https://www.fiercehealthcare.com/payer/5-takeaways-from-cbo-s-analysis-a-single-payer-system?mkt_tok=eyJpIjoiTURRNU5HTmpZbU5tT1RFeiIsInQiOiJLcVdxN0dKUU5iaEdMTGtaMG9xbFdtdEgxdXJBbndhTUNyMWN6UTZzbGJhTHFkS3Z4eTRBZkFGNUxcLzlyZUxvMHpOUDRDbmptdGE4aHVoMk4wS1NTYUlWMFVPMmFxNEEzTkJcL1RDODhYa3psN0VkNFhFdTVqYjlDSHltaTdPMUFxIn0%3D&mrkid=959610

As chatter about “Medicare-for-All” ideas heats up—at least among the field of Democratic presidential hopefuls—the Congressional Budget Office decided to offer its own take.
Well, sort of.
Wednesday, the CBO issued a report that dove into the key considerations policymakers might want to think about before they overhaul the U.S. healthcare into a single-payer system. Putting it mildly, they said, the endeavor would be a “major undertaking.”
They don’t actually offer up specific cost estimates on any of the Medicare-for-All bills floating around, though other researchers put Bernie Sanders’ Medicare-for-All plan at between $32.6 trillion and $38.8 trillion over the first decade.
But the CBO analysts did weigh in on a slew of different approaches to financing, coverage, enrollment and reimbursement that could be built into a single-payer plan.
“Establishing a single-payer system would be a major undertaking that would involve substantial changes in the sources and extent of coverage, provider payment rates and financing methods of healthcare in the United States,” the CBO said.
So what exactly did the CBO have to say about what it would take to create a single-payer system? Here are some key takeaways:
1. There could be a role for private insurance—or not
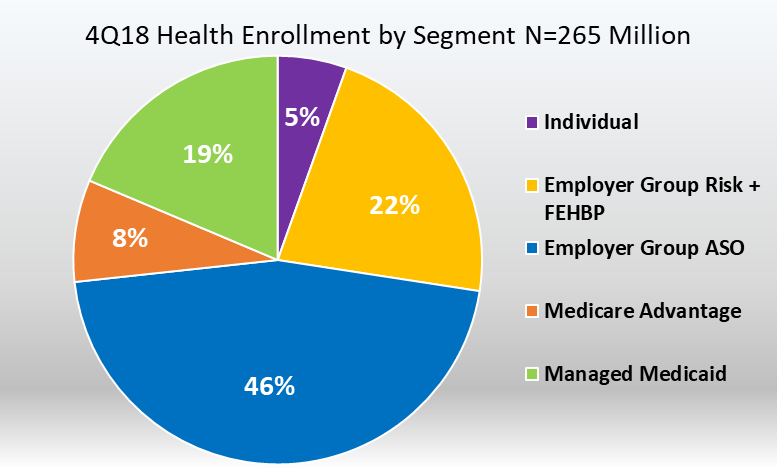
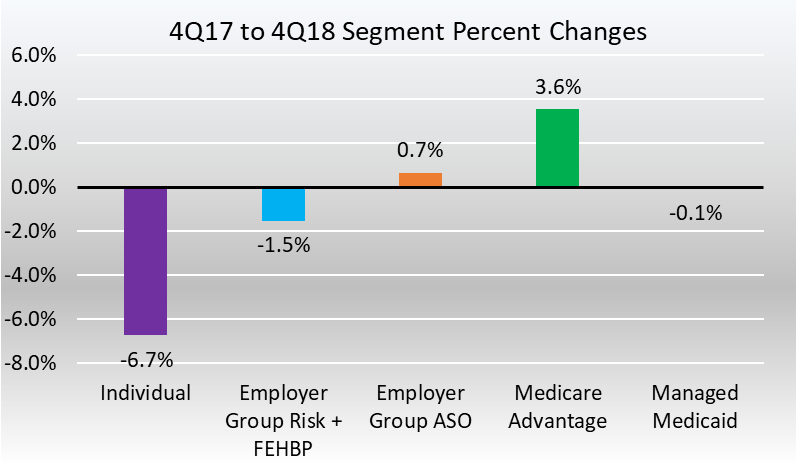
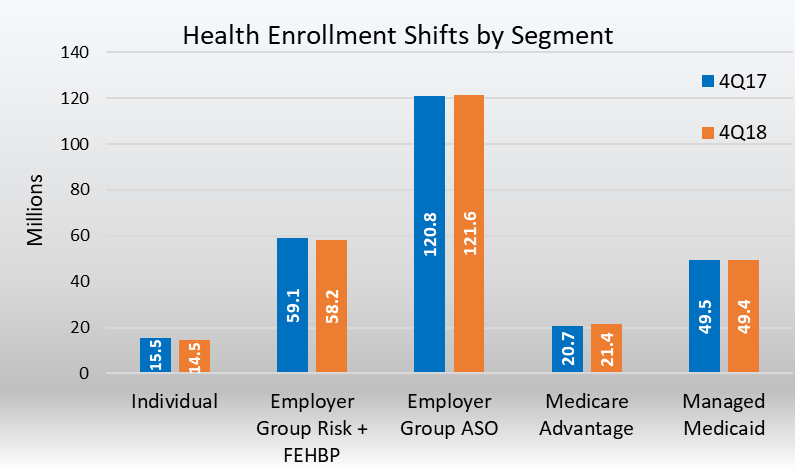
There has been plenty of heated debate around Medicare for All focused on the role that existing private coverage could—or could not—play in that system. Most insured Americans are enrolled in a private plan today, including about one-third of Medicare beneficiaries.
