With the coronavirus still spreading widely, it’s time to start thinking seriously about influenza, which typically spreads in fall and winter. A major flu outbreak would not only overwhelm hospitals this fall and winter, but also likely overwhelm a person who might contract both at once.
Doctors have no way of knowing yet what the effect of a dual diagnosis might be on a person’s body, but they do know the havoc that the flu alone can do to a person’s body. And, we know the U.S. death toll of COVID-19 as of Aug. 17, 2020 was 170,000, and doctors are learning more each day about the effects of the disease on the body. Public health officials in the U.S. are therefore urging people to get the flu vaccine, which is already being shipped in many areas to be ready for September vaccinations.
Flu cases are expected to start increasing early in October and could last late into May. This makes September and early October the ideal time to get your flu shot.
But there’s reason to be concerned that flu vaccination rates could be lower this year than in past years, even though the risk of getting seriously ill may be higher because of widespread circulation of the coronavirus.
In an effort to avoid getting sick, millions of Americans avoided seeing their health care provider the past few months. Social distancing and stay-at-home orders have resulted in a decreased use of routine medical preventive services such as vaccinations. Many employers that often provide the flu shot at no cost to employees are allowing employees to work from home, potentially limiting the number of people who will get the flu shot at their jobs.
As a health care professional, I urge everyone to get the flu vaccine in September. Please do not wait for flu cases to start to peak. The flu vaccine takes up to two weeks to reach peak effectiveness, so getting the vaccine in September will help provide the best protection as the flu increases in October and later in the season.
A lifesaver in previous years, but more so now
Both COVID-19 and the flu are contagious respiratory illness that present with similar symptoms. Both viruses can impact the elderly and those with certain chronic conditions, such as heart and lung disease, the hardest.
Data on flu vaccination rates from 2018-2019 show that only 49% of Americans six months of age and older received the flu vaccine. The vaccine’s effectiveness varies each season, with early data from the 2019-2020 flu season indicating a vaccine effectiveness rate of 50% overall, and 55% in youth.
While some may think this effectiveness rate is low, the flu vaccine remains the single best way to prevent the flu and related complications. For example, during the 2018-2019 flu season, flu vaccination was estimated to prevent 4.4 million flu illnesses, 58,000 flu hospitalizations and 3,500 deaths. Early data from the 2019-2020 flu season estimates there were 39-56 million flu illnesses, 18-26 million flu-related medical visits, 410-740,000 hospitalizations and up to 62,000 deaths. Much of this disease burden is preventable from higher flu vaccination rates.
It is now quite apparent that COVID-19 will still be circulating during flu season, which makes getting a flu vaccine more important than ever. As schools, our communities and our economy continue to reopen, it is vital to get the flu vaccine for personal, family and community protection.

A flu camp in Lawrence, Maine during the 1918 influenza pandemic. Nurses and doctors tried desperate measures to stop the spread of the disease, which ultimately killed more than 675,000 people in the U.S. alone. Bettmann/Getty Images
Severe cases of both COVID-19 and the flu require the same lifesaving medical equipment. This highlights the importance of getting the flu vaccine for not only your own personal health but also the health of your community. Receiving the flu vaccine will help reduce the burden of respiratory illness on our already very overstretched health care system. By increasing flu vaccination rates, we can reduce the overall impact of respiratory illnesses on the population and hence lower the resulting burden on the health care system during the COVID-19 pandemic.
Because flu vaccination protects against one of these respiratory illnesses, the CDC recommends everyone (with few exceptions) six months of age and older get an annual flu vaccine. While the flu vaccine will not protect you against COVID-19, the flu vaccine will reduce your risk of developing the flu as well as reduce your risks of flu-related complications including hospitalization and even death.
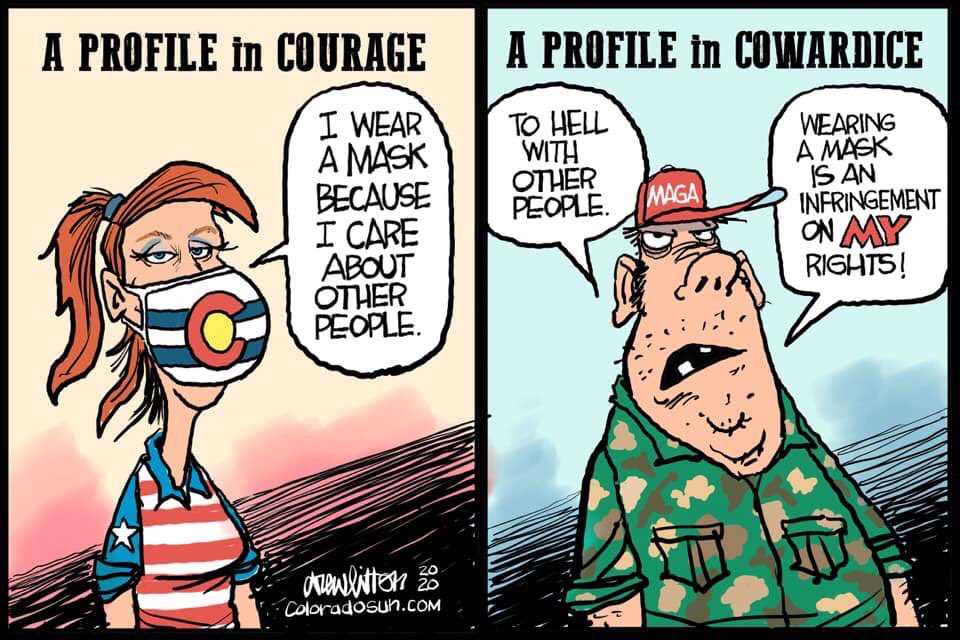
While it may seem like there is so much out of our control during this pandemic, getting the flu vaccine, practicing proper hand washing, social distancing and wearing face coverings are within our control and will protect not only you but also your family and community.
If you are not getting the flu vaccine from your employer, think about alternative sources now. Vaccines should be available in most areas by Sept. 1.
- Call you doctor’s office to ask how you can get a flu shot.
- Call your local public health department.
- Consider getting a vaccine while you are grocery shopping or picking up prescriptions.
Mainly, make sure you take advantage of this potentially lifesaving vaccine. Get it on your calendar for early September now. And remember, the flu shot cannot give you the flu.