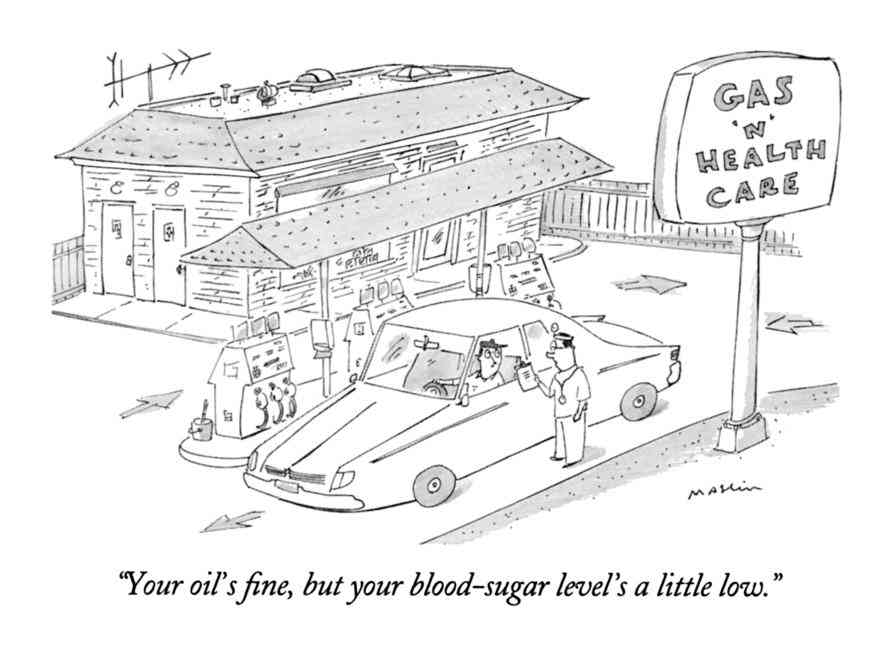
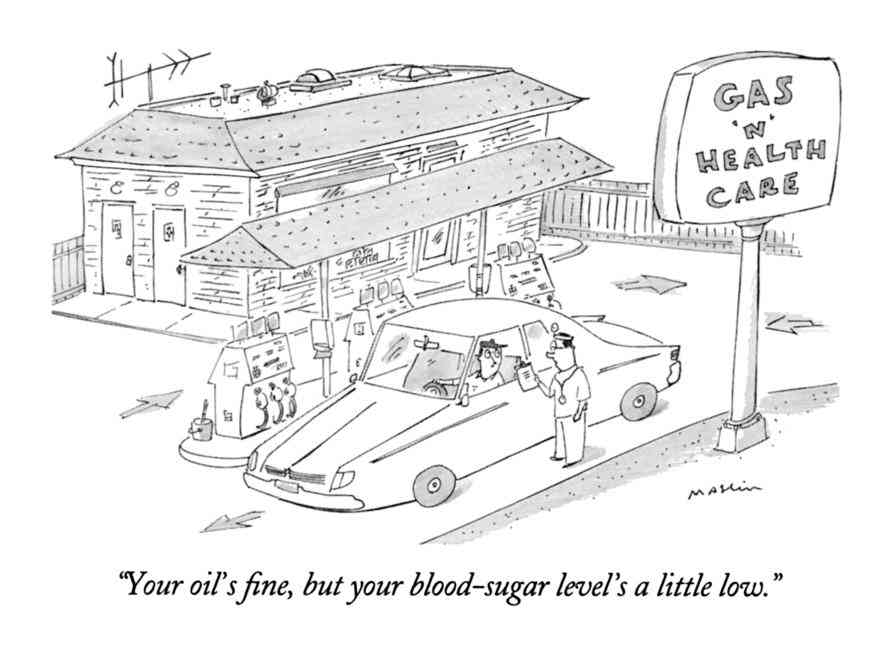
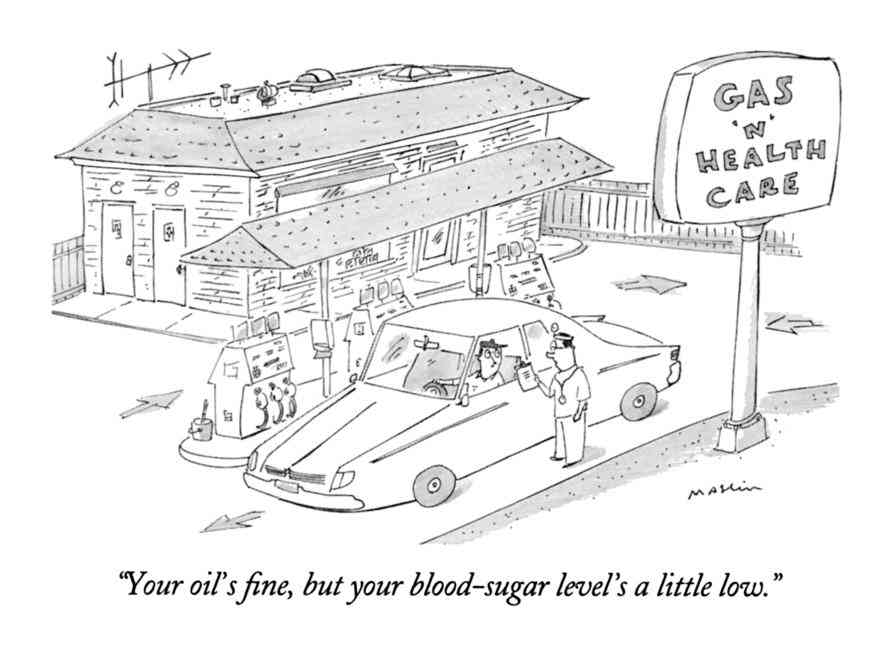
Cartoon – Retail Healthcare
Colleen Blye serves as executive vice president and CFO of New York City-based Montefiore Health System.
Before joining the system in January 2016, she was executive vice president and CFO of Catholic Health Services of Long Island, an integrated healthcare delivery system based in Rockville Centre, N.Y.
She was also executive vice president for finance and integrated services at Englewood, Colo.-based Catholic Health Initiatives.
Here, Ms. Blye shares her proudest moment as Montefiore’s CFO, discusses her daily mantra and reveals the revenue cycle tools she’s most excited about.
Question: Since joining Montefiore, what has been one of your proudest moments as CFO?
Colleen Blye: When we restructured the balance sheet last year and [pursued] public financing. This was the first time in Montefiore’s history that we went for a public rating. As a result, this refinancing provided much needed liquidity for our system, and it allowed us to level debt service. We now have a solid baseline going forward which offers us access to additional financing, as needed. That was a big deal and positions our organization with a debt structure appropriate for a system of our size and scale.
Q: What is the greatest challenge you faced as CFO in 2018? Do you expect this to be your biggest challenge in 2019 as well?
CB: One [challenge] is shifting the finance culture overall from one of financial reporting to one of analytics, and being a business partner. In today’s healthcare world, I think this is imperative, and Montefiore has embraced this culture. I think businesses separate from the healthcare environment operate this way, and we need to be responding and shifting so that finance is a true business partner throughout the organization.
The other aspect that I think is increasingly challenging for all of us in financial healthcare is trying to understand how to diversify our shrinking revenue base. There’s been a lot of revenue compression by governmental payers and the market in general. Therefore, it is imperative that we continually think about how we’re going to diversify that revenue base and bring in new revenue streams to facilitate growth.
Q: What is a daily mantra that informs your leadership decisions?
CB: I always use the concept, “Leave an organization better than you received it.” That doesn’t always mean having absolute analytics or support. Seasoned CFOs understand [that] you must use your experience and other intellect, in addition to data and supporting analysis, to determine whether the risk of any given business decision is worthwhile going forward.
Q: Montefiore Health System has 11 hospitals and serves 3 million people in communities across the Bronx, Westchester and the Hudson Valley. How does the system’s financial strategy differ by location?
