As the Senate eyes alternative or additional cost-saving provisions to those included in the House-passed reconciliation bill, some Republicans are considering reforms to Medicare. That is a promising development because overhauling Medicare Advantage could lower federal costs in ways that even many Democrats have advocated (although it is certain the overall bill will receive no Democratic support due to myriad other provisions).
Medicare Advantage, or MA, is Medicare’s private insurance option.
Beneficiaries can get their coverage through these plans in lieu of the traditional, government-managed program. Medicare pays MA sponsors a per-person monthly fee, which they use in turn to pay providers for the services their enrollees need. Enrollment in MA surged after Congress amended the payment formula in 2003. According to the 2024 Medicare trustees report, in the last decade alone, MA enrollment increased from 16 million people in 2014, or 30 percent of total enrollment, to 34 million people in 2024, or one out of every two program beneficiaries.
MA is growing because the plans usually offer more generous coverage than the traditional program without charging substantially higher premiums. In fact, many MA enrollees get free prescription drug coverage and much lower cost-sharing for hospital and physician services. They also sometimes get limited dental and vision care protection. MA enrollees usually do not pay for Medigap insurance, which can be expensive.
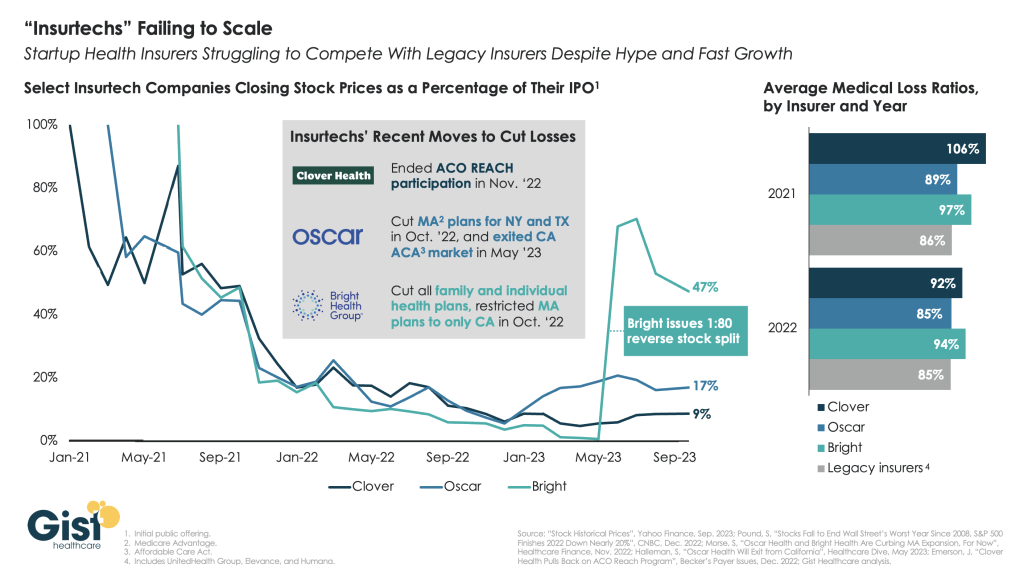
Critics argue MA plans can offer added benefits only because they are overpaid – a contention credible research confirms, including as conducted by the Medicare Payment Advisory Commission (MedPAC). At the same time, other data shows MA plans are often more efficient at delivering services than the traditional program because the plans scrutinize claims more carefully. High MA enrollment is also associated with positive spillover effects in the traditional program.
MA reforms should incentivize efficiency and high-quality care without needlessly overpaying the plans. The Senate should pull together a reform plan that gradually restructures the MA market so that it operates more efficiently and with lower costs for taxpayers. The following general principles should guide what is developed.
- Competitive Bidding.
