
Category Archives: Investment
Healthcare CFOs Share Plans for 2024
https://www.linkedin.com/pulse/healthcare-cfos-share-plans-2024-steven-shill-k62nf/

The upheaval of the past few years has permanently changed the healthcare landscape, and while many sectors of the industry continue to endure financial hardship, there is reason for cautious optimism in 2024 as healthcare begins to see a return on investment in technology and a resurgence in dealmaking.
This year, BDO surveyed healthcare CFOs to discover their plans, priorities, and concerns heading into 2024.
In today’s newsletter, I’ve outlined the top research findings that every healthcare leader needs to know to prepare for the year ahead.
Top 3 Workforce Investment Areas
Clinician burnout and staffing shortages remain challenging in the healthcare industry, but BDO’s survey indicated that many CFOs are bullish that the worst is behind them, with 47% stating they feel that in 2024, the talent shortage will represent less of a risk than in 2023.
Investment in the workforce is crucial to addressing staffing challenges, and in the year ahead, healthcare CFOs intend to invest in the following ways:
1. Training: 48% of CFOs plan to spend more on training, in part to buttress ongoing investment in new technologies like AI that can help with predictive staffing and financial reporting.
2. Recruitment: 48% of CFOs will spend more on recruiting, as the talent shortfall tightens an already restricted pool of candidates.
3. Compensation & Benefits: Alongside greater spending on recruiting itself, 46% of CFOs intend to increase compensation and benefits as a means of attracting talent from competitors and retaining current staff.
Transaction Plans
Dealmaking turned a corner in 2023, with activity returning to pre-pandemic levels in Q2. Despite fluctuating interest rates and the volatility of an election year, we can expect more transactions in 2024, with 72% of CFOs planning some kind of deal, relative to their organization’s financial health and liquidity. An increase in antitrust activity, however, could impact the size and type of deals that see success. Healthcare CFOs planning a large deal should be prepared for heightened scrutiny.
While we expect to see a wide range of deals taking place over the next year, two specific deal types are worth calling out:
1. Carve-outs/Divestitures: We may see an uptick in enterprise sales, carve-outs, and divestitures, particularly for institutions that have been struggling financially — 31% of institutions that violated their bond or loan covenants in 2023 are planning to pursue deals of this kind.
2. Private Equity (PE) and Venture Capital (VC): Nearly one in five (19%) CFOs, particularly those working with physician groups, plan to explore PE and VC investment as avenues toward scaling, sharing services, and safeguarding succession planning.
Service Line Investment Plans
There are still many areas where CFOs are intending to increase investment, but changed market conditions mean that some core areas of healthcare may see decreased investment as the industry realigns:
1. Specialty Services: Fifty-two percent of CFOs plan to increase their investments in specialty services like cardiology, oncology, and dermatology, while 23% of CFOs intend to partner with a capital provider or operator.
2. Service Expansion: Home care (51%), virtual/telehealth (48%), and ambulatory service centers (49%) are also priority areas for investment as institutions continue to expand and maintain access to healthcare outside of traditional hospital and clinic settings.
3. Primary Care: Although primary care remains at the heart of the healthcare industry, many CFOs (42%) have in fact signaled an intent to reduce investment in this area, reassessing their primary care strategies due to significant cash flow pressures and ongoing realignment as the retail market gains ground.
Want to know more about healthcare leaders’ plans for the year ahead? Get more insights and data in BDO’s 2024 Healthcare CFO Outlook Survey.
Where are you planning on increasing investment in your organization this year? Let me know in the comments below.
One System; Two Divergent Views

Healthcare is big business. That’s why JP Morgan Chase is hosting its 42nd Healthcare Conference in San Francisco starting today– the same week Congress reconvenes in DC with the business of healthcare on its agenda as well. The predispositions of the two toward the health industry could not be more different.
Context: the U.S. Health System in the Global Economy
Though the U.S. population is only 4% of the world total, our spending for healthcare products and services represents 45% of global healthcare market. Healthcare is 17.4% of U.S. GDP vs. an average of 9.6% for the economies in the 37 other high-income economies of the world. It is the U.S.’ biggest private employer (17.2 million) accounting for 24% of total U.S. job growth last year (BLS). And it’s a growth industry: annual health spending growth is forecast to exceed 4%/year for the foreseeable future and almost 5% globally—well above inflation and GDP growth. That’s why private investments in healthcare have averaged at least 15% of total private investing for 20+ years. That’s why the industry’s stability is central to the economy of the world.
The developed health systems of the world have much in common: each has three major sets of players:
- Service Providers: organizations/entities that provide hands-on services to individuals in need (hospitals, physicians, long-term care facilities, public health programs/facilities, alternative health providers, clinics, et al). In developed systems of the world, 50-60% of spending is in these sectors.
- Innovators: organizations/entities that develop products and services used by service providers to prevent/treat health problems: drug and device manufacturers, HIT, retail health, self-diagnostics, OTC products et al. In developed systems of the world, 20-30% is spend in these.
- Administrators, Watchdogs & Regulators: Organizations that influence and establish regulations, oversee funding and adjudicate relationships between service providers and innovators that operate in their systems: elected officials including Congress, regulators, government agencies, trade groups, think tanks et al. In the developed systems of the world, administration, which includes insurance, involves 5-10% of its spending (though it is close to 20% in the U.S. system due to the fragmentation of our insurance programs).
In the developed systems of the world, including the U.S., the role individual consumers play is secondary to the roles health professionals play in diagnosing and treating health problems. Governments (provincial/federal) play bigger roles in budgeting and funding their systems and consumer out-of-pocket spending as a percentage of total health spending is higher than the U.S. All developed and developing health systems of the world include similar sectors and all vary in how their governments regulate interactions between them. All fund their systems through a combination of taxes and out-of-pocket payments by consumers. All depend on private capital to fund innovators and some service providers. And all are heavily regulated.
In essence, that makes the U.S. system unique are (1) the higher unit costs and prices for prescription drugs and specialty services, (2) higher administrative overhead costs, (3) higher prevalence of social health issues involving substance abuse, mental health, gun violence, obesity, et al (4) the lack of integration of our social services/public health and health delivery in communities and (5) lack of a central planning process linked to caps on spending, standardization of care based on evidence et al.
So, despite difference in structure and spending, developed systems of the world, like the U.S. look similar:
The Current Climate for the U.S. Health Industry
The global market for healthcare is attractive to investors and innovators; it is less attractive to most service providers since their business models are less scalable. Both innovator and service provider sectors require capital to expand and grow but their sources vary: innovators are primarily funded by private investors vs. service providers who depend more on public funding. Both are impacted by the monetary policies, laws and political realities in the markets where they operate and both are pivoting to post-pandemic new normalcy. But the outlook of investors in the current climate is dramatically different than the predisposition of the U.S. Congress toward healthcare:
- Healthcare innovators and their investors are cautiously optimistic about the future. The dramatic turnaround in the biotech market in 4Q last year coupled with investor enthusiasm for generative AI and weight loss drugs and lower interest rates for debt buoy optimism about prospects at home and abroad. The FDA approved 57 new drugs last year—the most since 2018. Big tech is partnering with established payers and providers to democratize science, enable self-care and increase therapeutic efficacy. That’s why innovators garner the lion’s share of attention at JPM. Their strategies are longer-term focused: affordability, generative AI, cost-reduction, alternative channels, self-care et al are central themes and the welcoming roles of disruptors hardwired in investment bets. That’s the JPM climate in San Franciso.
- By contrast, service providers, especially the hospital and long-term care sectors, are worried. In DC, Congress is focused on low-hanging fruit where bipartisan support is strongest and political risks lowest i.e.: price transparency, funding cuts, waste reduction, consumer protections, heightened scrutiny of fraud and (thru the FTC and DOJ) constraints on horizontal consolidation to protect competition. And Congress’ efforts to rein in private equity investments to protect consumer choice wins votes and worries investors. Thus, strategies in most service provider sectors are defensive and transactional; longer-term bets are dependent on partnerships with private equity and corporate partners. That’s the crowd trying to change Congress’ mind about cuts and constraints.
