
Cartoon – The Kid’s Point of View


https://mailchi.mp/13ef4dd36d77/the-weekly-gist-august-27-2021?e=d1e747d2d8

Droplets, fomites, aerosols…these terms describing the kinds of particles which can spread virus particles rose to the top of our lexicon last year. Initially we focused on fomites, infectious particles deposited on surfaces, and worried that touching our groceries and mail could spread the coronavirus.
Scientists were convinced that most COVID transmission occurred via droplets, large respiratory particles exhaled in a cough or a sneeze that traveled only a short distance from an infected person, which led to the guidance that staying six feet apart would keep us safe. But worrisome case reports of a single individual passing the virus to a roomful of people, and the mitigating effects of ventilation, began to hint at aerosol transmission, a much more insidious type of spread in which the virus is transmitted through much smaller particles, which travel longer distances and can linger in the air for hours.
Aerosol spread is not only worrisome because it makes a pathogen more contagious, but smaller aerosol particles can be inhaled more deeply into the lungs, potentially causing more severe illness. A new review in Science evaluates the current data on COVID transmission and the advances made over the past year in understanding airflow and aerosol spread, making the bold statement that aerosol transmission is not only the main mechanism for COVID-19 spread, but is likely the primary mode of transmission for the vast majority of respiratory diseases.
Today, our lack of attention to ventilation, air purification and other means to reduce aerosol spread means that we are woefully unprepared for children to return to school—and underscores the need for extensive masking to mitigate transmission. But in the long run, better understanding the mechanisms for preventing airborne transmission could allow us to reduce susceptibility to a host of respiratory diseases. Take complications from asthma, which dropped dramatically during the pandemic—leading researchers to posit that viral infections, rather than environmental triggers, could be the more common cause behind exacerbations.
Harnessing this new knowledge will require further research to quantify the effects of spread and mitigation—and the willingness to invest in preventive measures in schools and other public spaces, yet another domain in which bolstering public health could have a meaningful long-term impact on our lives.
https://mailchi.mp/13ef4dd36d77/the-weekly-gist-august-27-2021?e=d1e747d2d8
When COVID volumes waned in the spring and early summer, most health systems “de-escalated” dedicated COVID testing and triage facilities. But with the Delta variant surging across the country, consumers are now once again looking for services like drive-through testing, which is perceived as more convenient and safer.
One physician leader told us patients in the ED are asking why the hospital got rid of the “COVID tent”, which provided a separate pathway for patients with respiratory and other COVID symptoms—and a highly visible signal that the rest of the department was as COVID-free as possible.
Another system is now fielding questions from the media about whether they’ll bring back their dedicated COVID hospital: “We spent a lot of time last year convincing the community that the dedicated hospital was key to safely managing care during the pandemic. Now we’ve got almost as many COVID admissions spread across our hospitals.”
Over the past year, providers have learned how to safely manage COVID care and prevent spread in healthcare settings—but consumers may perceive the lack of dedicated facilities as a decline in safety.
Unlike last year, hospitals are full of non-COVID patients, as those who delayed care reemerge. And with the current surge likely to continue into flu season, emergency rooms will only get more crowded, necessitating a new round of communication describing how hospitals are keeping patients safe, and reassuring patients that healthcare settings remain one of the safest places to visit in the community.
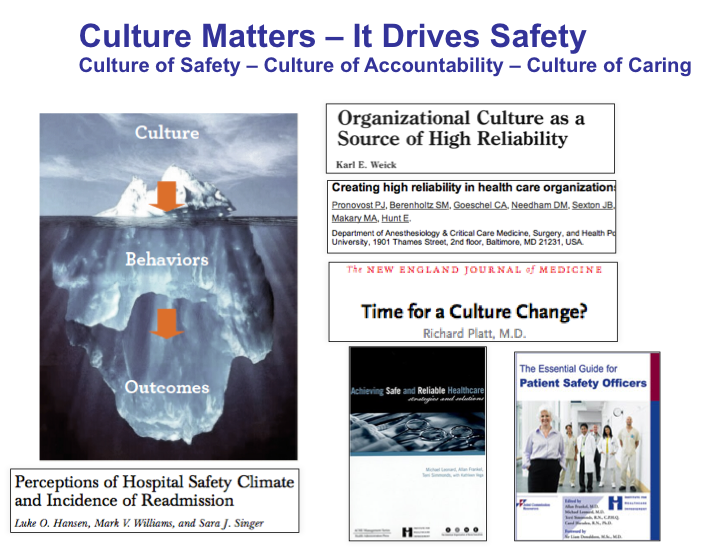
As billions of people gear up for widespread vaccination against COVID-19, another issue has reared its head. Three major COVID-19 variants have emerged across the globe—and preliminary research suggests these variants may be cause for concern.