CB: At the highest level, we are one system. However, every market has different opportunities, and it’s imperative that we find those opportunities and capitalize on them to benefit the patients, providers, communities, and therefore, the system overall.
Q: The system is bringing specialty care expertise in areas including cancer, advanced imaging, neuroscience, transplantation, musculoskeletal and heart and vascular care to new markets in its service region of four counties. How does this play a role in the system’s financial improvement plans?
CB: It’s certainly a big part. This goes back to diversifying the revenue stream and understanding where those opportunities are. Specialty care is a critical element of the future of healthcare. We’ve seen a significant shift from inpatient to outpatient care for the less complex services. But,it’s equally important to understand the more complex care as well, capturing that environment so we can take care of the whole person. From an economic point of view, it typically is that more complex care that produces some of the greater margins for our organization.
Q: What are your top cost containment strategies?
CB: We’re focused on all opportunities. One challenge many organizations have is to maintain a cost-focused culture while you’re trying to support growth to sustain the business. But we look at all aspects — how do we maintain our quality care yet utilize our size and scale to get efficiency? We’re constantly looking at that as it relates to our procurement strategy. We’re constantly looking at our employee and benefit cost structure. We [must] continually look at that resource consumption and make sure we’re spending wisely. As a system, our goal is to make sure that quality care is at the center of what we’re focused on but that we utilize who we are — scale and size — to maximize opportunities.
It’s [also] not just the cost side of the equation that we look at. To grow and sustain, we also have to grow our business. We have to be equally focused on where those growth opportunities lie for us as an organization, maintaining equal focused on our revenue efficiency to make certain we’re collecting every dollar we’re entitled to for the services we deliver.
Q: What new revenue cycle tool are you most excited about?
CB: The tools we’re most excited about are those that are patient-focused. Consumers, particularly millennials, expect and look for that convenience. We are working with vendors that transition a complex billing and information cycle. This enables us to communicate with our patients in a far more user-friendly way, We’re excited about these opportunities which are focused on patient-centered communications, allowing us to connect directly with patients, informing them at the earliest point about what their financial responsibilities are, how to interpret that information, and how to make payments on those responsibilities.
Q: If you could pass along one nugget of advice to another hospital CFO, what would it be?
CB: Always keep your eyes and ears open for opportunities and always think about how you can grow and expand your thinking and the perspective you bring to the work that you do.
I would also encourage thinking about how to become partners in the healthcare business. I think we have a calling now as CFOs to be far more involved in operations, rather than just financial reporting, providing data, trends and insight to our internal colleagues. I would really suggest moving from the traditional finance acumen to use those skills and techniques to be a strategic-thinking and better business partner.

Patient consumer metaphors place “disproportionate burdens” on patients to solve healthcare’s cost and quality issues, researchers wrote in a blog post published by Health Affairs.
Academics from the Hastings Center, a nonprofit bioethics research institute in Garrison, N.Y., wrote that patient-centered care messages have begun to mesh with patient consumerism. The authors note while patient advocates began using consumerism as a means to challenge corporate and professional dominance in healthcare, “today, ‘consumer-driven’ healthcare has become associated with neoliberal efforts to emphasize market factors in health reform and de-emphasize government regulation and financing.”
The authors continue: “In our view, a narrow focus on consumerism is conceptually confused and potentially harmful. The consumer metaphor wrongly assumes that healthcare is a market in the usual understanding of that term, that the high cost of U.S. healthcare is a function of excessive consumer demand, and that price transparency and competition can deliver on the promise of reducing costs or ensuring quality.”
The researchers concluded if the consumer metaphor continues, they believe patient-centered approaches, which can lead to improvements in healthcare, would be undermined.

The shift in health care from volume-based, fee-for-service to value-based reimbursement (VBR) continues to push forward. In its wake, unintended consequences and new challenges have emerged — not only in aspects of delivery but also when determining fair market value (FMV) and remaining compliant with the federal Anti-Kickback Statute and the Stark Law. Below we touch on those consequences and how they’ve emerged from both new and old regulations.
