https://www.healthleadersmedia.com/strategy/northwell-ceo-urging-healthcare-providers-mobilize-gun-control
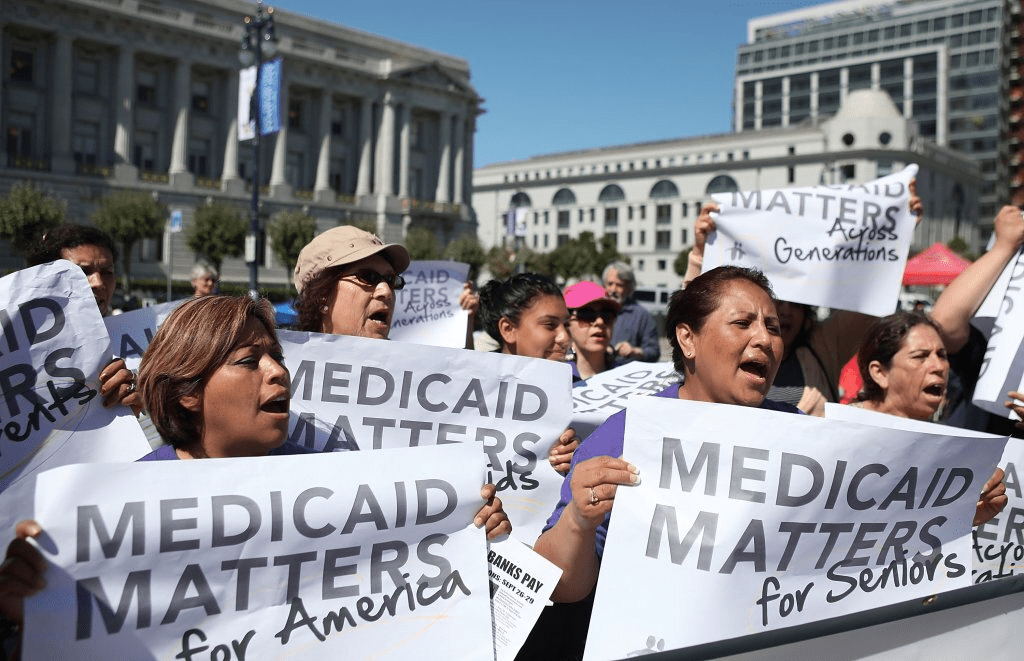
The prominent executive is pushing beyond a letter he released last week and is now seeking to rally his peers around solving what he sees as a public health crisis.
KEY TAKEAWAYS
‘All of us have allowed this crisis to grow,’ he wrote in a letter published Thursday in The New York Times.
Healthcare CEOs should put pressure on politicians without resorting to ‘blatant partisanship,’ he said.
Northwell Health President and CEO Michael J. Dowling isn’t done pushing fellow leaders of healthcare provider organizations to take political action in the aftermath of deadly mass shootings.
Dowling addressed healthcare CEOs in a “call to action“ published online last week by the Great Neck, New York–based nonprofit health system. Now he’s published a full-page print version of that letter in Thursday’s national edition of The New York Times, while reaching out directly to peers who could join him in a to-be-determined collective action plan to curb gun violence.
“To me, it’s an obligation of people who are in leadership positions to take some action, speak out, and prepare their organizations to address this as a public health issue,” Dowling tells HealthLeaders.
Wading into such a politically charged topic is sure to give some healthcare CEOs pause. Even if they keep their advocacy within all legal and ethical bounds, they could face rising distrust from community members who oppose further restrictions on firearms. But leaders have a responsibility to thread that needle for the sake of community health, Dowling says.
“I do anticipate that there’ll be criticism about this, but then again, if you’re in a leadership role, criticism is what you’ve got to deal with,” he says.
Dowling argues that healthcare leaders have successfully spoken out about other public health crises, such as smoking and drug use. But they have largely failed to respond adequately as gun violence inflicts considerable harm—both physical and emotional—on the communities they serve, he says.