But what makes them different from the original strain?
The following visualizations answer some key questions, including when these variants were first discovered, how far they’ve spread worldwide, and most importantly, their potential impact on the population.
Before diving in, it’s important to understand why viruses mutate in the first place.
To infect someone, a virus takes over a host cell and uses it to replicate itself. But nature isn’t perfect, and sometimes, mistakes are made during the replication process—those mistakes are called mutations.
A virus with one or more mutations is referred to as a variant. Most of the time, variants do not affect a virus’s physical structure, and in those instances, they eventually disappear. However, there are certain cases when a mutation impacts part of a virus’s genetic makeup that does change its behavior.
According to the U.S. Centers for Disease Control (CDC) a change in behavior can alter:
Preliminary research has detected some of these changes in the three major COVID-19 variants—B.1.1.7, B.1.351, and P.1.
The three major variants emerged at different times, and in different parts of the world. Here’s an overview of each variant, when they were discovered, and how far they’ve spread so far.
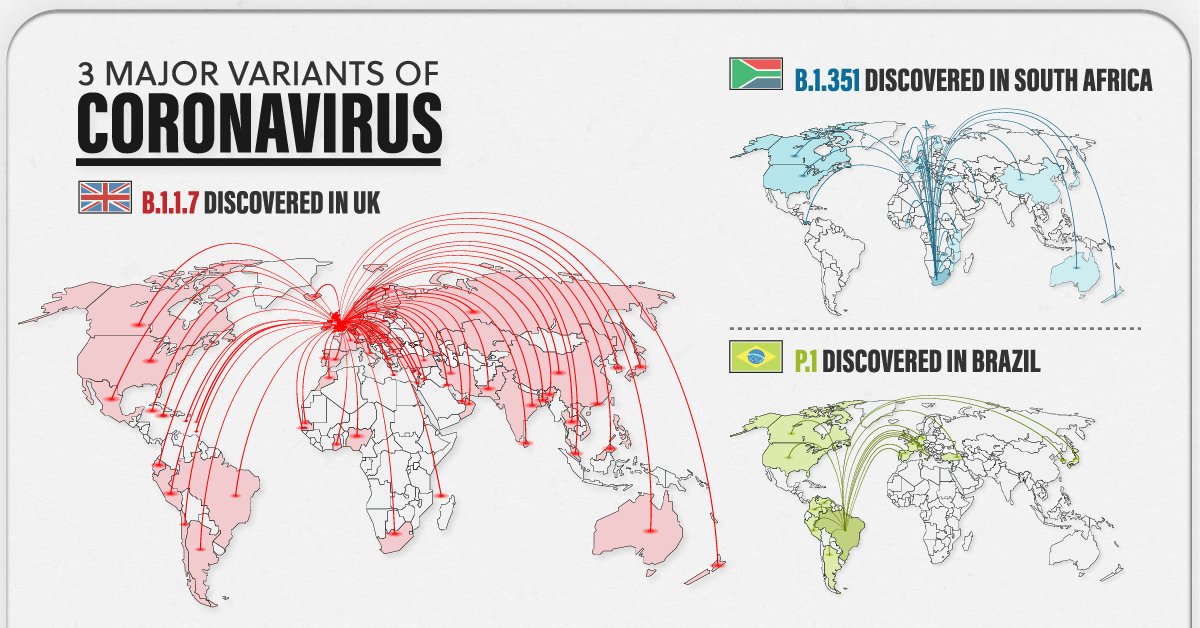
The B.1.1.7 variant was detected in the UK in the fall of 2020. By December 2020, it had spread across the globe, with cases emerging across Europe, North America, and Asia.
