/cdn.vox-cdn.com/uploads/chorus_asset/file/18046968/web_1863137.jpg)
Cartoon – Chances of Bipartisan Health Reform
/cdn.vox-cdn.com/uploads/chorus_asset/file/18046968/web_1863137.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/18046968/web_1863137.jpg)

https://apnews.com/article/us-news-nutrition-coronavirus-pandemic-d1e17ef502ab92bd41216c90ac60ba5f

When COVID-19 first swarmed the United States, one health insurer called some customers with a question: Do you have enough to eat?
Oscar Health wanted to know if people had adequate food for the next couple weeks and how they planned to stay stocked up while hunkering down at home.
“We’ve seen time and again, the lack of good and nutritional food causes members to get readmitted” to hospitals, Oscar executive Ananth Lalithakumar said.
Food has become a bigger focus for health insurers as they look to expand their coverage beyond just the care that happens in a doctor’s office. More plans are paying for temporary meal deliveries and some are teaching people how to cook and eat healthier foods.
Benefits experts say insurers and policymakers are growing used to treating food as a form of medicine that can help patients reduce blood sugar or blood pressure levels and stay out of expensive hospitals.
“People are finally getting comfortable with the idea that everybody saves money when you prevent certain things from happening or somebody’s condition from worsening,” said Andrew Shea, a senior vice president with the online insurance broker eHealth.
This push is still relatively small and happening mostly with government-funded programs like Medicaid or Medicare Advantage, the privately run versions of the government’s health program for people who are 65 or older or have disabilities. But some employers that offer coverage to their workers also are growing interested.
Medicaid programs in several states are testing or developing food coverage. Next year, Medicare will start testing meal program vouchers for patients with malnutrition as part of a broader look at improving care and reducing costs.
Nearly 7 million people were enrolled last year in a Medicare Advantage plan that offered some sort of meal benefit, according to research from the consulting firm Avalere Health. That’s more than double the total from 2018.
Insurers commonly cover temporary meal deliveries so patients have something to eat when they return from the hospital. And for several years now, many also have paid for meals tailored to patients with conditions such as diabetes.
But now insurers and other bill payers are taking a more nuanced approach. This comes as the coronavirus pandemic sends millions of Americans to seek help from food banks or neighborhood food pantries.
Oscar Health, for instance, found that nearly 3 out of 10 of its Medicare Advantage customers had food supply problems at the start of the pandemic, so it arranged temporary grocery deliveries from a local store at no cost to the recipient.
The Medicare Advantage specialist Humana started giving some customers with low incomes debit cards with either a $25 or $50 on them to help buy healthy food. The insurer also is testing meal deliveries in the second half of the month.
That’s when money from government food programs can run low. Research shows that diabetes patients wind up making more emergency room visits then, said Humana executive Dr. Andrew Renda.
“It may be because they’re still taking their medications but they don’t have enough food. And so their blood sugar goes crazy and then they end up in the hospital,” he said.
The Blue Cross-Blue Shield insurer Anthem connected Medicare Advantage customer Kim Bischoff with a nutritionist after she asked for help losing weight.
The 43-year-old Napoleon, Ohio, resident had lost more than 100 pounds about 11 years ago, but she was gaining weight again and growing frustrated.
The nutritionist helped wean Bischoff from a so-called keto diet largely centered on meats and cheeses. The insurer also arranged for temporary food deliveries from a nearby Kroger so she could try healthy foods like rice noodles, almonds and dried fruits.
Bischoff said she only lost a few pounds. But she was able to stop taking blood pressure and thyroid medications because her health improved after she balanced her diet.
“I learned that a little bit of weight gain isn’t a huge deal, but the quality of my health is,” she said.
David Berwick of Somerville, Massachusetts, credits a meal delivery program with improving his blood sugar, and he wishes he could stay on it. The 64-year-old has diabetes and started the program last year at the suggestion of his doctor. The Medicaid program MassHealth covered it.
Berwick said the nonprofit Community Servings gave him weekly deliveries of dry cereal and premade meals for him to reheat. Those included soups and turkey meatloaf Berwick described as “absolutely delicious.”
“They’re not things I would make on my own for sure,” he said. “It was a gift, it was a real privilege.”