The big question facing JPM attendees this week and in Congress over the next few months is the same: is the U.S. healthcare system status quo sustainable given the needs in other areas at home and abroad?
Investors and organizations at JPM think the answer is no and are making bets with their money on “better, faster, cheaper” at home and abroad. Congress agrees, but the political risks associated with transformative changes at home are too many and too complex for their majority.
For healthcare investors and operators, the distance between San Fran and DC is further and more treacherous than the 2808 miles on the map.
The JPM crowd sees a global healthcare future that welcomes change and needs capital; Congress sees a domestic money pit that’s too dicey to handle head-on–two views that are wildly divergent.
So Much to Worry About

If you are a hospital executive—and if you are reading this, you probably are—then you have no shortage of worries. The worry list is long:
- Trying to control expenses.
- Dealing with declining revenue, especially when considered on an after-inflation basis.
- Struggling with ongoing staffing issues that have no immediate solutions.
- Solving the longstanding problem of patient access to appointments and service.
And the list could go on and on.
But maybe the biggest concern is one that is not on many worry lists: the remarkable development of artificial intelligence (AI) and how AI is relentlessly pushing into business practice generally and into healthcare more specifically.
While the long-term worry is how your hospital will carefully and properly adopt AI inside the business and clinical parts of your organization, the more immediate and short-term worry is whether you, as an executive, understand AI in a way that you can be ultimately useful to your organization.
Full disclosure: I can’t help here much. For me, AI is a pretty big black box. But when I confront this kind of business problem I start reading and learning. One of the most useful AI articles I have come across is “The Optimists: The Full Story of Microsoft’s Relationship with OpenAI,” which was published in the December 11, 2023, issue of The New Yorker magazine. The article was written by Charles Duhigg, a former winner of the Pulitzer Prize.
I am hoping that for your own professional development you will read the Duhigg article, but just in case, here are the highlights:
- Microsoft has reportedly invested $13 billion in the for-profit arm of OpenAI.
- Using OpenAI technology, Microsoft has built a series of AI assistants into Word, Outlook, and PowerPoint. These AI assistants are now known as Office Copilots.
- Knowledgeable commentators say these Microsoft applications are only moderately sophisticated but, honestly, they seem rather remarkable to me. Here are some of Duhiggs’s examples of requests Office Copilot users can make:
- “Tell me the pros and cons of each plan described on that video call.”
- “What’s the most profitable product in these twenty spreadsheets?”
- How about writing projects? Duhigg notes that the Office Copilot can:
- Create a financial narrative of the past decade based on a company’s last ten executive summaries.
- Turn a memo into a PowerPoint.
- Compile a to-do list for Teams video attendees, in multiple languages, after listening in on a meeting.
- Later in the article Duhigg details the functionality of the Word Copilot:
- “You can ask it to reduce a five-page document to ten bullet points…[o]r…it can take the ten bullet points and transform them into a five-page document.”
- It can write a memo based on previous emails you have written.
- “You can ask, ‘Did I forget to include anything that usually appears in a contract like this?,’ and the Copilot will review your previous contracts.”
Duhigg reports that Microsoft previously acquired a company called GitHub. GitHub is “a website where users shared code and collaborated on software.” Microsoft operates GitHub as an independent division. GitHub has been a very big success and is used by software engineers and, in a short period of time, has grown to over 100 million users.
OpenAI created an artificial intelligence tool that autocompletes software code. Despite reservations at Microsoft, GitHub President Nat Friedman decided to release the GitHub Copilot autocomplete tool. The result has been $100 million in revenue to GitHub in less than a year.
At the end of the article, Duhigg notes that these early AI business applications are both “impressive and banal.” Banal because they don’t yet live up to the sci-fi predictions for AI and its long-term impact on society.
Honestly, I don’t see it that way. This OpenAI/Microsoft collaboration is only scratching the surface and its potential uses are already endless, waiting to be invented by 100s of millions of users all over the world, including in healthcare. From my seat, the sky is the limit here. Almost anything seems possible.
I hope this summary of Mr. Duhigg’s exceptional article proves useful and advances your awareness of AI’s aggressive and rapid move into day-to-day business—here, through many of the Microsoft productivity programs that every one of us uses every day. In any case, I recommend that you read Duhigg’s entire article. It is most certainly worth your time.
How to convince the board that it’s time to merge
https://mailchi.mp/27e58978fc54/the-weekly-gist-august-11-2023?e=d1e747d2d8

This week we had a conversation with a health system executive who has been wondering how to make the case to his board for expansion beyond the existing markets where the organization operates.
Like many, he’s confronting declining margin performance, and feeling pressure to combine with another system—joining the wave of cross-market consolidation that’s been dominating discussion among system CEOs recently.
His concern was that his locally governed board may be putting an artificial brake on growth, not seeing value of expansion beyond their market for the community they serve.
That’s a valid point—how does it help a Busytown resident if the local health system expands to operate in Pleasantville? Shouldn’t Busytown Health System just focus its resources and time on improving performance at home, and wouldn’t it represent a loss to Busytown if Pleasantville got investment dollars that could have been spent locally?
That’s a question raised by the “super-regional” or national strategies being pursued by many large systems today, and one worth thinking about.
Whenever a system grows outside its geography, there should be a solid argument that additional scale will reap returns for its existing operations, from better efficiency, better access to innovation and talent, better access to capital, or the like.
Those are legitimate reasons for out-of-market growth and consolidation, as long as the systems involved are diligent in pursuing them.
But local boards are right to hold executives accountable for making the case for growth, and ensuring that growth creates value for local patients and purchasers.
Beyond Hype: Getting the Most Out of Generative AI in Healthcare Today
https://www.bain.com/insights/getting-the-most-out-of-generative-ai-in-healthcare/

Generative AI applications can already help health systems improve margins, yet only 6% have a strategy ready.
At a Glance
- In the wake of their most challenging financial year since 2020, US hospitals are desperately searching for margin improvements.
- Generative AI can increase productivity and cost efficiency, but only 6% of health systems currently have a strategy.
- Leading providers and payers will start with highly focused, low-risk generative AI use cases, generating the funds and experience for more transformative future applications.
While Covid-19 may no longer be dominating the global news cycle, healthcare providers and payers are still feeling its reverberations. More than half of US hospitals ended 2022 with a negative margin, marking the most difficult financial year since the start of the pandemic.
CEOs and CFOs remember the challenges all too well: The Omicron surge halted nonurgent procedures in the first half of the year, government support tapered off, and labor expenses ballooned amid staffing shortages. There was also the record-high inflation that continues to intensify margin pressures today. According to a recent Bain survey of health system executives, 60% cite rising costs as their greatest concern.
Payers and providers are now on the hunt for margin improvements. In our experience, the most successful companies won’t merely reduce costs, but also ramp up productivity. When done right, modest technology investments can accomplish both.
Artificial intelligence (AI) may hold part of the answer. With the costs to train a system down 1,000-fold since 2017, AI provides an arsenal of new productivity-enhancing tools at a low investment.
Many executives recognize the growing opportunity, especially with the recent rise of generative AI, which uses sophisticated large language models (LLMs) to create original text, images, and other content. It’s inspiring an explosion of ideas around use cases, from reviewing medical records for accuracy to making diagnoses and treatment recommendations.
Our survey reveals that 75% of health system executives believe generative AI has reached a turning point in its ability to reshape the industry. However, only 6% have an established generative AI strategy.
It’s time to play offense—or be forced to play defense later. But choosing from the laundry list of generative AI applications is daunting. Companies are at high risk of overinvesting in the wrong opportunities and underinvesting in the right ones, undermining future profitability, growth, and value creation. A wait-and-see approach is a tempting prospect.
However, we believe the next generation of leading healthcare companies will start today, with highly focused, low-risk use cases that boost productivity and cost efficiency. Over the next three to nine months, these companies will improve margins and learn how to implement a generative AI strategy, building up the funds and experience needed to invest in a more transformative vision.