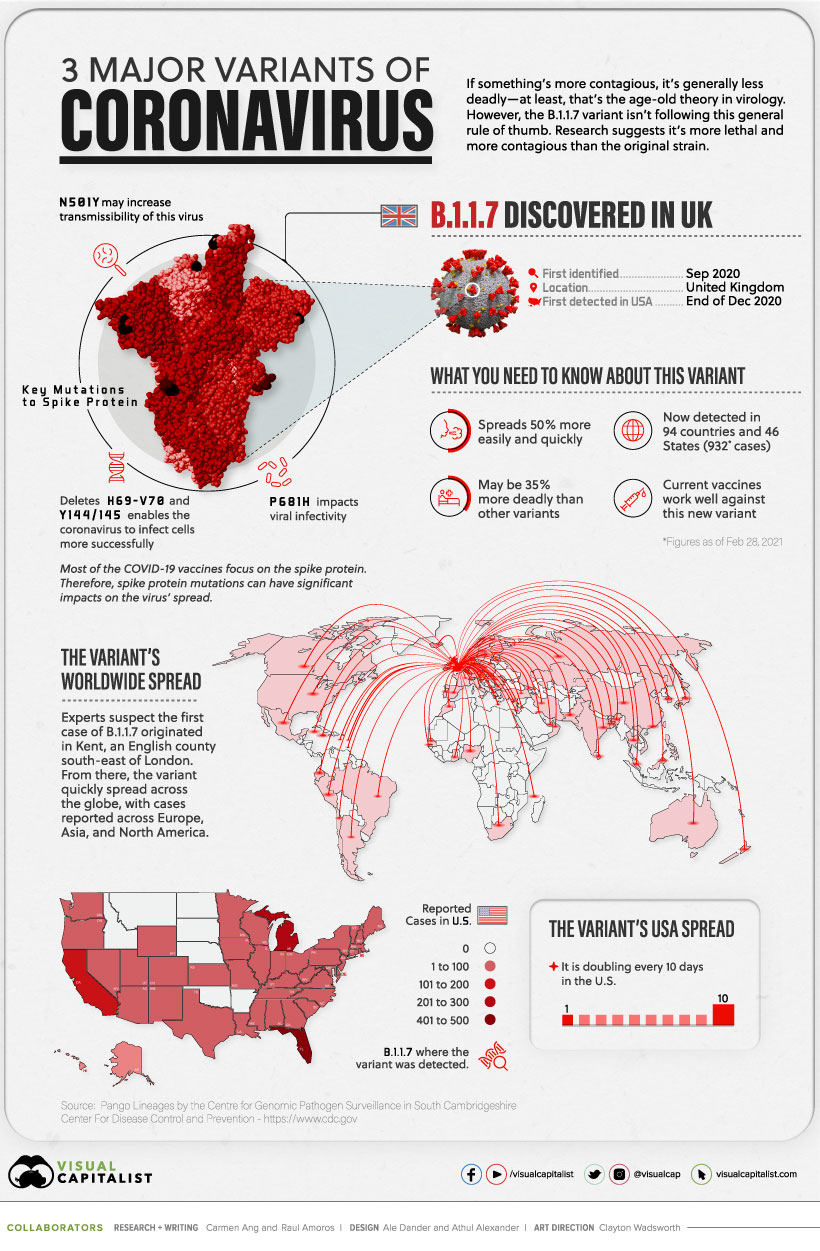
Currently, the variant has been reported in roughly 94 countries.
Early research suggests it’s 50% more transmissible than other variants, and potentially 35% more deadly than the standard virus. Luckily, studies suggest that some of the existing vaccines work well against it.
In October 2020, the second major variant was discovered—B.1.351. It was first identified in South Africa, but by end of the year, it had spread to the UK, Switzerland, Australia, and Japan.