“It is easy to point fingers at members of Congress for their inaction, the vile rhetoric of some politicians who stoke the flames of hatred, the lax laws that provide far-too-easy access to firearms, or the NRA’s intractable opposition to common sense legislation,” Dowling wrote in the print version of his letter. “It is far more difficult to look in the mirror and see what we have or haven’t done. All of us have allowed this crisis to grow. Sadly, as a nation, we have become numb to the bloodshed.”
His letter proposes a four-part agenda for healthcare leaders to tackle together:
- Put pressure on elected officials who “fail to support sensible gun legislation.” He urged healthcare CEOs to increase their political activity but avoid “blatant partisanship.” The online version of his letter links to OpenSecrets.org‘s repository of information on campaign contributions from gun rights interest groups to politicians.
- Invest in mental health without stigmatizing. Most mass murderers aren’t “psychotic or delusional,” Dowling wrote. Rather, they’re usually just disgruntled people who let their anger erupt into violence, which is why firearms sales to people at risk of harming themselves or others should be prohibited, he wrote.
- Increase awareness and training. Individuals shouldn’t be allowed to buy or access certain types of firearms “that serve no other purpose than to inflict mass casualties,” he wrote. Healthcare leaders should support efforts to spot risk factors and better understand so-called “red flag” laws that empower officials to take guns away from people deemed to be a potential threat to themselves or others, he wrote.
- Support universal background checks. In the same way that doctors shouldn’t write prescriptions without knowing a patient’s medical history to ensure the drug will do no harm, gun sellers shouldn’t be allowed to complete a transaction without having a background check conducted on the buyer, Dowling wrote, adding that a majority of Americans support this idea.
The letter notes that the U.S. has nearly 40,000 firearms-related deaths each year and that several dozen people have died in mass shootings thus far in 2019, including 31 earlier this month in separate shootings in El Paso, Texas, and Dayton, Ohio.
Corporate Responsibility
The way for-profit companies think about their relationship with the communities in which they operate has been shifting for some time. The most recent evidence of that shift came earlier this week, when the influential Business Roundtable released a revised statement on the principles of corporate governance, responding to criticism over the so-called “primacy of shareholders.”
The 181 CEOs who signed onto the new statement said they would run their business not just for the good of their shareholders but also for the good of customers, employees, suppliers, and communities. There’s some similarity between that updated notion of corporate responsibility and the sort of advocacy work Dowling wants to see from his for-profit and nonprofit peers alike.
Every single organization has a social mission, and large organizations that have sway in a local community have a responsibility to the community’s health, Dowling says.
“A healthy community helps and creates a healthy organization,” he says.
One major factor that may be pushing more CEOs to take a public stance on politically sensitive issues—or at least giving them the cover to do so confidently—is the generational shift in the U.S. workforce. Although most Americans overall say CEOs shouldn’t speak out, younger workers overwhelmingly support such action, as Fortune‘s Alan Murray reported, citing the magazine’s own polling.
Dowling says he has received hundreds of letters, emails, and phone calls from members of Northwell Health’s 70,000-person workforce expressing support in light of his original letter published online last week.
“The feedback has been absolutely universal in support,” he says.
But Which Policies?
Even among healthcare professionals who agree it’s appropriate to speak out on politically charged topics, there’s sharp disagreement over which policies lawmakers should enact and whether those policies would infringe on the public’s Second Amendment rights.
The group Doctors for Responsible Gun Ownership (DRGO) rejects the premise of Dowling’s argument: “Firearms are not a public health issue,” the DRGO website states, arguing that responsible gun ownership has been shown to benefit the public health by preventing violent crime.
Dennis Petrocelli, MD, a psychiatrist in Virginia, wrote a DRGO article that called Virginia’s proposed red flag law “misguided” and perhaps “the single greatest threat to our constitutional freedoms ever introduced in the Commonwealth of Virginia.” His concern is that the government might be able to take guns away without any real evidence of a threat.