Endless potential—and high hurdles
The excitement around generative AI may feel akin to the hype around other recent digital and technology developments that never quite rose to their promised potential. Well-intentioned, well-informed individuals are debating how much change will truly materialize in the next few years. While developments over the past six months have been a testament to the breakneck speed of change, nobody can accurately predict what the next six months, year, or decade will look like. Will new players emerge? Will we rely on different LLMs for different use cases, or will one dominate the landscape?
Despite the uncertainty, generative AI already has the power to alleviate some of providers’ biggest woes, which include rising costs and high inflation, clinician shortages, and physician burnout. Quick relief is critical, considering that the heightened risk of a recession will only compound margin pressures, and the US could be short 40,800 to 104,900 physicians by 2030, according to the Association of American Medical Colleges.
Many health systems are eyeing imminent opportunities to reduce administrative burdens and enhance operational efficiency. They rank improving clinical documentation, structuring and analyzing patient data, and optimizing workflows as their top three priorities (see Figure 1).
Figure 1
In the near term, generative AI can reduce administrative burdens and enhance efficiency

Some generative AI applications are already streamlining administrative tasks and allowing thinly stretched physicians to spend more time with patients. For instance, Doximity is rolling out a ChatGPT tool that can draft preauthorization and appeal letters. HCA Healthcare partnered with Parlance, a conversational AI-based switchboard, to improve its call center experience while reducing operators’ workload. And there are new announcements seemingly every week: Consider how healthcare software company Epic Systems is incorporating ChatGPT with electronic health records (EHRs) to draft response messages to patients, or how Google Cloud is launching an AI-enabled Claims Acceleration Suite for prior authorization processing.
These applications only scratch the surface of potential. In the future, generative AI could profoundly transform care delivery and patient outcomes. Looking ahead two to five years, executives are most interested in predictive analytics, clinical decision support, and treatment recommendations (see Figure 2).
Figure 2
Predictive analytics, clinical decisions, and care recommendations are long-term generative AI priorities

It’s hard not to catch AI “fever.” But there are real challenges ahead. Some are already tackling the biggest questions: Organizations such as Duke Health, Stanford Medicine, Google, and Microsoft have formed the Coalition for Health AI to create guidelines for responsible AI systems. Even so, solutions to the greatest hurdles aren’t yet keeping up with the rapid technology development.
Resource and cost constraints, a lack of expertise, and regulatory and legal considerations are the largest barriers to implementing generative AI, according to executives (see Figure 3).
Figure 3
A lack of resources, expertise, and regulation are the biggest barriers to generative AI in healthcare

Even when organizations can overcome these hurdles, one major challenge remains: focus and prioritization. In many boardrooms, executives are debating overwhelming lists of potential generative AI investments, only to deem them incomplete or outdated given the dizzying pace of innovation. These protracted debates are a waste of precious organizational energy—and time.
Starting small to win big
Setting the bar too high is setting up for failure. It’s easy to get caught up, betting big on what seems like the greatest opportunity in the moment. But 12 months later, leaders often find themselves frustrated that they haven’t seen results or feeling as if they’ve made a misplaced bet. Momentum and investments slow, further hindering progress.
Leading companies are forming a more pragmatic strategy that considers current capabilities, regulations, and barriers to adoption. Their CEOs and CFOs work together to enforce four guiding principles:
- Pilot low-risk applications with a narrow focus first. Tomorrow’s leaders are making no-regret moves to deliver savings and productivity enhancements in short order—at a time when they need it most. Gaining experience with currently available technology, they are testing and learning their way to minimum viable products in low-risk, repeatable use cases. These quick wins are typically in areas where they already have the right data, can create tight guardrails, and see a strong potential return on investment. Some, like call center and chatbot support, can improve the patient experience. However, given the current challenges around regulation and compliance, the most successful early initiatives are likely to be internally focused, such as billing or scheduling. Most importantly, executives prioritize initiatives by potential savings, value, and cost.
- Decide to buy, partner, or build. CEOs will need to think about how to invest in different use cases based on availability of third-party technology and importance of the initiative.
- Funnel cost savings and experience into bigger bets. As the technology matures and the value becomes clear, companies that generate savings, accumulate experience, and build organizational buy-in today will be best positioned for the next wave of more sophisticated, transformative use cases. These include higher-risk clinical activities with a greater need for accuracy due to ethical and regulatory considerations, such as clinical decision support, as well as administrative activities that require third-party integration, such as prior authorization.
- Remember generative AI isn’t a strategy unto itself. To build a true competitive advantage, top CEOs and CFOs are selective and discerning, ensuring that every generative AI initiative reinforces and enables their overarching goals.
Some health systems are already seeing powerful results from relatively small, more practical investments. For instance, recognizing that clinicians were spending an extra 130 minutes per day outside of working hours on administrative tasks, the University of Kansas Health System partnered with Abridge, a generative AI platform, to reduce documentation burden. By summarizing the most important points from provider-patient conversations, Abridge is improving the quality and consistency of documentation, getting more patients in the door, and cutting down on pervasive physician burnout.
Although it will require some upfront investment, in the long run it will be more costly to underestimate the level and speed at which generative AI will transform healthcare. The next generation of leaders will start testing, learning, and saving today, putting them on a path to eventually revolutionize their businesses.
Healthcare Finance Trends for 2023: Multiple Intersecting Challenges
https://www.commercehealthcare.com/trends-insights/2023/healthcare-finance-trends-for-2023

This annual look at high-impact trends affecting healthcare in the coming year is based on evaluation of current industry research data. Healthcare Finance Trends for 2023 (Trends) explores eight themes identified by CommerceHealthcare® ranging across four areas:
- Financial. Providers enter the year contending with multiple financial stress points. They will also seek growth in technology-enabled remote care.
- Patient financial experience. The need to drive not only improvement but also personalization of the financial experience is paramount. A central role will be played by patient financing programs which will see growing demand in 2023.
- Trust. Building trust with all constituencies is explored as a linchpin for long-term provider success. The latest findings on cybersecurity show that this contributor to trust will continue to consume leadership attention.
- Digital transformation. Pursuit of digital-first operations is accelerating, with the finance area an important focus. Emerging payment modes are finding a home in healthcare’s digital finance landscape.
This report’s consistent message is that these trends intersect in ways that compound both the challenges and the upside potential of strategies that address them.
1. Multiple Financial Stress Points Will Constrain Options
Healthcare’s financial predicament for the next 12–18 months is being described in strong terms. Citing $450 billion of EBITDA that could be in jeopardy, more than half of the industry’s project profit pool by 2027, one analyst suggests “a gathering storm.” Another perceives “broad and serious threats” as “elevated expenses” erode margins and exact “a profound financial toll.” Fitch Ratings issued a “deteriorating” outlook for nonprofit health systems.
These financial headwinds are upending healthcare’s traditional status as “recession-proof.” It is helpful to probe the multiple forces in play, the urgent workforce management challenge, and the varied solution set.
Multiple stress factors at work
Observing that margins will be down 37% in 2022 relative to pre-pandemic, a recent stark assessment concluded, “U.S. hospitals are likely to face billions of dollars in losses — which would result in the most difficult year for hospitals and health systems since the beginning of the pandemic.”
A confluence of factors is exacerbating the stress for 2023:
- Rising acuity levels. Over two-thirds of surveyed C-suite executives said patient health has worsened from pandemic-induced delayed care. The upshot, stated by 27% of CFOs, is rising expenses due to higher acuity. Inpatient days are projected to increase at an 8% rate over the coming decade.
- Reimbursement gaps and inflation. Commercial and government reimbursement rates are not keeping pace with rising costs. Surging inflation is widening this gap. Hospitals are also reporting substantial insurer payment delays and denials.
- Investment declines. Stock and bond market declines have removed a cushion for operating weakness. Market uncertainty will complicate 2023 portfolio management.
Persistent workforce concerns remain center stage
Burnout and shortages have disrupted the clinical workforce. Nearly 60% of physician, advanced practice provider and nurse survey respondents said their teams are not adequately staffed, and 40% lack resources to operate at full potential. Many providers face extreme to moderate shortages of allied health professionals.
The problem extends beyond the clinical. A survey saw 48% of respondents experiencing severe labor deficiencies in revenue cycle management (RCM) and billing, and one in four finance leaders must fill over 20 positions to be fully staffed.
