http://khn.org/news/big-employers-embrace-health-plan-status-quo/

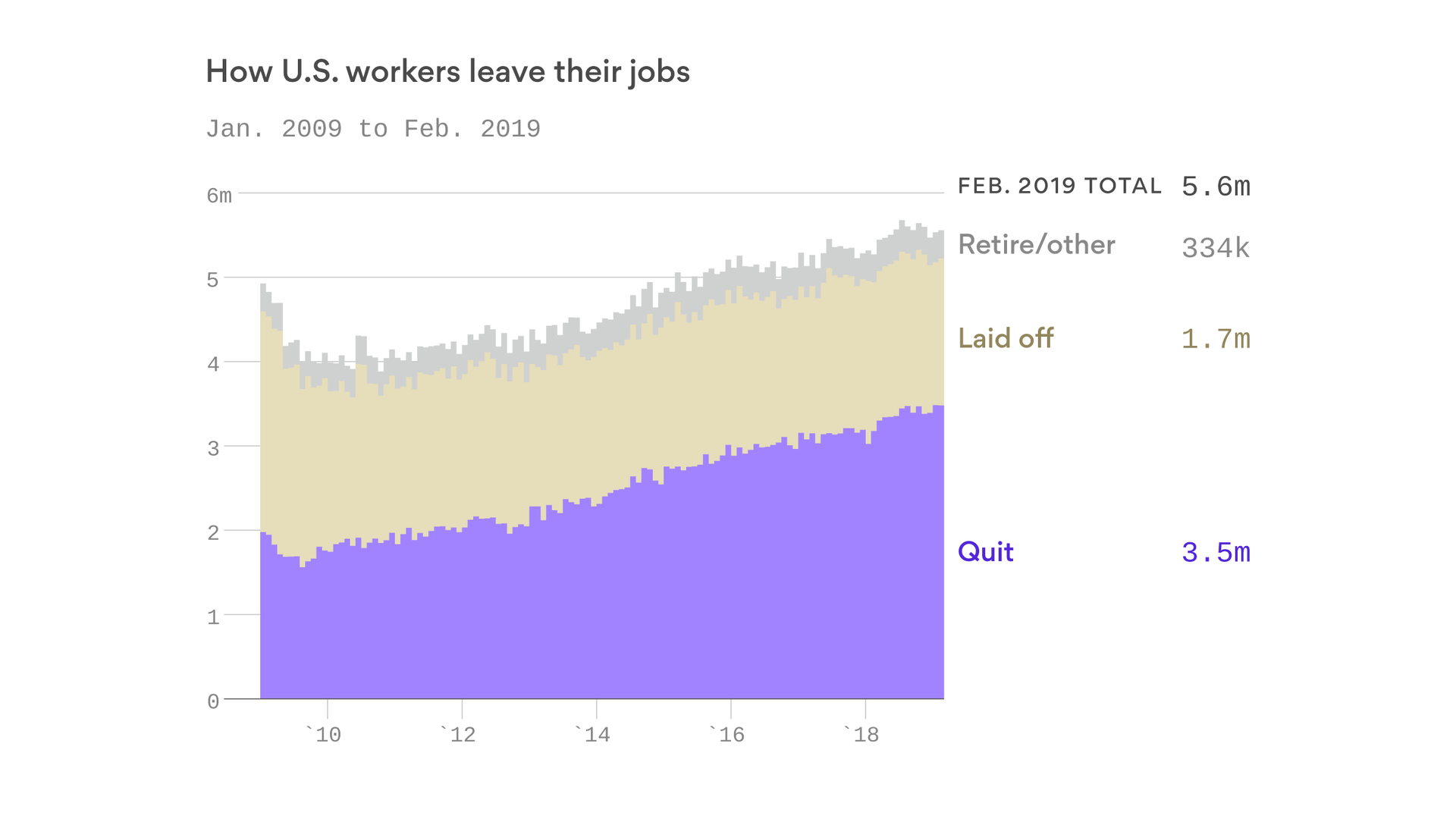
The shrinking unemployment rate has been a healthy turn for people with job-based benefits.
Eager to attract help in a tight labor market and unsure of Obamacare’s future, large employers are newly committed to maintaining coverage for workers and often their families, according to new research and interviews with analysts.
Two surveys of large employers — one released Aug. 2 by consultancy Willis Towers Watson and the other out Tuesday from the National Business Group on Health, show companies continue to try to control costs while backing away from shrinking or dropping health benefits. NBGH is a coalition of large employers.
