Category Archives: Leadership
Thought of the Day: On Listening
Thought of the Day: Too Few Candies Left in the Box

“I know that I have less to live than I have lived.
I feel like a child who was given a box of chocolates. He enjoys eating it, and when he sees that there is not much left, he starts to eat them with a special taste.
I have no time for endless lectures on public laws – nothing will change. And there is no desire to argue with fools who do not act according to their age. And there’s no time to battle the gray. I don’t attend meetings where egos are inflated and I can’t stand manipulators.
I am disturbed by envious people who try to vilify the most capable to grab their positions, talents and achievements.
I have too little time to discuss headlines – my soul is in a hurry.
Too few candies left in the box.
I’m interested in human people. People who laugh at their mistakes are those who are successful, who understand their calling and don’t hide from responsibility. Who defends human dignity and wants to be on the side of truth, justice, righteousness. This is what living is for.
I want to surround myself with people who know how to touch the hearts of others. Who, through the blows of fate, was able to rise and maintain the softness of the soul.
Yes, I hustle, I hustle to live with the intensity that only maturity can give. I’ll eat all the candy I have left – they’ll taste better than the ones I already ate.
My goal is to reach the end in harmony with myself, my loved ones and my conscience.
I thought I had two lives, but it turned out to be only one, and it needs to be lived with dignity.”
Brilliant Anthony Hopkins
and free interpretation of Mario de Andrade’s poem
Thought of the Day: We are all one
Health systems bulk up C-suites ahead of transformation

Faced with tighter margins and continued rising costs, many health system C-suites are restructuring. At least 17 health systems have reorganized executive teams and some eliminated C-suite roles.
The chief operating officer role in particular has been on the chopping block for health systems but not everyone is slimming down.
Some are bulking up amid organizational transformation with an eye on the future.
In June, Sutter Health in Sacramento, Calif., named Todd Smith, MD, its inaugural senior vice president and chief physician executive, responsible for supporting the health system through clinical transformation. Dr. Smith will focus on service line standards, reducing variation and strengthening the system’s relationship with medical group and community physicians.
Sutter isn’t the only system adding clinical leaders to the C-suite. Mass General Brigham in Somerville, Mass., named Erica Shenoy, MD, PhD, its first chief of infection control in June. Her expanded role is accountable for leading the integration of infection control at the system and developing and implementing infection control standards, policies and measurements. She was also appointed to the National Infection Control Advisory Committee to guide HHS earlier this year.
Meritus Health in Hagerstown, Md., added physician leadership to its executive team. Adrian Park, MD, became the system’s first chief surgical officer with responsibility for building a surgical program with advanced technology and minimally invasive procedures to the system. He is known for surgical innovation in laparoscopic techniques, and holds more than 20 patents.
MaineHealth in Portland recently added Chris Thompson, MD, to the C-suite as the system’s first chief medical transformation officer. He is responsible for chief medical officer duties as well as innovating in care delivery.
Richmond, Va.-based VCU Health and OU Health in Oklahoma City named their first chief nursing executives as well earlier this year.
Health systems are also adding strategic experts with expertise in patient experience, transformation and data analytics.
Atlanta-based Emory Healthcare created a new role for Amaka Eneanya, MD, to serve as chief transformation officer, accountable for enhancing patient and clinician experiences. She took on the role in July and is tasked with developing systemwide strategies to boost patient experience, improve access to care, increase community engagement and enrich clinician experience. Dr. Eneanya works with the system’s diversity, equity and inclusion office to prioritize strategies for health equity, diversity and inclusion in care delivery as well.
“Amaka is a forward-thinking leader who is well versed in transformational strategy and operational structure and will help us move Emory Healthcare to the next level,” said Joon S. Lee, MD, CEO of Emory Healthcare. “We look forward to working with her in our continued pursuit to transform and strengthen patient access and the patient experience.”
Last year, Centura Health in Centennial, Colo., also added a chief transformation officer, Scott Lichtenberger, MD, as a new position to balance short-term improvements and long-term value. He is responsible for ensuring the system delivers results quickly.
Finally, Cleveland Clinic has elevated another IT leader into the C-suite in recent weeks. Albert Marinez was named the system’s first chief analytics officer, set to begin his new role Aug. 28. He previously served as chief analytics officer of Intermountain Health in Salt Lake City, and will be responsible for overseeing data strategies for better patient care and lower costs at Cleveland Clinic. He will also have accountability for boosting the system’s growth alongside chief digital officer Rohit Chandra, PhD.
Thought of the Day: Importance of Small Steps
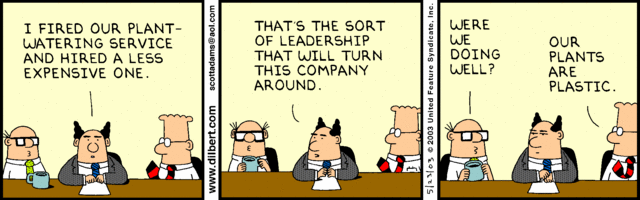
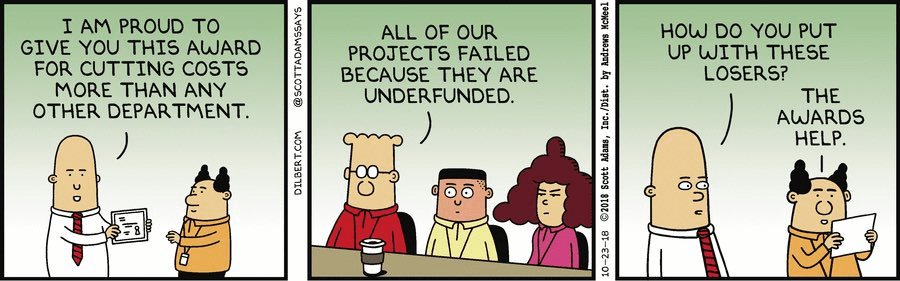
Cartoon – Operating Expense Reduction
How to convince the board that it’s time to merge
https://mailchi.mp/27e58978fc54/the-weekly-gist-august-11-2023?e=d1e747d2d8
This week we had a conversation with a health system executive who has been wondering how to make the case to his board for expansion beyond the existing markets where the organization operates.
Like many, he’s confronting declining margin performance, and feeling pressure to combine with another system—joining the wave of cross-market consolidation that’s been dominating discussion among system CEOs recently.
His concern was that his locally governed board may be putting an artificial brake on growth, not seeing value of expansion beyond their market for the community they serve.
That’s a valid point—how does it help a Busytown resident if the local health system expands to operate in Pleasantville? Shouldn’t Busytown Health System just focus its resources and time on improving performance at home, and wouldn’t it represent a loss to Busytown if Pleasantville got investment dollars that could have been spent locally?
That’s a question raised by the “super-regional” or national strategies being pursued by many large systems today, and one worth thinking about.
Whenever a system grows outside its geography, there should be a solid argument that additional scale will reap returns for its existing operations, from better efficiency, better access to innovation and talent, better access to capital, or the like.
Those are legitimate reasons for out-of-market growth and consolidation, as long as the systems involved are diligent in pursuing them.
But local boards are right to hold executives accountable for making the case for growth, and ensuring that growth creates value for local patients and purchasers.
Physicians lack trust in hospital leadership
https://mailchi.mp/c02a553c7cf6/the-weekly-gist-july-28-2023?e=d1e747d2d8