These programs typically last a few weeks or months and often focus on customers with a medical condition or low incomes who have a hard time getting nutritious food. But they aren’t limited to those groups.
Indianapolis-based Preventia Group is starting food deliveries for some employers that want to improve the eating habits of people covered under their health plans. People who sign up start working with a health coach to learn about nutrition.
Then they can either begin short-term deliveries of meals or bulk boxes of food and recipes to try. The employer picks up the cost.
It’s not just about hunger or a lack of good food, said Chief Operating Officer Susan Rider. They’re also educating people about what healthy, nutritious food is and how to prepare it.
Researchers expect coverage of food as a form of medicine to grow as insurers and employers learn more about which programs work best. Patients with low incomes may need help first with getting access to nutritional food. People with employer-sponsored coverage might need to focus more on how to use their diet to manage diabetes or improve their overall health.
A 2019 study of Massachusetts residents with similar medical conditions found that those who received meals tailored to their condition had fewer hospital admissions and generated less health care spending than those who did not.
Study author Dr. Seth Berkowitz of the University of North Carolina noted that those meals are only one method for addressing food or nutrition problems. He said a lot more can be learned “about what interventions work, in what situations and for whom.”
A lack of healthy food “is very clearly associated with poor health, so we know we need to do something about it,” Berkowitz said.
https://mailchi.mp/128c649c0cb4/the-weekly-gist-january-22-2021?e=d1e747d2d8

As one of his first official actions upon taking office Wednesday, President Biden signed an executive order implementing a federal mask mandate, requiring masks to be worn by all federal employees and on all federal properties, as well as on all forms of interstate transportation. Yesterday Biden followed that action by officially naming his COVID response team, and issuing a detailed national plan for dealing with the pandemic. Describing the plan as a “full-scale wartime effort”, Biden highlighted the key components of the plan in an appearance with Dr. Anthony Fauci and COVID response coordinator Jeffrey Zients.
The plan instructs federal agencies to invoke the Defense Production Act to ensure adequate supplies of critical equipment, including masks, testing equipment, and vaccine-related supplies; calls for new national guidelines to help employers make workplaces safe for workers to return to their jobs, and to make schools safe for students to return; and promises to fully fund the states’ mobilization of the National Guard to assist in the vaccine rollout.
Also included in the plan is a new Pandemic Testing Board, charged with ramping up multiple forms of COVID testing; more investment in data gathering and reporting on the impact of the pandemic; and the establishment of a health equity task force, to ensure that vulnerable populations are an area of priority in pandemic response.
But Biden can only do so much by executive order. Funding for much of his ambitious COVID plan will require quick legislative action by Congress, meaning that the administration will either need to garner bipartisan support for its proposed “American Rescue Plan” legislation, or use the Senate’s budget reconciliation process to pass the bill with a simple majority (with Vice President Harris casting the tie-breaking vote). Even that may prove challenging, given skepticism among Republican (and some moderate Democratic) senators about the $1.9T price tag for the legislation.
We’d anticipate intense bargaining over the relief package—with broad agreement over the approximately $415B in spending on direct COVID response, but more haggling over the size of the economic stimulus component, including the promised $1,400 per person in direct financial assistance, expanded unemployment insurance, and raising the federal minimum wage to $15 per hour.
Some of the broader economic measures, along with the rest of Biden’s healthcare agenda and his larger proposals to invest in rebuilding critical infrastructure, may have to wait for future legislation, as the administration prioritizes COVID relief as its first—and most important—order of business.

On January 14, 2021, Planned Parenthood Southeast and the Feminist Women’s Health Center filed a lawsuit challenging the Trump administration’s approval of Georgia’s waiver under Section 1332 of the Affordable Care Act (ACA). The lawsuit was filed in federal district court in DC. This post summarizes that legal challenge as well as parts of President Biden’s recent proposed pandemic relief package that relate to the ACA and coverage. The $1.9 trillion American Rescue Plan includes several coverage-related proposals and would follow the pandemic relief passed by Congress in December 2020.