“The extent of uncertainty in Washington has made people reluctant to make changes to their benefit programs without knowing what’s happening,” said Julie Stone, a senior benefits consultant with Willis Towers Watson. “They’re taking a wait-and-see attitude.”
That’s a marked change from three years ago, when many big employers — those with 1,000 employees or more — contemplated ending medical benefits and shifting workers to the Affordable Care Act’s marketplaces.
In 2014, only 25 percent of big companies were “very confident” they would have a job-based health plan for employees in 10 years, according to the Willis Towers Watson survey.
This year, 65 percent expected to offer health benefits in a decade. And 92 percent said they were very confident a company-based health plan would exist in five years.
Many managers once eyed Obamacare marketplaces as workable coverage alternatives despite the law’s requirement that employers offer health insurance, analysts said.
But problems with marketplace plans, including fewer offerings, rising premiums and shrinking medical networks, have made employers think twice, they said.
Another big reason to maintain rich coverage is “the strength of the economy,” said Paul Fronstin, director of health research at the Employee Benefit Research Institute, an industry group. “Employers are doing what they have to do to get the right workers.”
Unemployment has fallen from 9.9 percent when Obamacare became law in 2010 to 4.3 percent last month, which equaled a 16-year low reached in May.
With such a steep decline, he added, “employers are thinking, ‘We need to offer this benefit for recruitment and retention.’”
Second Thoughts On High-Deductible Plans
Companies are even rethinking the long-standing expedient of shifting a portion of rising medical costs to employees through high-deductible plans and a greater share of the premium bill, other research shows.
“Employers are beginning to recognize that cost sharing has its limits,” said a June report from PwC, a multinational professional services network. Low unemployment and competition for workers mean “employers have less appetite for scaling back benefits and continuing with a plan design that has proven largely unpopular.”
At Fidelity Investments, a Boston-based financial firm with more than 45,000 employees, worker contributions have grown to about 30 percent of total health costs.
Jennifer Hanson, the company’s benefits chief who sits on NBGH’s board, doesn’t see that continuing.
As costs grow, “if you continue to shift more of a bigger number to employees, health care becomes unaffordable,” she said in an interview. “As employers, we really do need to pay attention less to who’s paying for what and more to how much everything costs.”
More than half of Americans with job-based insurance face deductibles — out-of-pocket costs for most care before insurance kicks in — of more than $1,000 for single-person coverage. Family deductibles can be much higher.
High On The To-Do List: Controlling Drug Costs
Big employers’ planned changes for next year focus on controlling drug costs and improving health results through telemedicine and steering patients to efficient, high-quality hospitals, noted the Willis Towers Watson report and the NBGH survey.
Employer health costs continue to rise, but not at the double-digit clip seen for many plans sold to individuals and families through the ACA marketplaces.
Employers expect health costs to increase 5.5 percent next year, up from 4.6 percent in 2017, according to the Willis Towers Watson report.
Companies in the NBGH survey predicted health costs will rise 5 percent next year, up from an average 4.1 percent increase for 2016.
That’s still far faster than inflation, which is less than 3 percent, and overall wage growth.
By many accounts, soaring costs for specialty pharmaceuticals used to treat cancer, rheumatoid arthritis, hemophilia and other complex conditions are the biggest factor.
“These are very expensive drugs,” said Brian Marcotte, NBGH’s CEO. “They cost thousands or tens of thousands per treatment.”
Often these drugs require infusion into the blood in a clinical setting, which can drive up their price tag.
For instance, hospital-based infusions have been found to cost as much as seven times more than those performed in, say, a doctor’s office.
Employers are working hard to steer patients to the least expensive, appropriate site, Marcotte said.
Big employers are also offering more on-site nurses and doctors; setting up accountable care organizations with incentives for doctors and hospitals to control costs; and striking deals with particular hospitals for high-cost operations such as transplants and joint replacements, the NBGH survey found.
Job-based insurance covers some 160 million people younger than 65, according to Census and Labor Department data, far more than the 10 million or so insured by plans sold through Obamacare marketplaces.
Government employers and companies with at least 500 workers, which historically have been more likely to offer health benefits than smaller employers, cover more than 90 million employees and dependents.
Willis Towers surveyed 555 large employers with about 12 million workers and dependents. NBGH surveyed 148 large companies with more than 15 million employees and dependents.