- MA plans submit bids under the current formula, but Medicare’s payment is a combination of those bids and benchmarks that are set administratively. The Senate should amend the formula to rely strictly on bidding, with a transition to prevent abrupt changes in what is offered to enrollees. The payment could be based on the average bid weighted by enrollment. The new system could be phased in over five years by gradually increasing its influence on the formula (20 percent in year one, going up to 100 percent in year five, for instance).
- Standardized Benefits.
- Competitive bidding should be combined with standardization of the coverage MA plans are offering. Without such rules, it is difficult for individual beneficiaries to compare their options on an apples-to-apples basis. The Senate should require CMS to develop a standard MA offering that is comparable in value to the traditional benefit (it may be necessary to add catastrophic protection to the traditional program to ensure the competition is fair). MA plans would then submit their bids based on this standardized offering, and all Medicare beneficiaries would have the option of opting for such coverage. Further, the Senate should direct CMS to develop a small number of standardized supplemental benefits that could be purchased by beneficiaries with additional premium payments. These offerings could focus on the most popular add-ons in the MA market.
- Risk Adjustment.
- There are many criticisms of the current system of providing payment adjustments to MA plans based on the varied health risks of their enrollees. The current system has several flaws that might be addressed, but the basic problem is too much reliance on the data submitted by the plans which can lead directly to higher revenue. That design of course invites abuse. The Senate should put into law a requirement that CMA is to determine a final annual risk score for the plans based on submitted information, and any needed refinements by the government to ensure the fairest possible comparisons across plans.
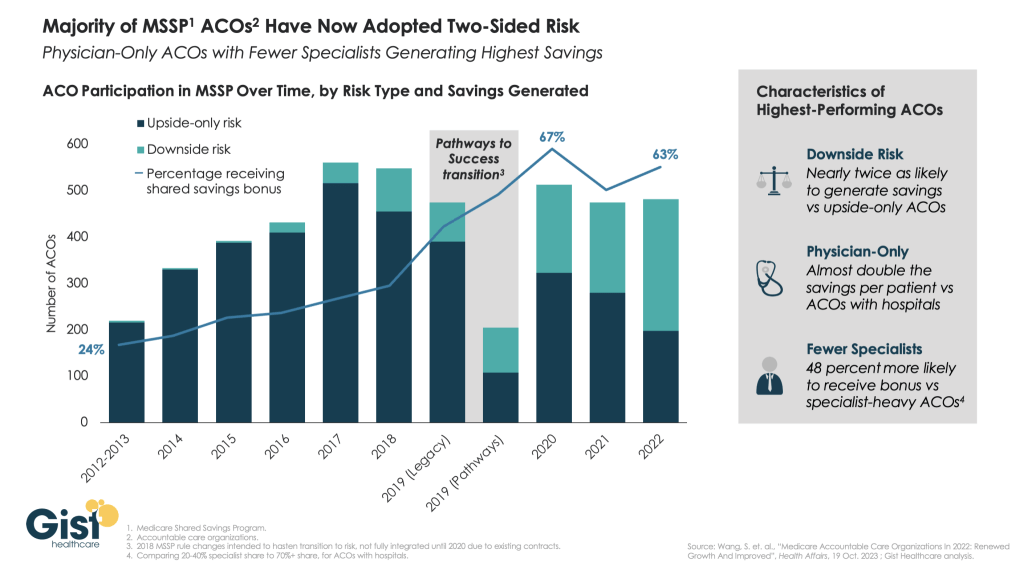
- ACOs as MA Plans.
- The Medicare program would benefit from robust provider-driven MA plans that can effectively compete with the insurer-led MA offerings now dominating the market. CMS should work with interested Accountable Care Organizations (ACOs) on building out functions they would need to become viable alternatives in the MA insurance market.
The Congressional Budget Office (CBO) estimates the House bill will increase deficits by $3.0 trillion over ten years when net interest is in the calculation. Medicare reforms could help the Senate produce a more fiscally responsible bill. If an MA bidding system led to a reduction in payments comparable to a 10 percent cut (which is realistic based on MedPAC’s research), the savings over a decade would be close to $500 billion.