fund “ideas and dreams,” the GoFundMe platform saw a 25-fold increase in the number of campaigns dedicated to medical care from 2011 to 2020.
Medical campaigns have garnered at least one third of all donations and raised $650M in contributions.
The article’s accounts of life-saving care leading to bankrupting medical bills are heartbreaking and familiar, and despite some success stories, the average GoFundMe medical campaign falls well short of its target donation goal.
The Gist:
Although unfortunately not surprising, these crowdfunding stats reflect our nation’s healthcare affordability crisis.
Online campaigns can alleviate real financial burdens for some people; however, they come at the costs of publicly exposing personal medical information, potentially offering false hope, and financially imposing on friends and family.
The majority of personal bankruptcies are caused by medical expenses, and recent changes like removing some levels of medical debt from credit reports are only a small step toward reducing the personal financial effects of medical debt.
Absent larger-scale healthcare payment and coverage reform, healthcare industry leaders continue to be challenged with finding ways to decouple the provision of essential medical care from the risk of financial ruin for patients.
3 huge healthcare battles being fought in 2024

Three critical healthcare struggles will define the year to come with cutthroat competition and intense disputes being played out in public:
1. A Nation Divided Over Abortion Rights
2. The Generative AI Revolution In Medicine
3. The Tug-Of-War Over Healthcare Pricing American healthcare, much like any battlefield, is fraught with conflict and turmoil. As we navigate 2024, the wars ahead seem destined to intensify before any semblance of peace can be attained. Let me know your thoughts once you read mine.
Modern medicine, for most of its history, has operated within a collegial environment—an industry of civility where physicians, hospitals, pharmaceutical companies and others stayed in their lanes and out of each other’s business.
It used to be that clinicians made patient-centric decisions, drugmakers and hospitals calculated care/treatment costs and added a modest profit, while insurers set rates based on those figures. Businesses and the government, hoping to save a little money, negotiated coverage rates but not at the expense of a favored doctor or hospital. Disputes, if any, were resolved quietly and behind the scenes.
Times have changed as healthcare has taken a 180-degree turn. This year will be characterized by cutthroat competition and intense disputes played out in public. And as the once harmonious world of healthcare braces for battle, three critical struggles take centerstage. Each one promises controversy and profound implications for the future of medicine:
1. A Nation Divided Over Abortion Rights
For nearly 50 years, from the landmark Roe v. Wade decision in 1973 to its overruling by the 2022 Dobbs case, abortion decisions were the province of women and their doctors. This dynamic has changed in nearly half the states.
This spring, the Supreme Court is set to hear another pivotal case, this one on mifepristone, an important drug for medical abortions. The ruling, expected in June, will significantly impact women’s rights and federal regulatory bodies like the FDA.
Traditionally, abortions were surgical procedures. Today, over half of all terminations are medically induced, primarily using a two-drug combination, including mifepristone. Since its approval in 2000, mifepristone has been prescribed to over 5 million women, and it boasts an excellent safety record. But anti-abortion groups, now challenging this method, have proposed stringent legal restrictions: reducing the administration window from 10 to seven weeks post-conception, banning distribution of the drug by mail, and mandating three in-person doctor visits, a burdensome requirement for many. While physicians could still prescribe misoprostol, the second drug in the regimen, its effectiveness alone pales in comparison to the two-drug combo.
Should the Supreme Court overrule and overturn the FDA’s clinical expertise on these matters, abortion activists fear the floodgates will open, inviting new challenges against other established medications like birth control.
In response, several states have fortified abortion rights through ballot initiatives, a trend expected to gain momentum in the November elections. This legislative action underscores a significant public-opinion divide from the Supreme Court’s stance. In fact, a survey published in Nature Human Behavior reveals that 60% of Americans support legal abortion.