Regular readers know that the Trump administration—through the Centers for Medicare and Medicaid Services (CMS) and the Treasury Department—approved a broad waiver request from Georgia under Section 1332 of the ACA. The approved waiver authorizes the state to establish a reinsurance program for plan year 2022 and eliminate the use of HealthCare.gov beginning with plan year 2023. CMS and Treasury approved the waiver application on November 1, 2020. The history of Georgia’s waiver application and approval is summarized in prior posts as well as in the complaint filed in the lawsuit.
The reinsurance portion of the waiver is straightforward; of the 16 states with an approved Section 1332 waiver, all but one state has established a state-based reinsurance program. But the second part of the waiver application, known as the Georgia Access Model, is far more controversial. This is the broadest waiver yet to be approved under Section 1332 and relies on interpretations of Section 1332 made in much-criticized Trump-era guidance from 2018.
Critics have long argued that Georgia’s proposal fails to satisfy Section 1332’s procedural and substantive guardrails, meaning it could not be lawfully approved by the Trump administration. Given this controversy, legal challenges to the waiver approval were expected.
Planned Parenthood Southeast and the Feminist Women’s Health Center—represented by Democracy Forward—filed a lawsuit in federal district court in DC on January 14, 2021. The lawsuit alleges that the Trump administration’s 2018 guidance and approval of Georgia’s waiver are unlawful because these actions violate Section 1332 of the ACA and the Administrative Procedure Act (APA). The lawsuit also cites many of the Trump administration’s ongoing efforts to undermine the ACA as evidence that the 2018 guidance and waiver approval are part of a pattern of ACA sabotage.
In particular, the plaintiffs argue that the 2018 guidance and waiver approval are contrary to Section 1332, exceed the scope of the agencies’ authority (by allowing states to waive non-waivable provisions of the ACA), and are arbitrary and capricious. They also argue that the waiver approval failed to satisfy procedural requirements under the ACA and APA because Georgia and the Trump administration “rushed through the process without adequate time for public comment and without adequate clarification of how the state intends to approach key issues.” Here, the lawsuit points to the fact that Georgia went through four iterations of its waiver application, that its application was incomplete, and that only eight comments (less than one half of one percent) of the 1,826 total comments submitted during the most recent federal public comment period were in support of the Georgia Access Model.
As such, the plaintiffs ask the court to vacate both the approved waiver and the 2018 guidance and declare that they are unlawful. They also ask that the federal government be enjoined from taking further action on Georgia’s waiver or considering other waivers under the 2018 guidance. The plaintiffs acknowledge that the reinsurance portion of the waiver is uncontroversial and that the focus of the lawsuit is on the Georgia Access Model; however, the plaintiffs challenge approval of the waiver as a whole and ask the court to set aside the waiver in whole or in part. The plaintiffs have not sued Georgia, although it is possible that Georgia may ask to intervene in the litigation to defend its interests.
Much of the lawsuit turns on how the Trump administration interpreted the statutory guardrails under Section 1332 and long-standing concerns about direct enrollment and enhanced direct enrollment. Federal officials can grant a Section 1332 waiver only if a state demonstrates that their proposal meets certain statutory “guardrails.” These guardrails ensure that a waiver proposal will 1) provide coverage that is at least as comprehensive as ACA coverage ( “comprehensiveness” guardrail); 2) provide coverage and cost-sharing protections that are at least as affordable as ACA requirements (“affordability” guardrail); 3) provide coverage to at least a comparable number of residents as under the ACA ( “coverage” guardrail); and 4) not increase the federal deficit. The Obama administration issued guidance in 2015 on its interpretation of these guardrails.
In 2018, the Trump administration replaced that guidance and adopted its own interpretation, which many argued was inconsistent with Section 1332. The 2018 guidance tried to pave the way for the Trump administration to approve waivers where only some coverage under the waiver (instead of all coverage) satisfied the comprehensiveness and affordability guardrails. Under this view, waivers could be approved even if only some coverage under the waiver was as comprehensive, as affordable, and as available as coverage provided under the ACA. The 2018 guidance would also allow waivers to expand access to plans that do not have to meet the ACA’s requirements. (Separately, the Trump administration issued a final rule to codify the 2018 guidance’s interpretations into regulations.)