An executive outlook highlighted demonstrable impact on financial performance and growth from these workforce problems, citing reductions in profitability, capacity and service (Figure 1).1
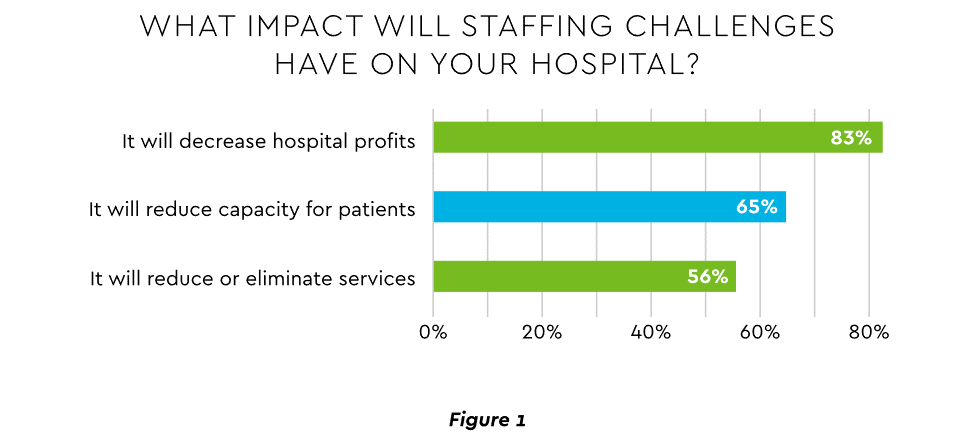
View PDF of Figure 1 chart[PDF]
Several studies detail negative outcomes:
- Expenses. Hospital employee expense is expected to increase $57 billion from 2021 to 2022, with contract labor ballooning another $29 billion. Average weekly earnings are up 21.1% since early 2022. Half of medical practices budgeted higher staff cost-of-living increases in 2022. Shortages plague post-acute facilities as well. Their reduced capability to accept discharged patients is lengthening many hospitals’ patient stays.
- Capacity constraint. Two-thirds of healthcare leaders identify “ability to meet demand” as their top workforce concern, suggesting a “looming capacity gap between future demand and labor supply.”
Range of measures being deployed
Health systems, hospitals and practices will vigorously pursue at least four direct actions to overcome the financial and staffing hurdles:
- Cost cutting. Expense control will be paramount and “hospitals will be forced to take aggressive cost-cutting measures.” McKinsey estimates total industry administrative savings of $1 trillion through multiple aggressive changes.
- Service line rationalization. Providers are rethinking how they deliver services to optimize efficiency. One path is utilizing “lower level” healthcare professionals in ways that free RNs and LPAs for more complex work suited to their top skills. Integrating remote care into the mix is another core element of the strategy.
- Recruitment and retention programs. Attracting and retaining talent is crucial. Compensation is one avenue. Over two-thirds of organizations are offering signing bonuses for allied health professionals. Some are instituting value-based payments for physicians, offering salary floors to protect from drops in patient volume. CFOs and CNOs are joining forces to invest in nurse retention strategies.
- Staffing management. An increasingly popular tool to reduce labor cost and optimize staff resources is outsourcing. Figure 2 shows that RCM is leading the way among those using the solution.
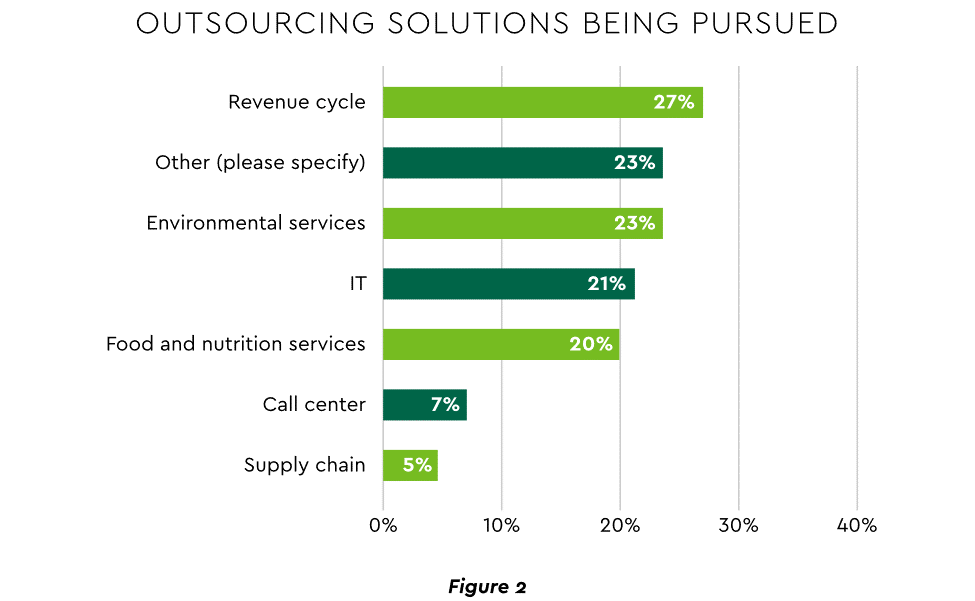
View PDF of Figure 2 chart[PDF]
2. Growth Strategies Favor Outpatient, Virtual, Acute Home Care
Pursuing top line growth in tandem with reining in expenses is essential. Inpatient volume growth has been tepid for several years ─ essentially flat in the 2016–20 period (Figure 3).
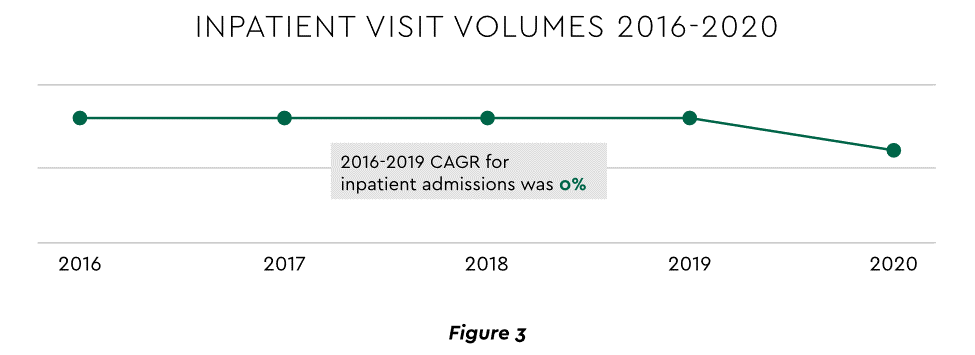
View PDF of Figure 3 chart[PDF]
Leaders have been pivoting to outpatient and virtual care to diversify revenue streams. Two high-potential 2023 growth tracks in this sector merit deeper assessment.
Telehealth
Considerable evidence attests to strong commitment to telehealth and remote care. Sixty-three percent of physicians worldwide expect most consultations to be performed remotely within 10 years. Approximately 40% of health centers are using remote patient monitoring today. Consumers are also positive: 94% definitely or probably will use telehealth again, 57% prefer it for regular mental health visits and 61% use it for convenient care.
Telehealth is still in early stages of maturity. Only 4% of surveyed top executives consider their organization proficient at implementing remote care. Healthcare is also recognizing that a full telehealth ecosystem must be constructed. A physician leader explained that the industry’s early telehealth incarnations failed to build “virtual-only environments or really drive e-consults as a way of doing things.” A vital ecosystem demands alterations to current contracts, coding, collections, patient financing, staff training and other business practices.
Hospital-at-Home (HaH)
Health systems see particularly promising growth in the provision of acute care in patients’ home settings, including post-surgical and cancer treatment. The federal government has already allowed waivers to 114 systems and 256 hospitals to obtain inpatient-level reimbursement for acute care at home. However, these waivers were prompted by the pandemic and are slated to end in early 2023. The renewal uncertainty has stymied some activity and represents an overhang on the opportunity. However, enthusiasm appears strong, and 33% of hospitals in a recent poll said they would be prone to continue HaH even without renewal.