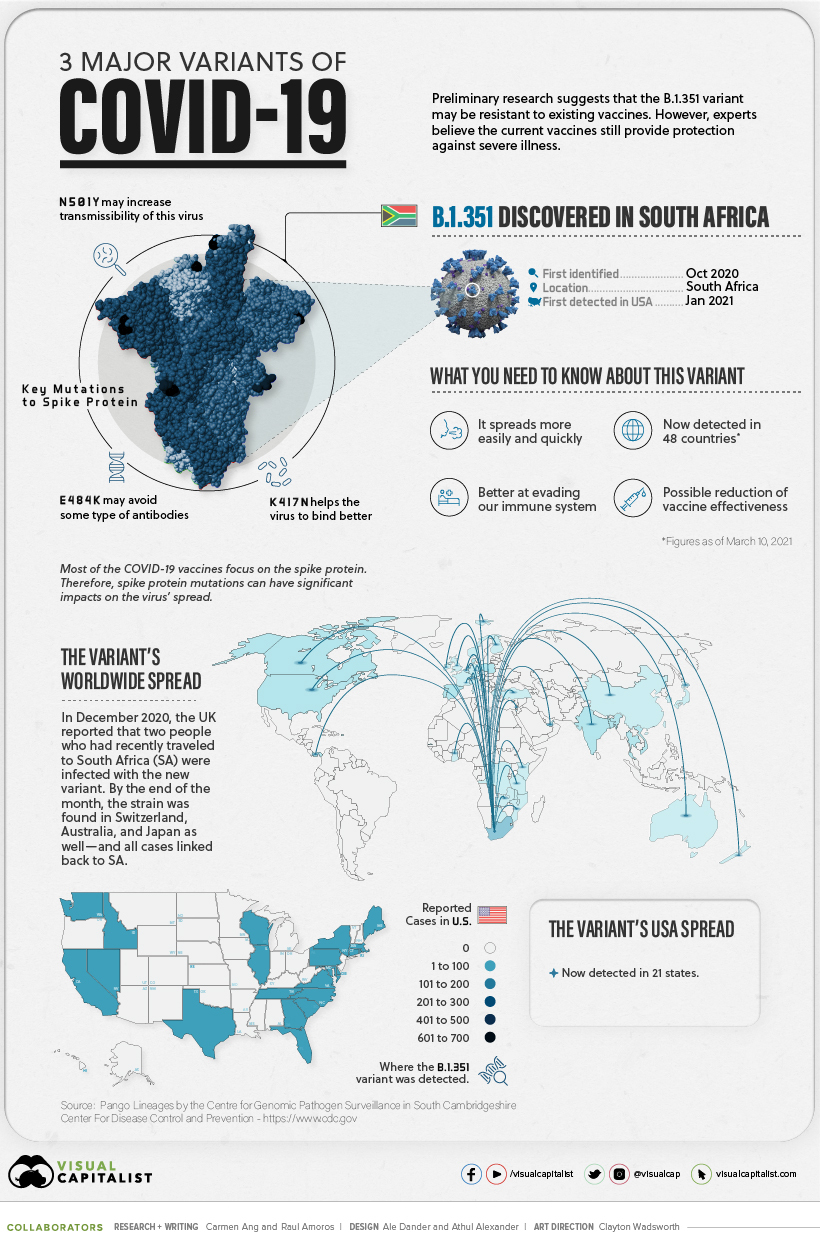
There are approximately 48 countries with reported cases, and research suggests several of the existing COVID-19 vaccines may not be as effective against this variant.
The P.1 variant was the last to arrive on the scene.
It was first discovered in January 2021, when Japan reported four cases of the variant, which was found in travelers who had arrived from Brazil.