A recent physician survey conducted by strategic healthcare communications firm Jarrard Inc. uncovered a startling finding: only 36 percent of physicians employed by or affiliated with not-for-profit health systems trust that their system’s leaders are honest and transparent. In contrast, a slight majority of physicians working with investor-owned health systems and practices answered that question in the opposite.
Overall, only around half of physicians trust their organization’s leaders when it comes to financial, operational, and patient care decision-making. Unsurprisingly, doctors put the most trust in peer physicians, by a wide margin.
The Gist: While the numbers, especially for nonprofit systems, are stark, this survey reflects an on-the-ground reality felt at health systems in recent years. Physician fatigue has spiked in the wake of the pandemic.
And health system-physician relationships are also being disrupted by cost pressures, payer and investor acquisitions, and the shift of care to ambulatory settings. We’ve heard from physicians that, compared to hospital owners, investor-backed systems provide greater transparency and clearer financial goals centered around the success of the business.
That physicians trust their peers so highly suggests a path forward: provide physician leaders with greater transparency into system performance and agency over strategy, with clear goals and metrics.
Thought of the Day: On Leadership Environment
Some people in leadership positions, intentionally or not, harm their employees and their organization by creating a toxic work environment, causing their employees to focus on job searching or protecting themselves from internal forces instead of safeguarding the company against external threats.
According to Simon Sinek, if someone feels safe enough to raise their hands and say, “I made a mistake” or “I need some help,” that leader has created an environment where their people feel safe to be themselves. However, if someone is so focused on “covering themselves” and sending a CYA email after every conversation or meeting, that leader has created a toxic culture that shouts NOT SAFE, every man/woman for themselves.
Great leaders create an environment where their people can be themselves but, more importantly, to become the very best version of themselves.