The forecasts are encouraging. Over half of hospitals believe it likely they will utilize HaH for at least half of their chronically ill patients over the next several years (Figure 4).
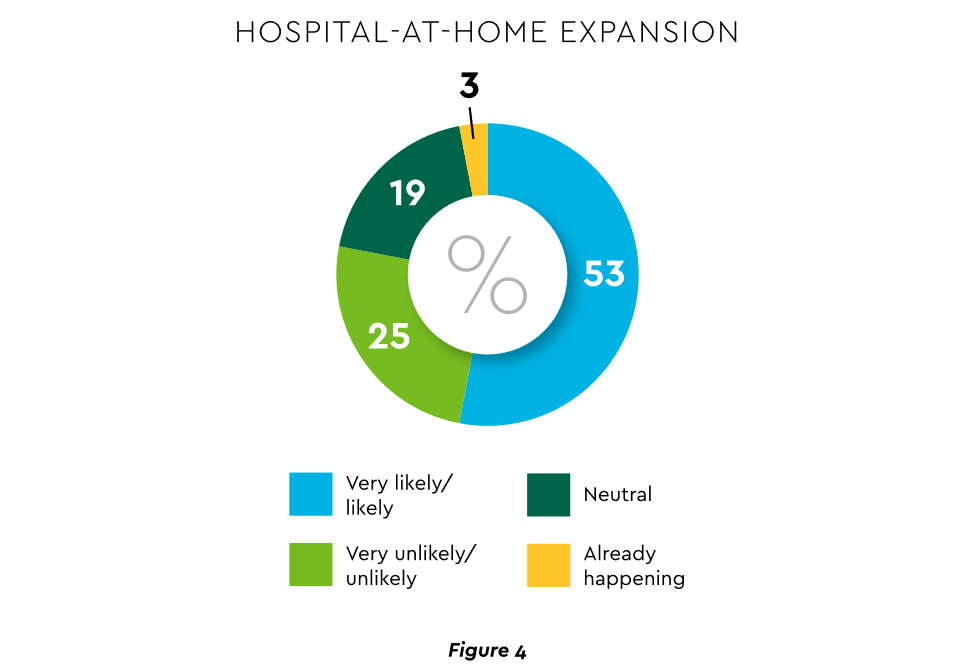
View PDF of Figure 4 chart[PDF]
HaH exists within a broader matrix of home care, and solid growth is anticipated across the range of home procedures (Figure 5).
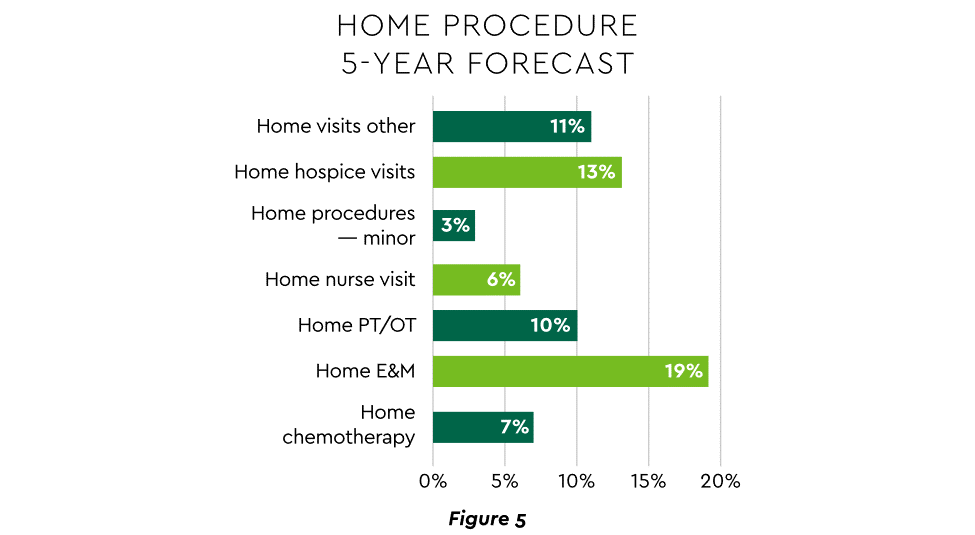
View PDF of Figure 5 chart[PDF]
Harvesting the HaH potential will require implementation of current and emerging enabling technologies in remote monitoring, high-speed networks and artificial intelligence that generates algorithmic guidance for caregivers and patients alike.
3. Strong Drive to Improve and Personalize the Patient Financial Experience
Today’s healthcare market dynamics place a premium on positive patient experiences. The goal is to deliver “an empathetic relationship between customers and brands built on what the customer wants and how they want to be treated.” It is a complex undertaking, with numerous touchpoints as captured in HFMA’s Consumerism Maturity Model (Figure 6).
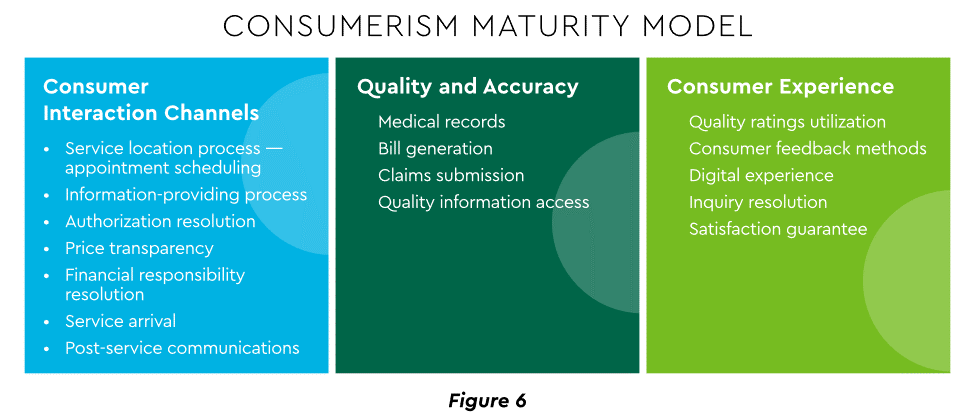
View PDF of Figure 6 chart[PDF]
An array of studies underscores the value proposition for intense provider focus on patient financial experience:
- Sixty-one percent of consumers said that ease of making payments is very or somewhat important in decisions to continue seeing a doctor. Over half of patients also said text message reminders make them very or somewhat more likely to pay a bill faster than usual.
- Thirty-five percent of respondents “have changed or would change healthcare providers to get a better digital patient administrative experience.”
- A quality financial experience encompasses “simplified explanations, consolidated bills that match one’s health plan benefits, clear language displaying patient liability and payment options.”35
Significantly improving the financial experience requires a unified strategy, not just a collection of individual initiatives. Three threads to such a strategy will be prominent in 2023.
Using a Digital Front Door
Organizations have been moving swiftly to channel many patient financial transactions through an integrated Digital Front Door (DFD). This approach offers patients a singular online point of access and intelligent navigation to needed services.
Growth is accelerating. A DFD is their patients’ first contact point for 55% of responding organizations, according to one technology survey. A leading forecaster sees 65% of patients engaging services via digital front doors by 2023.
Expanding price transparency
Mandates for full price transparency and “no surprises” billing are in effect, but estimates of compliance are mixed. An analysis of 2,000 hospitals determined that only 16% met the requirement to post an online “machine readable” file displaying clear charges for 300 “shoppable services.” Another assessment showed a more substantial 76% of hospitals had posted files, and 55% were deemed “complete.” One provision of interest to practices is the “good faith estimate” of expected charges required to be given to uninsured and self-pay individuals when they schedule visits.
CommerceHealthcare® has worked with clients to enhance the patient financial experience by complementing their website pricing data with clear information on patient financing options and enrollment access. Bill pay information can also be added for one-stop guidance.
Personalizing the experience
Beyond choice and convenience, the deeper objective is truly personalized experiences throughout the care journey. The words of leading analysts best define the drive to personalize:
- “Tomorrow’s healthcare experience will be built by patients tailoring their own experience.”
- “By 2024, 30% of chronic care patients will truly own and openly leverage their personal health information to advocate for, secure, and realize better personalized care.”