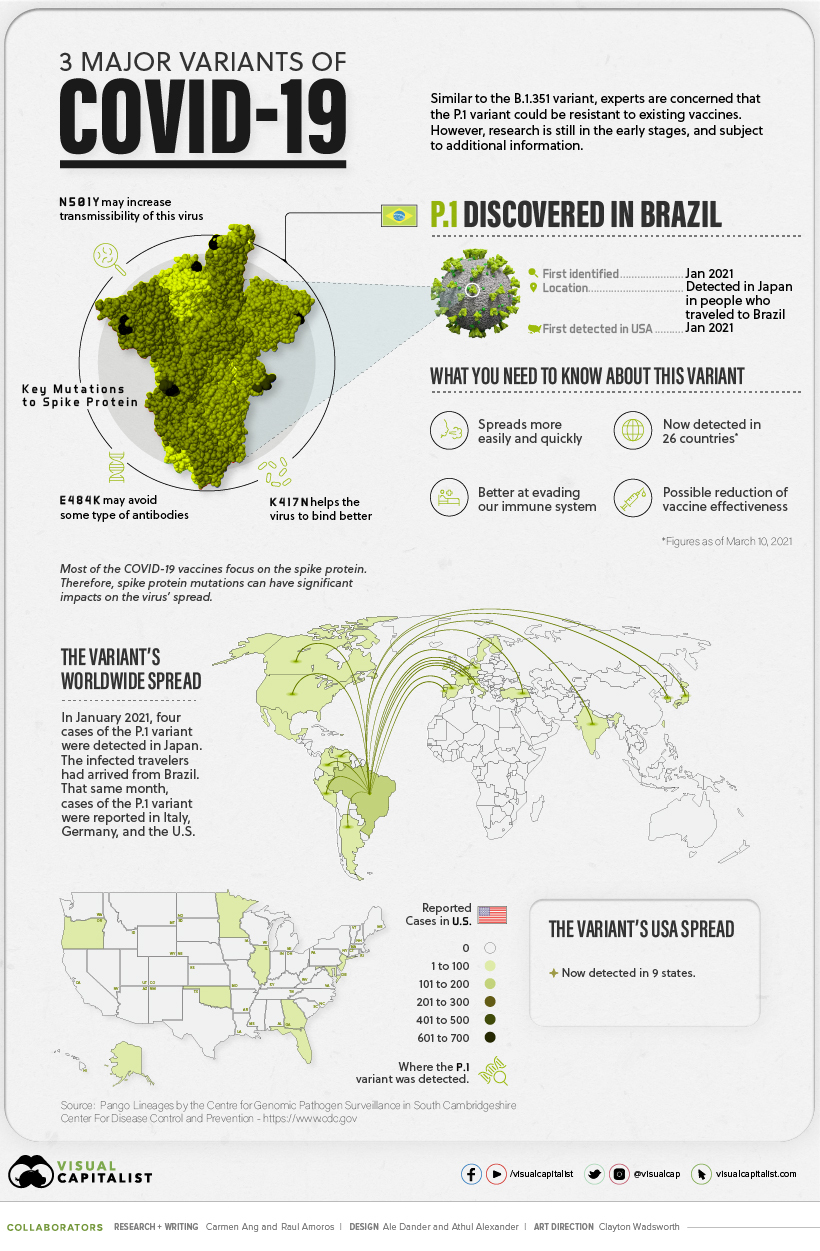
Approximately 25 countries have reported cases of the P.1 variant, and early research suggests this variant is not only more contagious, but could also have the ability to infect people with natural immunity who had already recovered from the original strain.
While there have been preliminary studies showing a dip in vaccine effectiveness, some experts emphasize that it’s too early to tell for certain. More data is needed to gain a deeper and more accurate understanding.
In the meantime, experts are emphasizing the importance of following our current public health strategies, which include physical distancing, vaccination, washing your hands, and using masks.


Oh, how the tide has turned. Three months ago, COVID was ravaging my homeland, India. The Delta variant was burning through the country like an uncontrolled wildfire. People carted dying relatives town to town, desperately seeking hospital beds or a whiff of oxygen. A cousin in India said, “COVID is not taking lives, just the beds. Lack of oxygen is taking lives.”
I watched India’s suffering unfold and felt guilty for living in one of the world’s most resourceful and scientifically advanced countries. My homeland was floundering, but at least my other homeland — the U.S. — was finally on track.
104 million Americans had been vaccinated. The Pfizer vaccine alleviated the worst outcomes of the B.1.1.7 and B.1351 variants. Adolescents aged 12-15 were gearing up for vaccine eligibility within days, and the CDC was reporting the U.S. could see a sharp decline in COVID cases by July if nationwide vaccinations continued. Health care workers had proper PPE, millions of people were getting vaccinated each week, and infection rates were declining steadily. We could finally see Spring’s light at the end of the year’s tortuous dark tunnel. Our country was in the home stretch.