If they’re allowed, commercial plans could play one of three roles in a single-payer system, according to the report: as supplemental coverage, as an alternative plan or to offer “enhanced” services to members in the government plan.
Allowing private insurers to offer substitutive plans is unlikely, because they could potentially offer broader provider networks or more generous benefits, which would draw people into them. A solution to this issue could be mandating that providers treat a minimum number of patients who are enrolled in a single-payer plan.
Private payers could also offer coverage for care that is traditionally outside of the purview of government programs, such as dental care, vision care and hearing care.
Supplemental plans like these are offered in the existing Medicare program, and several countries with single-payer systems allow this additional coverage.
For example, in England, private plans offer “enhancements” to members of the government plan, including shorter wait times and access to alternative therapies, But members of these plans must pay for it in addition to tax contributions to the country’s National Health Service.
2. Other government programs could stick around
In addition to Medicare and Medicaid, the federal government operates several health programs targeting individual populations: the Veterans Affairs health system, TRICARE and Indian Health Services.
A single-payer system could be designed in a way that also maintains these individualized programs, the CBO said. Canada does this today, where its provinces operate the national system while it offers specific programs outside that for indigenous people, veterans, federal police officers and others.
There could also be a continuing role for Medicaid, according to the report.
“Those public programs were created to serve populations with special needs,” the CBO said. “Under a single-payer system, some components of those programs could continue to operate separately and provide benefits for services not covered by the single-payer health plan.”
On the flip side, though, a single-payer plan could choose to fold members of those programs into the broader, national program as well, the office said.
3. A simplified system could also mean simplified tech
Taiwan’s government-run health system has a robust technology system that can monitor patients’ use of services and healthcare costs in near real-time, according to the report.
Residents are issued a National Health Insurance card that can store key information about them, including personal identifiers, recent visits for care, what prescriptions they use and any chronic conditions they may have. Providers also submit daily data updates to a government databank on service use, which is used to closely monitor utilization and cost. Other technology platforms in Taiwan can track prescription drug use and patients’ medical histories.
However, getting to a streamlined system like this in the U.S. would be bumpy, the CBO said. It would face many of the same challenges the health system is already up against today, such as straddling many federal and state agencies and addressing the needs of both rural and urban providers.
But the payoffs could be significant, according to the report.
“A standardized IT system could help a single-payer system coordinate patient care by implementing portable electronic medical records and reducing duplicated services,” the agency wrote.
4. How to structure payments to providers? Likely global budgets
Most existing single-payer systems use a global budget to pay providers, and may also apply in tandem other payment approaches such as capitation or bundled payments according to the report.
How these global budgets operate varies between countries. Canada’s hospitals operate under such a model, while Taiwan sets a national healthcare budget and then issues fee-for-service payments to individual providers. England also uses a national global budget.
Global budgets are rare in the U.S., though Maryland hospitals operate under an all-payer system. These models put more of the financial risk on providers to keep costs within the budget constraints.
Many international single-payer systems pay based on volume, but the CBO said value-based contracting could be built into any of these payment arrangements.
5. Premiums and cost-sharing are still in play, especially depending on tax structures
A government-run health system would, by its nature, need to be funded by tax dollars, but some countries with a single-payer system do charge premiums or other cost-sharing to offset some of those expenditures.
Canada and England operate on general tax revenues, while Taiwan and Denmark include other types of financing. Danes pay a dedicated, income tax to back the health system, while the Taiwanese have a payroll-based premium.
The type of tax considered would have different implications on financing, according to the CBO. A progressive tax rate, for instance, would impose higher levies on people with higher incomes, while a consumption tax, such as one added to cigarettes, would affect people more evenly.
Policymakers will also have to weigh when to impose new taxes, shifting the economic burden between generations.
The CBO did not offer any cost estimates in terms of the amount the federal government would need to raise in taxes to fund a single-payer program.