The lawsuit argues that the Georgia Access Model violates all four statutory guardrails because it will “drastically underperform the ACA.” The waiver proposal could lead to net enrollment losses in Georgia, which violates the coverage guardrail. The waiver could lead some consumers to enroll in non-ACA plans (such as short-term plans) with benefit gaps, which violates the comprehensiveness guardrail. And consumers will have to pay higher premiums and out-of-pocket costs through higher broker commissions, reduced competition, and adverse selection against the ACA markets, which violates the affordability guardrail and potentially the deficit neutrality guardrail (since higher ACA premiums mean higher federal outlays in the form of premium tax credits).
As health care providers in Georgia, Planned Parenthood Southeast and the Feminist Women’s Health Center allege they will be harmed for several reasons. They argue that the Georgia Access Model will make it more difficult and expensive for their patients to obtain health insurance. Fewer patients with health insurance will result in higher levels of uncompensated care. More uncompensated care will strain the plaintiffs’ resources and limit other services, such as community outreach. The loss of coverage resulting from the waiver will leave their patients in worse health and develop more complex treatment needs, making it more expensive for plaintiffs to treat those patients as a result. And approval of the waiver will make it more complicated for the plaintiffs to assist their patients with enrollment.
The lawsuit was assigned to Judge James E. Boasberg of the federal district court for DC. Health policy watchers know Judge Boasberg as the judge who repeatedly invalidated the Trump administration’s approval of state Section 1115 waivers with work and community engagement requirements. He is thus no stranger to assessing the legality of waiver approvals under the APA and other federal statutes.
The lawsuit will proceed, and the Biden administration will be responsible for filing a response in court. One potential option could be for the Biden administration to ask the court for a stay while it revisits the approved waiver and perhaps holds another round of public comment on the most recent version of the waiver (which, as the lawsuit points out, was never submitted for public comment). The Biden administration could consider any new comments in reevaluating approval of the Georgia Access Model.
If the federal government newly concludes that the proposal fails to satisfy the substantive guardrails, it could have grounds to amend, suspend, or terminate Georgia’s waiver, so long as certain procedures are followed. This is because the terms and conditions of the waiver agreement between the federal government and Georgia (as well as implementing regulations) always give the federal government “the right to suspend or terminate a waiver, in whole or in part, any time before the date of expiration, if the Secretaries determine that the state materially failed to comply with the terms” of the waiver.
Georgia’s waiver agreement includes some unique terms and conditions relative to waivers in other states. Those terms seem designed to limit the federal government’s ability to suspend or terminate Georgia’s waiver. But the federal government can do so as long as it complies with relevant procedures. This includes notifying Georgia of its determination, providing an effective date, and citing reasons for the amendment or termination (i.e., why the Georgia Access Model fails to satisfy Section 1332’s substantive guardrails). Georgia would have 90 days to respond, with the possibility of providing a corrective action plan to come into compliance with the waiver conditions. Georgia must also be given an opportunity to be heard and challenge the suspension or termination.
Alternatively, the Biden administration could regularly assess and monitor the state’s compliance with the terms and conditions and its progress, or lack thereof, in implementing the Georgia Access Model. Federal officials do this with all waivers. Under the waiver approval, Georgia must, for instance, satisfy requirements related to funding, reporting and evaluation, development of an outreach and communications plan, and operational standards for eligibility determinations. If Georgia fails to comply with these terms and conditions, that too would be grounds to initiate the process to amend or terminate parts or all of Georgia’s waiver.
On January 14, a few days before taking office, President Biden issued a 19-page fact sheet outlining his proposed American Rescue Plan to contain the COVID-19 virus and stabilize the economy. The announcement praised the bipartisan package adopted in December 2020 as “a step in the right direction” but notes that Congress did not go far enough to fully address the pandemic and economic fallout. Following Inauguration Day, Biden is expected to lay out an additional economic recovery plan.
Among many other initiatives, the comprehensive $1.9 trillion plan would provide funding for a national vaccination program, create a new public health jobs program, provide funding for schools to reopen safely, extend and expand emergency paid leave, extend and expand unemployment benefits, raise the minimum wage, and deliver $1,400 in support for people across the country. The Biden plan also calls for preserving and expanding health insurance, noting that 30 million people were uninsured even before the pandemic and that millions may have lost job-based coverage in 2020.