Now in play, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) promises to fundamentally change the way the country evaluates and pays for health care. Its new payment schedules, however, have created ramifications that not only tangle the hospital-physician relationship but also create implications for VBR transactions and valuations.
As part of the transition to value-based medicine, four new MACRA elements in particular represent significant changes:
1. Pay for Performance (P4P) Arrangements: The remuneration system makes part of payment dependent on performance, measured against a defined set of criteria, and creates measurements and performance standards for establishing target criteria.
2. Shared Savings Arrangements: The new approach incentivizes providers to reduce health care spending for a defined patient population by offering a percentage of net savings realized as a result of their efforts.
3. Episodic Payments: An episode payment system offers a single price for all the services needed by a patient for an entire episode of care; for example, all the inpatient and outpatient care needed following a heart attack. The intent is to reduce the incentive to overuse unnecessary services within the episode. It also gives health care providers the flexibility to decide what services should be delivered rather than constraining them by fee codes and amounts.
4. Global Budget: With a fixed prepayment made to a group of providers or to a health care system (as opposed to a health care plan), this arrangement covers most or all of a patient’s care during a specified time period.
Clearly the value equation is shifting. Value is defined no longer solely by how much revenue a physician generates but rather by solving problems for patients and patient experience. Value can also be derived not by revenue per patient, but by how many patient lives a physician directs, and with that comes control over how some payments are allocated for patient related services.
As the value dynamics change, hospitals have sought to establish closer relationships with physicians. Acquisitions of physician practices by hospitals have continued at dramatic rates alongside the move toward direct physician employment and provider service agreements. New players in the market and marketplace forces have also emerged as competition to hospitals. Private equity groups and insurance companies are pursuing the acquisition of physicians and clinics for control of patient lives, and therefore revenue.
While the trend toward hospital-physician alignment is intended to improve health care delivery, it has come under scrutiny for potential fraud and abuse violations due in part to established laws that now appear at odds with the new VBR movement.
Health care organizations, providers and their counsels are well aware of the laws in place they must abide by, namely the Anti-Kickback Statute (AKS) and the Stark Law, which have been in force for more than three decades.
Such regulatory considerations related to fraud and abuse have long had significant impact on the value attributable to each property interest and on the valuation process itself. There are in fact several distinct meanings of fraud within the context of the health care regulatory framework, and they affect a property’s profitability and sustainability, creating significant risk and uncertainty for business entities.
What constitutes fraud, however, is now under the microscope and creating potential liability under the False Claims Act. The new direction of collaborative relationships on behalf of the patient and patient outcomes can make some arrangements suspect. How do physicians refer patients in the new MACRA environment without it being considered a conflict of interest or fraudulent? How will payments made to physicians not exceed the range of FMV and be deemed commercially reasonable? How can alignment strategies be constructed to provide a full continuum of care under VBR reforms?
While there have been no changes to the longstanding regulations, discord between the old laws and the new VBR direction is necessitating a different approach to compliance. The American Hospital, in a letter to the U.S. Senate Finance Committee in a hearing on the Stark law, said, “As interpreted today, the two ‘hallmarks’ of acceptability under the Stark law — fair market value and commercial reasonableness — are not suited to the collaborative models that reward value and outcomes.”
The friction between the enforcement of fraud and abuse laws by the Department of Justice and the Office of the Inspector General, and the VBR models being implemented by Health and Human Services is warranting a review of MACRA and the threshold and definition of commercial reasonableness. With no one clear definition of commercial reasonableness, its analysis is ripe for distortion.
Many regulators’ arguments are centered around Practice Loss Postulate (PLP) — that the acquisition of a physician practice that then operates at a “book financial loss” is dispositive evidence of the hospital’s payment of consideration based on the volume and/or value of referrals.
The problem? In maintaining the economic delineation between physicians and hospitals, the PLP focuses exclusively on immediate and direct financial (cash) returns on, and returns of, investments by health care organizations related to vertical integration transactions. The PLP ignores other economic benefits associated with vertical integration, such as social benefits, qualitative gains, efficiency gains and avoiding costs.