Now the Delta variant is here and I have to wonder, Who were we kidding? We don’t live in a world where vertical borders prevent airborne particles from crossing time zones. Planes and boats carry viruses from one country to the next like microscopic stowaways. The virus doesn’t abandon ship. It mutates, and adapts, and colonizes.
We had a real chance to strangle this monster, to show the rest of the world how it was done, to help them all in the process. We let that chance slip away. Not everyone and not everywhere, but enough people got complacent. Some waited for herd immunity to carry the load—a number that crept from 60 to 70 to 85 percent, depending on what you read and when you read it—and others just figured it would pass. Now the Delta variant, the same one that tore through India and Great Britain, has twisted out of our flimsy grip and is roaring with laughter.
How did this happen?
Misinformation. Political discord. Vaccine hesitancy. The bottom line is our vaccination rate faltered. The CDC reported that on August 1, 2021, approximately 400,000 Americans received their first COVID dose. While that seems high, it’s less than a quarter of the peak in mid-April. We haven’t maxed out eligible people (only 58.1 percent of eligible people were fully vaccinated as of a week ago). We’re maxing out the number of people who know COVID’s real repercussions are far worse than the vaccine’s feared ones.
The U.S now has the third-highest rate of vaccine skepticism among 15 of the world’s largest economies. Our vaccine surplus is so large the FDA extended Johnson & Johnson’s vaccine expiration dates to avoid throwing out perfectly good doses. Less than a week ago, President Biden announced the U.S. has donated and shipped more than 110 million doses to 60 countries. While I applaud the humanitarian effort, I question the fate of those doses if the 41.9 percent unvaccinated eligible people in our country had wanted them.
It makes me wonder: Why does science take a backseat to unsubstantiated pseudoscientific claims?
Spreaders of vaccine disinformation fill their social media accounts with statements questioning COVID’s existence and purporting unproven treatments (never mind the fact that we wouldn’t need treatments if COVID didn’t exist) with little to no peer-reviewed scientific research to support their anti-vaccine claims. According to Imran Ahmed, CEO of the Center for Countering Digital Hate, twelve people — the “disinformation dozen” — produce 65 percent of the shares of anti-vaccine misinformation on social media platforms.”
Is it easier for some to believe that a science-backed treatment is inherently more dangerous than an unknown herb plucked from a field? Perhaps. But what do they say to the approximately 216 kids hospitalized daily in the U.S. over the past week, particularly in areas where vaccine coverage is low? Bad luck? You weren’t strong enough? What would have made them stronger?
Yes, there are measures underway to increase vaccinations—full FDA approval, social media crackdowns on misinformation, and government, company, military, and college mandates. But let’s be honest, many Americans are fighting these measures, as they will fight future mandates, and the next vaccine.
Only two things can change how non-vaxxers perceive COVID vaccines: education and trust. We need to sincerely hear their reasons, and then gently clarify misinformation—vaccines don’t introduce disease into our bodies. They stimulate our immune systems to obtain immunity without getting the disease. Vaccines don’t alter our DNA. Their safety has been tested. Medicines have potential side effects, but illnesses have definite ones. COVID kills indiscriminately; vaccines don’t.
Trust is harder. How can we help people trust these vaccines? I suppose on a deeper level, it’s more about trusting the people that make the vaccines. Big pharma, for-profit companies—sure, they are the money makers. But behind the scenes, the vaccines are created by men and women who’ve accepted the charge to make this world—not just individuals—safer and healthier. They’ve spent years studying, researching, and testing potential vaccines with dedication and patience, including the mRNA technology in COVID vaccines. Just because the COVID vaccine’s rollout was fast-tracked to combat the pandemic doesn’t mean the scientists cut corners in designing and testing it.
Unfortunately, we don’t have the luxury of slowly educating and gradually building trust. COVID is terrorizing our planet now. The world is shaking its heads at the U.S., wondering what happened. We were supposed to be the leader. This morning, an aunt in a small town in India sent me a WhatsApp message: “I have taken the vaccine … the positivity rate has gone down … I am worried for America … how r u?” I don’t know. America, how are we? It’s not too late to destroy this monster, but if the unvaccinated remain unmoved, it will be soon.