While gun rights advocates may see Dowling as merely their latest political foe, Dowling contends that he’s pushing for a cause that can peaceably coexist with the constitutional right to bear arms.
“You can have effective, reasonable legislative action around guns that still protects the essence of what many people believe to be the core of the Second Amendment,” Dowling says. “It’s not an either/or situation.”
Others Speaking Out
Dowling isn’t, of course, the only healthcare leader speaking out about gun violence.
On the same day last week that Northwell Health published Dowling’s online call to action, Ascension published a similar letter from President and CEO Joseph R. Impicciche, JD, MHA, who referred to gun violence in American society as a “burgeoning public health crisis.”
“Silence in the face of such tragedy and wrongdoing falls short of our mission to advocate for a compassionate and just society,” Impicciche wrote, citing the health system’s Catholic commitment to defend human dignity.
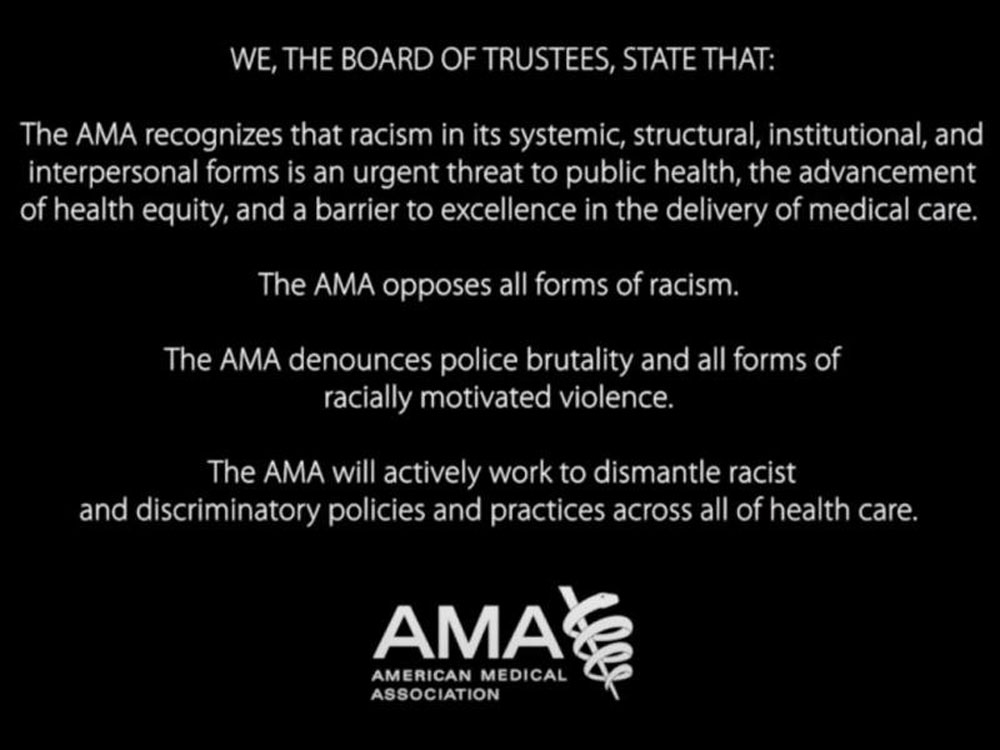
The American Medical Association (AMA) and American College of Emergency Physicians (ACEP) each issued statements this month calling for public policy changes in response to these recent shootings, continuing their long-running advocacy work on the topic.
American Hospital Association 2019 Chairman Brian Gragnolati, who is president and CEO of Atlantic Health System in Morristown, New Jersey, said in a statement this month that hospitals and health systems “play a role in the larger conversation and are determined to use our collective voice to prevent more senseless tragedies.”