As a consequence, such a vertical integration move could be viewed by regulators as evidence of legally impermissible referrals under the Stark law. However, it would prevent vertically integrated health systems from withstanding fraud and abuse scrutiny. And it would create barriers to satisfying the threshold of commercial reasonableness.
Active industry input and congressional committee discussion is underway in hopes of generating workable strategies to reduce the law’s burden. And although the actual outcomes are uncertain, changes are clearly ahead.
Click to access CBC_59_032719.pdf

Funded by Private Equity, the ongoing consolidation of solo and small-group physician practices into Physician Practice Management organizations reflects a maturing healthcare marketplace that is repositioning to deliver single specialty care services in retail settings.
Time is running out for solo and small group practices. To position themselves for successful consolidation transactions now and in the future, operators and buyers need to understand the fundamental market dynamics shaping valuations.

Today’s Medicare Advantage plans are flourishing and the Silver Tsunami is among the reasons.
“Over the last four years, Medicare Advantage enrollment increased by more than 30 percent, while the number of people eligible for Medicare grew by about 18 percent,” said Steve Warner, vice president of Medicare Advantage Product for UnitedHealthcare Medicare and Retirement.
Other reasons for the growth: Innovative models from big insurers and upstarts alike that improve care for health plan members and drive revenue for payers as they look beyond fee-for-service.
IT STARTS WITH THE CONSUMER
Consumers are finding unique value in MA, both in terms of the quality of care and in the financial value.
Medicare Advantage, in fact, makes it easier for consumers to navigate the healthcare system and choose providers, in a way that traditional Medicare does not, said those interviewed.
“Actually it’s pretty hard to navigate the healthcare system on your own,” said Tip Kim, chief market development officer at Stanford Health Care. “Most Medicare Advantage plans have some sort of care navigation.”
Warner of UnitedHealth’s Warner added that Medicare Advantage also offers value and simplicity.
“It provides the convenience of combining all your coverage into one plan so you have just one card to carry in your wallet and one company to work with,” Warner said. “Most plans also offer prescription drug coverage and additional benefits and services not available through original Medicare, including dental, vision and fitness.”
REBRANDING FOR THE NEW ERA
MA plans did not emerge out of thin air. By another name, Medicare Advantage is managed care, a term that was the bane of healthcare during the height of HMOs in the 1980s.
“Medicare Advantage has rebranded ‘managed care’ to ‘care coordination,'” said consultant Paul Keckley of The Keckley Report. “Humana and a lot of these folks have done a pretty good job. Coordinating care is a core competence. Managed care seems to be working in this population.”
MA came along at the right time for CMS’s push to value-based care.
“I would suggest on the providers’ side, embracing Medicare Advantage is an opportunity to get off the fee-for-service mill,” said Jeff Carroll, senior vice president of Health Plans for Lumeris, which recently paired with Stanford Health Care on the Medicare Advantage plan, Stanford Health Care Advantage.
“Provider-sponsored Medicare Advantage plans are a way to put teeth into an accountable care organization,” Keckley added. “Medicare Advantage success is a silver tsunami among major tsunamis. Obviously it’s a profitable plan for seniors and profitable for underwriters. The winners in the process will get this to scale.”
MA is an innovative model that is not a government-run system, but a privately-run system essentially funded by the government.
PAYERS IN THE MA GAME
UnitedHealthcare has the largest MA market share of any one insurer. Twenty-five percent of Medicare Advantage enrollees are in a UnitedHealthcare MA plan, followed by 17 percent in Humana, 13 percent in a Blue Cross Blue Shield and 8 percent in Aetna, according to the Kaiser Family Foundation.
Numerous insurers, in fact, have gotten into the MA market, including Clover Health in San Francisco, a five-year-old startup which has Medicare Advantage as its only business.
Clover is a tech-oriented company that boasts machine learning models that can accurately predict and identify members at risk of hospitalization.
Because Clover focuses only on MA, it can do a better job at problem solving the needs of an older population, said Andrew Toy, president and CTO of Clover Health.
“The problems we face in Medicare Advantage are very different from a younger generation,” Toy said.