Path to resolution: Uncertain. Traditionally, SCOTUS rulings have mirrored public opinion on key social issues, but its deviation on abortion rights has failed to shift public sentiment, setting the stage for an even fiercer clash in years to come. A Supreme Court ruling that renders abortion unconstitutional would contradict the principles outlined in the Dobbs decision, but not all states will enact protective measures. As a result, America’s divide on abortion rights is poised to deepen.
2. The Generative AI Revolution In Medicine
A year after ChatGPT’s release, an arms race in generative AI is reshaping industries from finance to healthcare. Organizations are investing billions to get a technological leg up on the competition, but this budding revolution has sparked widespread concern.
In Hollywood, screenwriters recently emerged victorious from a 150-day strike, partially focused on the threat of AI as a replacement for human workers. In the media realm, prominent organizations like The New York Times, along with a bevy of celebs and influencers, have initiated copyright infringement lawsuits against OpenAI, the developer of ChatGPT.
The healthcare sector faces its own unique battles. Insurers are leveraging AI to speed up and intensify claim denials, prompting providers to counter with AI-assisted appeals.
But beyond corporate skirmishes, the most profound conflict involves the doctor-patient relationship. Physicians, already vexed by patients who self-diagnose with “Dr. Google,” find themselves unsure whether generative AI will be friend or foe. Unlike traditional search engines, GenAI doesn’t just spit out information. It provides nuanced medical insights based on extensive, up-to-date research. Studies suggest that AI can already diagnose and recommend treatments with remarkable accuracy and empathy, surpassing human doctors in ever-more ways.
Path to resolution: Unfolding. While doctors are already taking advantage of AI’s administrative benefits (billing, notetaking and data entry), they’re apprehensive that ChatGPT will lead to errors if used for patient care. In this case, time will heal most concerns and eliminate most fears. Five years from now, with ChatGPT predicted to be 30 times more powerful, generative AI systems will become integral to medical care. Advanced tools, interfacing with wearables and electronic health records, will aid in disease management, diagnosis and chronic-condition monitoring, enhancing clinical outcomes and overall health.
3. The Tug-Of-War Over Healthcare Pricing
From routine doctor visits to complex hospital stays and drug prescriptions, every aspect of U.S. healthcare is getting more expensive. That’s not news to most Americans, half of whom say it is very or somewhat difficult to afford healthcare costs.
But people may be surprised to learn how the pricing wars will play out this year—and how the winners will affect the overall cost of healthcare.
Throughout U.S. healthcare, nurses are striking as doctors are unionizing. After a year of soaring inflation, healthcare supply-chain costs and wage expectations are through the roof. A notable example emerged in California, where a proposed $25 hourly minimum wage for healthcare workers was later retracted by Governor Newsom amid budget constraints.
Financial pressures are increasing. In response, thousands of doctors have sold their medical practices to private equity firms. This trend will continue in 2024 and likely drive up prices, as much as 30% higher for many specialties.
Meanwhile, drug spending will soar in 2024 as weight-loss drugs (costing roughly $12,000 a year) become increasingly available. A groundbreaking sickle cell disease treatment, which uses the controversial CRISPR technology, is projected to cost nearly $3 million upon release.
To help tame runaway prices, the Centers for Medicare & Medicaid Services will reduce out-of-pocket costs for dozens of Part B medications “by $1 to as much as $2,786 per average dose,” according to White House officials. However, the move, one of many price-busting measures under the Inflation Reduction Act, has ignited a series of legal challenges from the pharmaceutical industry.
Big Pharma seeks to delay or overturn legislation that would allow CMS to negotiate prices for 10 of the most expensive outpatient drugs starting in 2026.
Path to resolution: Up to voters. With national healthcare spending expected to leap from $4 trillion to $7 trillion by 2031, the pricing debate will only intensify. The upcoming election will be pivotal in steering the financial strategy for healthcare. A Republican surge could mean tighter controls on Medicare and Medicaid and relaxed insurance regulations, whereas a Democratic sweep could lead to increased taxes, especially on the wealthy. A divided government, however, would stall significant reforms, exacerbating the crisis of unaffordability into 2025.
Is Peace Possible?