Opportunities abound to personalize the patient financial experience. Automating manual processes establishes a foundation. Patient financing with no- or low-interest credit lines and flexible terms can produce monthly payment schedules tailored to each patient’s needs. Refunds can be made through multiple payment modes to meet varying patient preferences.
4. Evidence Underscores Growing Demand for Patient Financing
Emphasizing patient financing as part of the overall experience is powerful. Patients continue to struggle paying for care. Recent granular data details three related forces at work.
Meeting care costs difficult for many patients
Commonwealth Fund found that 42% of individuals had problems paying medical bills or were paying off medical debt during the past year, while 49% were unable to pay an unexpected
$1,000 medical bill.42 Health costs trigger reduction in a range of personal expenditures, led by deferring or avoiding care and drugs (Figure 7).
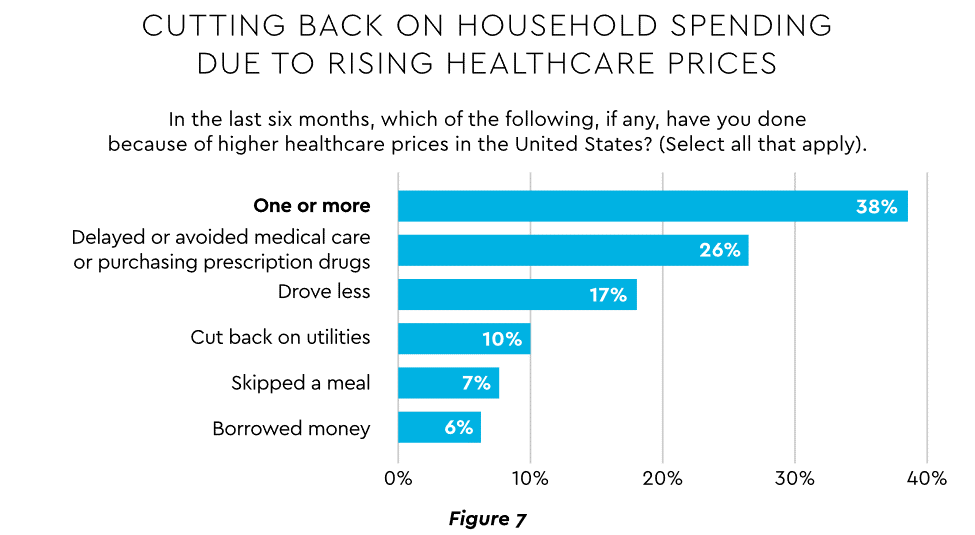
View PDF of Figure 7 chart[PDF]
Twenty-eight percent of Americans now describe themselves as less prepared than last year to pay for routine or unanticipated care.
Patient obligation for care costs still rising
Patient obligation continues its upward march. Insurance premiums have climbed steadily for both the insured and their employers, and employees now pay over $6,000 annually on average for family coverage (Figure 8).45
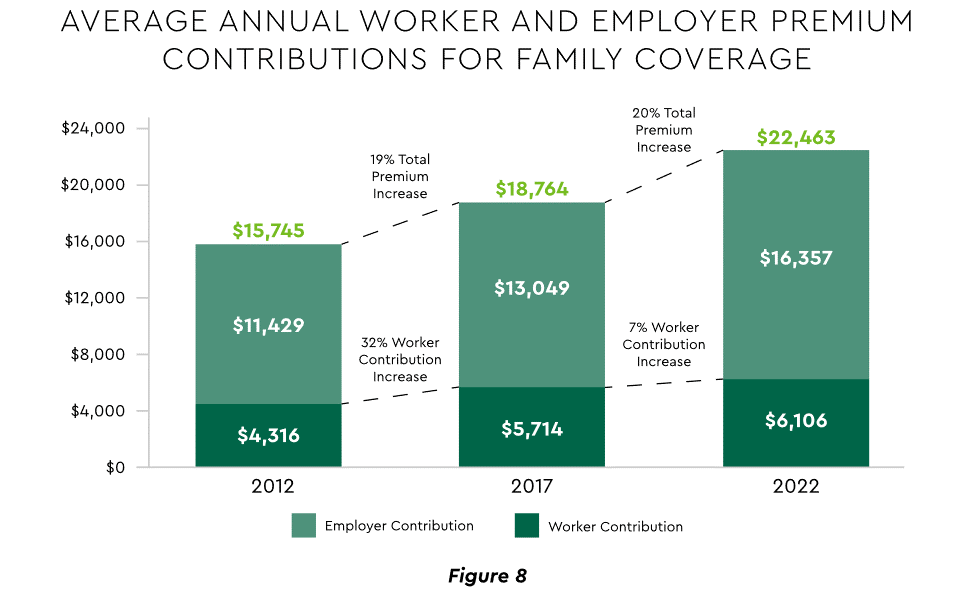
View PDF of Figure 8 chart[PDF]
High deductible health plans (HDHP) also place substantial burden on the patient. Through 2021, 28% of workers were enrolled in an HDHP with an average family deductible of $4,705. Employer satisfaction with these plans is high, auguring further expansion.
Providers feeling the financial effects
Patient payment difficulties are clearly impacting provider financials. A recent in-depth analysis uncovered substantial self-pay issues:
- Self-pay accounts represented 60% of 2021 patient bad debt, up from 11% in 2018.
- Nearly 18% of patient balances were over $7,500 and 17% over $14,000. Collections were noticeably lower at these balances.
Multiple chronic conditions add to the problem. A recent extensive analysis concluded: “Among individuals with medical debt in collections, the estimated amount increased with the number of chronic conditions ($784 for individuals with no conditions to $1,252 for individuals with 7–13).”
For their part, providers will be encouraged to broaden patient financing programs. Patients are certainly interested. When asked, 62% of consumers indicated they would use financing options or creative payment plans if available for large bill amounts. Many health systems, hospitals and practices will turn to outside help to satisfy the demand. A recent analysis recommended that health systems “consider keeping shorter-term payment plans in-house and extended term plans through external partnerships.”
Organizations will also need to step up their communications. A survey revealed that 64% of patients were unaware that their doctors and hospitals offered payment plans or financial help.
5. Building Trust Becoming a Critical Success Factor
Trust has emerged as a paramount issue today for most organizations as they encounter an “imperative to build trust and transparency among different stakeholder groups — employees, customers, suppliers, regulators and the communities in which they operate.” Healthcare is no exception, and the trust issue is growing in both complexity and urgency.
Healthcare’s trust gap
Trust in healthcare took a hit from the COVID-19 experience. A spring 2022 HFMA survey recorded 44% of finance leaders saying they perceived decreased patient trust. Between April 2020 and December 2021, the percentage of Americans who trusted information from doctors “a great deal” declined by 23%, from hospitals 21%, and from nurses 16%. The patient financial experience also faces “drivers of mistrust,” according to surveyed leaders who cited general payment confusion (58%), surprise billing (39%), high prices of commodity items (28%) and lack of price transparency (26%). Building trust reaps dividends. People who trust their providers are five times more likely to stay with them than those who are neutral or distrustful.
Strategies for building trust
Industry experts promote several approaches to galvanize trust among all constituencies:
- Commitment. Embedding trust deeply in the organization requires full support from senior leadership.
- Data transparency and governance. IDC predicts that “by end of 2023, 20% of expenses on care integration solutions will be centered around ‘trust’ to protect data, workflows and transactions.”
- Reliance on fewer business partners. Many health systems, hospitals and practices are reducing their number of vendors in order to focus on a set of trusted long-term partners. For example, almost two-thirds of surveyed providers said they were seeking to streamline the number of software solutions over the next year.
The bank partner advantage
A provider’s banking relationship can yield valuable collaboration in the trust-building endeavor. Banks enjoy solid trust among consumers. As an example, 53.4% of consumers rated banks as most trusted to provide payment “super apps” and financial digital front doors ─ exceeding the next closest source by 10 points.
6. Cybersecurity in 2023: No Rest for the Weary
Cybersecurity is part of the trust calculus and has become an evergreen topic in healthcare. Compromised data and ransomware attacks are ongoing and leaders must continually refine their understanding in at least three areas: the overall security landscape, particular financially related considerations and contemporary security defenses.