Forty percent of the older population is diabetic. Most seniors will be dealing with a chronic disease as they get older.
In other insurance, whether its individual or commercial, the lower cost of the healthier population offsets the cost of the sicker population. MA has no way to offset these costs. Plans can’t cherry-pick consumers or raise premiums for a percentage of the population.
What MA plans can do is design plans that fit the varying needs of the population. A plan can be designed for diabetics. For younger seniors or those not dealing with a chronic disease, a plan can be designed that includes a gym membership.
“All these plans are regulated,” Toy said. “We have the flexibility to move dollars around. We can offer a higher deductible plan, or a nutrition plan. The incentives for us in Medicare Advantage are different than the incentives in Medicare. CMS has explored giving us more leeway for benefits. Consumers have a choice while still having the guarantees of Medicare.”
Toy believes regular Medicare is more expensive because MA offers a more affordable plan based on what an individual needs.
“When you need it, we get more involved in that care,” Toy said, such as “weight control issues for diabetics.”
The drawbacks are narrower networks, though Toy said Clover offers an out-of-network cost sharing that is pretty much in line with being in-network.
UnitedHealthcare’s Medicare Advantage LPPO plans offer out-of-network access to any provider who accepts Medicare, Warner said.
UnitedHealthcare also offers a wide variety of low and even zero-dollar premium Medicare Advantage plans and annual out-of-pocket maximums, Warner said. By contrast, original Medicare generally covers about 80 percent of beneficiaries’ healthcare costs, leaving them to cover the remaining 20 percent out-of-pocket with no annual limit.
“From a consumer value proposition, it makes Medicare Advantage a better deal,” Kim said. “One is Part B, 20 percent of an unknown number. Knowing what the cost will be in a predictable manner is a preferable manner.”
Stanford Health Care launched a Medicare Advantage plan in 2013. Lumeris owned and operated its own plan, Essence Healthcare, for more than eight years. Stanford and Lumeris partnered on Stanford Health Care Advantage in northern California, using Lumeris technology to help manage value-based reimbursementand new approaches to care delivery through artificial intelligence-enabled diagnostic tools and other methods.
“We are not a traditional insurance company,” Kim said. “We’re thinking about benefits from a provider perspective. It’s a different outlook than an insurance company. By definition we’re local.”
MA MARKET STILL HAS ROOM TO GROW
While the Medicare Advantage market is competitive, it is also under-penetrated, Brian Thompson, CEO for UnitedHealthcare Medicare & Retirement, said during a 2018 earnings report.
Currently, about 33 percent of all Medicare beneficiaries are in an MA plan, he added, but UnitedHealth sees a path to over 50 percent market concentration in the next 5-10 years.
It’s a path not so subtly promoted by the Centers for Medicare and Medicaid Services.
As a way to encourage insurers to take risk and get in the market, around 2009, CMS gave MA insurers 114 percent of what it paid for fee-for-service Medicare. The agency began decreasing those payments so that by 2017, traditional Medicare and MA became about even.
MA insurers instead thrive on their ability to tailor benefits toward wellness, coordinate care and contain costs within the confines of capitated payments, the essence of value-based care.
They have received CMS support in recent rate notices that gives them the ability to offer supplemental benefits, such as being able to target care that addresses the social determinants of health. Starting in 2020, telehealth is being added to new flexibility for these plans.
WHAT THE FUTURE MAY HOLD FOR MA
Medicare Advantage plans have expanded and, in so doing, opened innovative new options for plans and their customers alike at the same time that the ranks of people eligible for Medicare continues to swell.
So where is it all going?
Medicare Advantage is changing the way healthcare is paid and delivered to the point that Keckley and Toy agreed the future may not lie in Medicare for All, but in Medicare Advantage for all.
“I think a reasonable place to end, is in some combination where the government is involved in price control, combined with the flexibility of Medicare Advantage,” Toy said. “That’s really powerful.”

A Medicare buy-in is more popular than switching to a single-payer health care system, according to a new poll from Quinnipiac University.
By the numbers: Overall, voters were split on the wisdom of single-payer — 45% said it would be a bad idea, and 43% said it would be a good idea.