American healthcare, much like any battlefield, is fraught with conflict and turmoil. As we navigate 2024, the wars ahead seem destined to intensify before any semblance of peace can be attained.
Yet, amidst the strife, hope glimmers: The rise of ChatGPT and other generative AI technologies holds promise for revolutionizing patient empowerment and systemic efficiency, making healthcare more accessible while mitigating the burden of chronic diseases. The debate over abortion rights, while deeply polarizing, might eventually find resolution in a legislative middle ground that echoes Roe’s protections with some restrictions on how late in pregnancy procedures can be performed.
Unfortunately, some problems need to get worse before they can get better. I predict the affordability of healthcare will be one of them this year. My New Year’s request is not to shoot the messenger.
Higher-risk patients paying more for colonoscopies
https://mailchi.mp/9b1afd2b4afb/the-weekly-gist-december-1-2023?e=d1e747d2d8
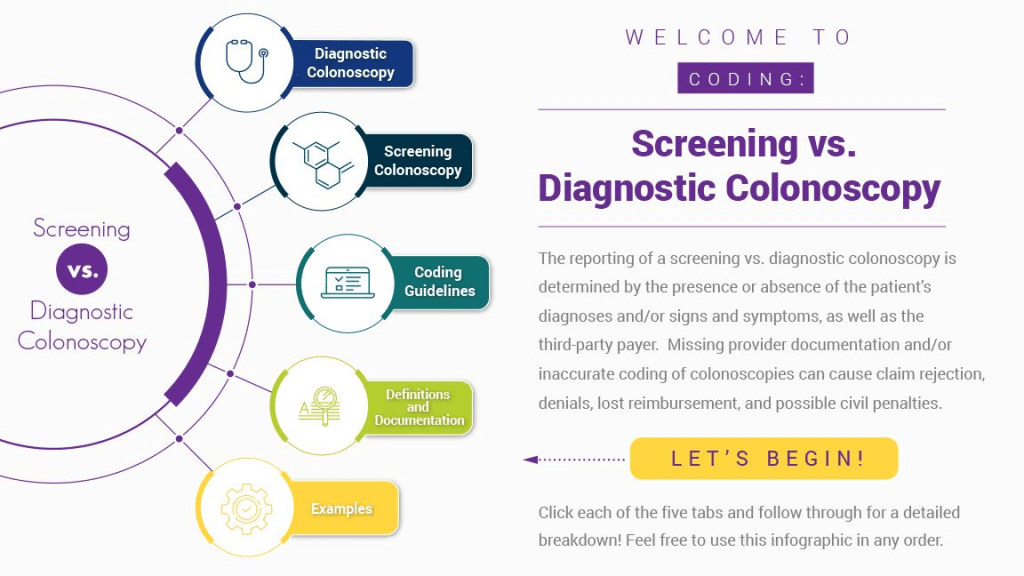
Published this week in Stat, this article explores the confusing payment landscape patients must navigate when receiving colonoscopies. While the Affordable Care Act requires that preventative care services be covered without cost-sharing, this only applies to the “screening” colonoscopies that low-risk patients are recommended to get every ten years.
But when procedures are performed at more frequent intervals for higher-risk patients, they are called “surveillance” or “diagnostic” colonoscopies, for which patients have no guarantees of cost-sharing protections, despite being essentially the same procedure, done for the same purpose.
If a gastroenterologist finds and excises one or more precancerous polyps during a screening colonoscopy, the procedure can leave the patient—especially one with a high deductible health plan—with a large, unexpected bill.
The Gist: Against the backdrop of a sharp rise in colorectal cancer rates among US adults under 65, articles like this are a frustrating demonstration of how insurance incentive structures can work against optimal care delivery.
Incentives should be carefully designed such that proven, preventative screenings—at the discretion of their doctor—are widely available to patients with minimal financial barriers. Surely, no one is “choosing” to have an “unnecessary” colonoscopy—as the procedure is notoriously disliked by patients.