The current landscape
The latest statistics quantify the cyber assault on healthcare:
- Incidence. 89% of organizations suffered at least one attack in the past 12 months with the average number at 43.
- Cost. A provider’s most serious attack costs an average of $4.4 million. IBM calculated healthcare’s average total cost of a breach at $10.1 million, up 42% since 2020.
- Attack Characteristics. Healthcare data types most commonly compromised are personal (58%), medical (46%), and credentials (29%). Organizations have an exposure to an average of over 26,000 network-connected devices. A disturbing finding is that those healthcare institutions that paid ransom got back only 65% of their data in 2021.
Specific financial considerations
Finance leaders will also need awareness of the following:
- Cyberattacks could affect credit ratings and are often a component of Environmental, Social and Governance assessments.
- Financial outsourcing requires monitoring. A recent news story chronicled an accounts receivable firm’s breach that exposed individual information, account balances and payments.
- Cyber insurance premiums are likely to increase substantially.
Responses/tools
Beyond a host of management and monitoring tools being deployed, a strategic philosophy is rapidly gaining ground. The “zero trust” model sounds counter to the trust-building mindset described earlier, but it has become essential. It “denies access to applications and data by default,” and 58% of hospitals and health systems have a zero trust initiative in place. Another 37% intend to implement one within 12–18 months.
Cybersecurity investment will challenge CFOs in 2023, especially in areas such as talent. Cybersecurity worker availability is estimated to satisfy only 68% of open positions. Banking partners will also be expected to play an important role. Over the years, major banks have become “leaders in enhancing cyber strategy and investing in cyber defenses, processes and talent.”
7. Digital Transformation of Finance In Focus
Digital transformation is fundamental to healthcare’s business and care delivery model changes. IBM’s website succinctly captures the goal, “Digital transformation means adopting digital-first customer, business partner, and employee experiences.” A leading forecaster believes 70% of healthcare organizations will rely on digital-first strategies by 2027.
Transformation efforts need to accelerate. One study showed that “digital, technology and analytics strategies exist for nearly all organizations, yet only 30% have begun to execute on those plans.”
One functional segment ramping up digital transformation is finance. According to a recent survey, 94% of CFOs and senior leaders stated that such efforts will be at the forefront of financial operations and strategy for 2023–2024, and 79% described it as an “absolute need” for “commercial stabilization and long-term survival of their healthcare organization.”
Advanced technology is gaining traction. Many see optimization in combining robotic process automation (RPA), artificial intelligence and machine learning to create “intelligent automation.” Together, these technologies create algorithms to automate decisions that guide “robotic” software to perform financial actions and thereby reduce manual labor.
Getting to digital-first in finance and across the enterprise has several critical success factors. These include sustained commitment, a platform-centric mindset and effective governance.
Commitment
Some assert that few healthcare executives have “created digital strategies that look far enough into the future.” Speed of change is also important. Health systems, hospitals and practices exhibit varying risk appetites and change rates. When asked to self-identify “transformation personas,” a little over half regarded themselves as being on the innovative “early mover” end of the spectrum, while the remainder will adapt as technologies prove themselves (Figure 9). Slower organizations will likely need to increase the pace.
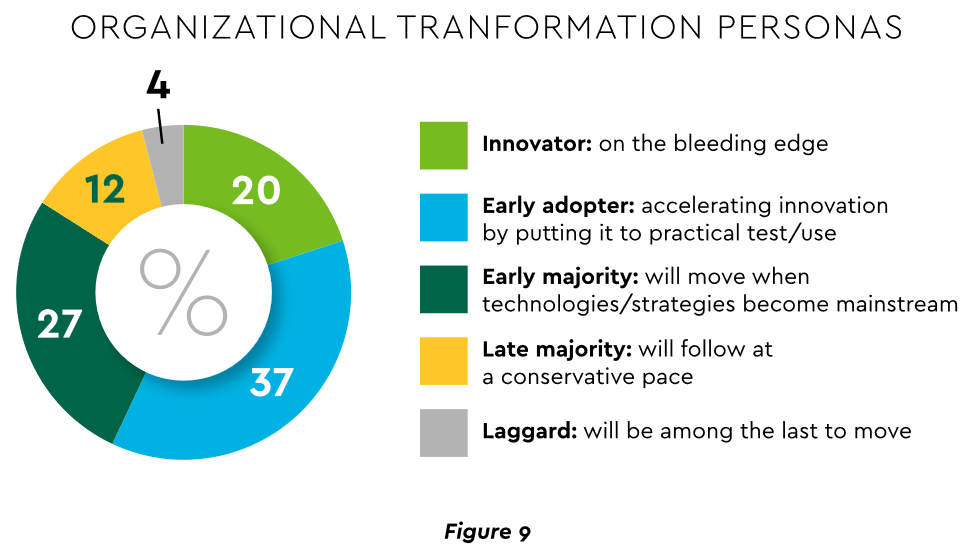
View PDF of Figure 9 chart[PDF]
Platforms, not point solutions
Implementing enterprise platforms rather than proliferating “point solutions” is obligatory. Organizations must be “prepared to compete in the platform economy as platform-based business models have changed the way we live, work and receive care.”
There are still too many tools and applications. A survey of top decision-makers at health systems found that 60% use over 50 software solutions just in operations (24% have over 150). System integration is one answer. Use of application programming interfaces (API) helps this effort substantially. API-first is fast becoming the norm among solution providers, with global API investment expected to nearly triple by 2030 (Figure 10)
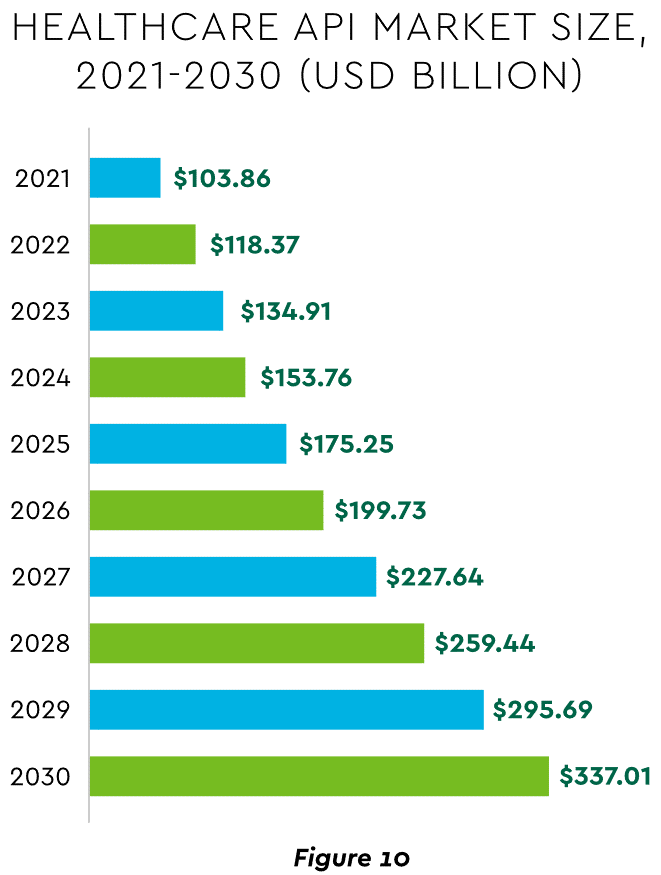
View PDF of Figure 10 chart[PDF]
Governance
Effective governance is vital to constructing a platform-based transformative model and to ensuring wide user adoption. Healthcare has seen the rise of new senior roles such as Chief Digital Officer and Chief Transformation Officer, positions focusing on initiatives like ownership of technology success at the department level and devising user incentives.
8. Digital Payments on the Horizon for Healthcare
A variety of emerging digital payment modes will further the transformation of finance. These payments are expected to grow almost 23% annually in healthcare. ACH payments have been on a strong upward trajectory in healthcare for several years, especially for business transactions. In 2021, ACH tallied a yearly increase of 18% in volume and 5% in dollars.