Republicans were the difference-makers. They overwhelmingly oppose single-payer (79% against), but a plurality of Republican voters (43%) support a Medicare buy-in.
Between the lines: Although the political battle between these rival plans is playing out primarily as a litmus test in the 2020 Democratic primary, Democrats seem fine with either proposal.
Yes, but: Even a Medicare buy-in limited to people older than 50 — pretty much the smallest option on the table for Democrats — would still provoke a big fight from industry.
 The Trump administration’s new legal argument against the Affordable Care Act is a political risk. It may also be a liability in court. How it works: The legal issue here is “severability” — if the ACA’s individual mandate is unconstitutional, can it be struck down in isolation? Or is it too intertwined with other parts of the law? Flashback: We’ve seen this movie before — in 2012, at the Supreme Court.
The Justice Department has now forced that same all-or-nothing decision into the case now pending before the 5th Circuit Court of Appeals. “There’s no way they were getting Roberts’ vote anyway … but this won’t help,” said Jonathan Adler, a law professor at Case Western Reserve University who helped spearhead a different challenge to the ACA.
It may not get that far. “I think the states ultimately lose,” Adler said. “I think the most likely outcome is they lose in the 5th Circuit. If they don’t lose at the 5th Circuit, they will lose at the Supreme Court.” If that’s what happens, adopting this riskier legal strategy may ultimately be the only thing that saves Republicans from the political nightmare of wiping out 20 million people’s health care coverage with no strategy on how to replace it.
|

The advantages of working in a high trust environment are evident to everyone from the CEO to the shop floor, from suppliers to customers, and even the competition. Building and maintaining trust within any organization pays off with many benefits.
Here are 12 benefits of working in a high trust culture:
1. Problems are easier to solve – because the energy is on the real problem, and people are not afraid to suggest creative solutions.
2. Focus is on the mission – rather than interpersonal protection.
3. Efficient Communication – less need to “spin” information.
4. Less unrest – little need for damage control.
5. Passion for the work – that is obvious to customers.
6. A real environment – no need to play head games.
7. People respect each other – less bickering and wasting time.
8. Fewer distractions – things get done right the first time.
9. Leaders allowed to be human – can make a mistake and not get derailed.
10. Developing people – emphasis on being the best possible.
11. Reinforcement works better – because it is not perceived as manipulative.
12. People enjoy work – the atmosphere is light and sometimes even fun.
With advantages like these, it is not hard to figure out why high trust groups out perform low trust organizations dramatically. There have been many studies that indicate the leverage you get with a high trust group over a low trust one is at least three times. That is why it is common for groups to more than double productivity in less that a year if the leaders know how to build trust.
There are dozens of leadership behaviors that will develop higher trust. An example would be to do what you say (“walk your talk”). I believe the most powerful leadership behavior that will develop higher trust is to create a safe environment. My quote for this phenomenon is “The absence of fear is the incubator of trust.”
Creating a culture of low fear is not rocket science at all. Leaders simply need to make people understand that they will not be put down for sharing their opinions as long as it is done in an appropriate way and time. I call this action “reinforcing candor,” because the person needs to feel welcome to share a contrary view without fear. Leaders who can accomplish this kind of culture will have the advantages listed above.
Work to consistently build, maintain, and repair trust in your organization. I believe the leverage in doing so is the most significant path to greatness in any organization.
 The Justice Department now wants the courts to strike down the entire Affordable Care Act — not just its protections for people with pre-existing conditions. This is a stunning escalation, raising both the real-world and political stakes in a lawsuit where both the real-world and political stakes were already very high. Where it stands: Judge Reed O’Connor ruled in December that the ACA’s individual mandate has become unconstitutional, and that the whole law must fall along with it.
Why it matters: If DOJ ultimately gets its way here, the ripple effects would be cataclysmic. The ACA’s insurance exchanges would go away. So would its Medicaid expansion. Millions would lose their coverage.
Politically, this makes no sense. Chuck Schumer and Nancy Pelosi must be dancing in the streets.
What they’re saying:
|