Notable technologies and payment rails to watch for expected crossover from consumer markets to healthcare include:
- Mobile payments. The market for mobile payment technologies has been growing at a 16% compound annual clip and should reach $90 billion in 2023, powered by wide smartphone use, 5G networks and convenience. This category encompasses technologies such as e-wallets, forecasted to grow 23% annually worldwide through 2030.
- Real-time payments (RTP). These digital transactions are settled nearly instantaneously through platforms such as The Clearing House. One forecast sees 30.4% compound RTP growth in the U.S. from 2022 to 2030.
- Buy Now Pay Later (BNPL). This growing mode offers consumers short-term financing to stretch payments over several installments. A recent survey established that 23% of American adult respondents have used a BNPL service. BNPL is just entering healthcare and is currently regarded as an option for certain elective or cosmetic procedures or for specific individual credit scenarios.
- Earned Wage Access (EWA). Using an RTP approach, employers are beginning to offer on-demand pay which enables “instant access to earned wages right after the work is performed, at the end of the shift, or upon completion of a project.” It is not a loan or advance pay. A 2021 poll conducted by Harris found that 83% of U.S. workers feel they should be able to access earned wages at the end of each day. Millennials were particularly interested: 80% would like daily automatic pay streaming to their bank accounts, and 78% said free EWA would boost loyalty to their employer. Given its pressing workforce concerns, healthcare is likely to find EWA a tool to promote retention.
Seeking the right use cases for these payment technologies offers many potential provider benefits.
Conclusion
The connected forces discussed and quantified here create major challenges to address in 2023. The strategic agenda calls for balancing tight cost control with investment in growth opportunities, significantly enhancing patient financial experience by meeting growing patient financial need, shoring up trusted relationships and cybersecurity, and accelerating the digital transformation of finance.
What CEOs want CFOs to focus on

Fifty-four percent of CFOs say that their CEOs are asking them to focus on cost reduction while 40 percent indicate that their CEOs want them honing in on strategy and transformation, according to Deloitte’s “CFO Signals Survey 2Q 2023.”
More than one-quarter of CFOs in the survey reported that their CEOs are asking them to focus on working capital efficiency and risk management while over one-third of CFOs said their CEOs want them focused on strategy and transformation, performance management, revenue growth, investment and capital/financing.
Since 2010, Deloitte has surveyed leading CFOs representing some of North America’s largest companies to provide insight into the business environment, company priorities and expectations, finance priorities and CFOs’ priorities.
Participating CFOs represent diversified, large companies, with 81 percent of respondents reporting revenue in excess of $1 billion. Twenty-three percent are from companies with more than $10 billion in annual revenue, according to Deloitte.
When Financial Performance Matters
https://www.kaufmanhall.com/insights/thoughts-ken-kaufman/when-financial-performance-matters

The Sunk Cost Fallacy
In behavioral economics, the sunk cost fallacy describes the tendency to carry on with a project or investment past the point where cold logic would suggest it is not working out. Given human nature, the existence of the sunk cost fallacy is not surprising. The more resources—time, money, emotions—we devote to an effort, the more we want it to succeed, especially when the cause is an important one.
Under normal circumstances, the sunk cost fallacy might qualify as an interesting but not especially important economic theory. But at the moment, given that 2022 will likely be the worst financial year for hospitals since 2008 and given that the hospital revenue/expense relationship seems to be entirely broken, there is little that is theoretical about the sunk cost fallacy. Instead, the sunk cost fallacy becomes one of the most important action ideas in the hospital industry’s absolutely necessary financial recovery.
Historically, cases of the sunk cost fallacy can be relatively easy to spot. However, in real time, cases can be hard to identify and even harder to act on. For hospital organizations that are subsidizing underperforming assets, identifying and acting on these cases is now essential to the financial health of most hospital enterprises.
For example, perhaps the asset that is underperforming is a hospital acquired by a health system. (Although this same concept could apply to a service line or a related service such as a skilled nursing facility, ambulatory surgery center, or imaging center.) The costs associated with integrating an acquired hospital into a health system are typically significant. And chances are, if the hospital was struggling prior to the acquisition, the purchaser made substantial capital investments to improve the performance.
As time goes on, if the financial performance of the entity in question continues to fall short, hospital executives may be reluctant to divest the asset because of their heavy investment in it.
This understandable tendency can lead the acquiring organization to throw good money after bad. After all, even when an asset is underperforming, it can’t be allowed to deteriorate. In the case of hospitals, that’s not just a matter of keeping weeds from sprouting in the parking lot. The health system often winds up supporting an underperforming hospital with both working capital and physical capital, which compounds the losses.
And the costs don’t stop there, because other assets in the system are supporting the underperforming asset. This de facto cross-subsidy has been commonplace in hospital organizations for decades. Such a cross subsidy was probably never sustainable, but it is even less so in the current challenging financial environment.
This is a transformative period in American healthcare, when hospital organizations are faced with the need to fundamentally reinvent themselves both financially and clinically. The opportunity costs of supporting assets that don’t have an appropriate return are uniquely high in such an environment. This is true whether the underperforming asset is a hospital in a smaller system, multiple hospitals in a larger system, or a service line within a hospital.
The money that is being funneled off to support underperforming assets may be better directed, for example, toward realigning the organization’s portfolio away from inpatient care and toward growth strategies. In some cases, the resources may be needed for more immediate purposes, such as improving cash flow to support mission priorities and avoiding downgrades of the organization’s credit rating.
The underlying principle is straightforward:
When a hospital supports too many low-performing assets, the capital allocation process becomes inefficient. Directing working capital and capital capacity toward assets that are dilutive to long-term financial success means that assets that are historically or potentially accretive don’t receive the resources they need to grow and thrive. The underlying principle is a clear lose-lose.
In the highly challenging current environment, it is especially important for boards and management to recognize the sunk cost fallacy and determine the right size of their hospital organizations—both clinically and financially.
Some leadership teams may determine that their organizations are too big, or too big in the wrong places, and need to be smaller in order to maximize clinical and balance-sheet strength. Other leadership teams may determine that their organizations are not large enough to compete effectively in their fast-changing markets or in a fast-changing economy.
Organizational scale is a strategy that must be carefully managed. A properly sized organization maximizes its chances of financial success in this very difficult inflationary period. Such an organization invests consistently in its best performing assets and reduces cross-subsidies to services and products that have outlived their opportunity for clinical or financial success.
Executives may see academic economic theory as arcane and not especially relevant. However, we have clearly entered a financial moment when paying attention to the sunk cost fallacy will be central to maintaining, or recovering, the financial, clinical, and mission strength of America’s hospitals.
The false promise of “no regrets” investments
https://mailchi.mp/a93cd0b56a21/the-weekly-gist-june-9-2023?e=d1e747d2d8

At the end of a meeting last week with a health system executive team, the system’s COO asked us a question: “Your concept of a consumer-focused health system centered around treating patients as members describes exactly how we want to relate to our patients, but we’re not sure about the timing. Could you give us a list of the ‘no regrets’ investments you’d recommend for health systems looking to do this?”
We frequently get asked about “no regrets” strategies:
decisions or investments that will be accretive in both the current fee-for-service system as well as a future payment and operational model oriented around consumer value. The idea is understandably appealing for systems concerned about changing their delivery model too quickly in advance of payment change. And there is a long list of strategies that would make a system stronger in both fee-for-service and value: cost reduction, value-driven referral management, and online scheduling, just to name a few.
But as we pointed out, the decision to pursue only the no-regrets moves is a clear signal that the organization’s strategy is still tied to the current payment model.
If the system is truly ready to change, strategy development should start with identifying the most important investments for delivering consumer value. It’s fine to acknowledge that a health system is not yet ready, but we cautioned the team that they should not rely on the external market to provide signals for when they should undertake real change in strategy.
External signals—from payers, competitors, or disruptors—will come too slowly, or perhaps never. At some point, the health system should be prepared to lead innovation, introduce a new model of value to the market, and define and promote the incentives to support it.
Real change will require disruption of parts of the current business and cannot be accomplished with “no-regrets investments” alone.