First, the American Rescue Plan calls for Congress to provide COBRA subsidies through the end of September. Presumably, these subsidies would be available from the beginning of 2021, rather than subsidizing premiums from 2020. COBRA subsidies during an economic emergency are not new. Congress subsidized COBRA premiums during the 2008 recession, with mixed results. Full COBRA subsidies were included in the original Heroes Act passed by the U.S. House of Representatives in May 2020, although not in the revised Heroes Act that was passed by the House in October 2020. But neither bill was ever taken up by the U.S. Senate. It is not clear from the fact sheet whether the Biden administration is aiming for full COBRA subsidies where the government would pay 100 percent of the premiums for COBRA coverage for laid-off workers and furloughed employees—or some other amount (e.g., 80 percent of premiums).
Second, the American Rescue Plan would accomplish one of candidate Biden’s key campaign promises by expanding and increasing the value of premium tax credits under the ACA. Democrats in Congress have repeatedly passed legislation that would accomplish what the American Rescue Plan fact sheet seems to call for. For instance, the Patient Protection and Affordable Care Enhancement Act—passed by the House in July 2020—would have expanded the availability of premium tax credits to those whose income is above 400 percent of the federal poverty level and made those credits more generous by reducing the level of income that an individual must contribute towards their health insurance premiums to 8.5 percent for those with the highest incomes. This subsidy expansion and enhancement would improve the affordability of coverage for millions of Americans who purchase coverage in the individual market.
Beyond COBRA and ACA subsidies, the American Rescue Plan calls for additional funding for veterans’ health care needs and for the Substance Abuse and Mental Health Services Administration and the Health Resources and Services Administration to expand access to behavioral health services. The proposal would also increase the federal Medicaid assistance percentage (FMAP) to 100 percent for the administration of COVID-19 vaccines to help ensure that all Medicaid enrollees will be vaccinated. The proposal does not appear to otherwise mention Medicaid, which is serving as a key safety net as incomes have dropped for millions of Americans, despite bipartisan support for an enhanced FMAP during the pandemic.

The figures are the last from the Trump administration, which has drastically reduced money toward navigators who help people use the Healthcare.gov website and find the best ACA plan for them. The administration has made no secret of its opposition to the law and after failing to overturn it in Congress has used executive actions to undermine it.
Still looming is the Trump administration’s lawsuit seeking to overturn the landmark law.
President-Elect Joe Biden and his pick for HHS chief, California Attorney General Xavier Becerra, however, are eager supporters and are likely to take a number of actions to restore and burnish it. That could be increasing tax credits and subsidies, increasing navigator funding and building on protections like essential health benefits.
The U.S. Supreme Court is expected to make its ruling on the ACA case later this spring or summer, but the Biden administration could essentially make it moot by walking back the zeroing out of the individual mandate penalty that is the linchpin of the lawsuit against it.
The relatively steady enrollment could be increased through those actions and the possibility of a special enrollment period to account for needs during the coronavirus pandemic. The COVID-19 crisis and the recession it has caused have kicked millions of people off their employer-sponsored insurance, and they could turn to the exchanges for coverage, especially with higher tax credits and subsidies.

The number of new unemployment claims filed last week jumped by 181,000 the week before to 965,000, the largest increase since the beginning of the pandemic.
It was the largest number of new unemployment claims since August.
An additional 284,000 claims were filed for the Pandemic Unemployment Assistance, the insurance for gig and self-employed workers.
The weekly report is President Trump’s last before President-elect Joe Biden is sworn in on Jan. 20. Biden will inherit a labor market badly weakened by the coronavirus pandemic and an economic recovery that appears to have stalled: 140,000 people lost their jobs in December, the first decline in months, with the U.S. still down millions of jobs since February.
The dire numbers will serve as a backdrop for Biden as he formally unveils an ambitious stimulus package proposal on Thursday, which could top $1 trillion, and is expected include an expansion of the child tax credit, a $2,000 stimulus payment, and other assistance for the economy.
Democrats were already using the weak labor to argue about the necessity of more aid.
Economists say that the economy’s struggles could be explained, in part, by the delay Congress allowed between the summer, when many fiscal aid programs expired and December, when lawmakers finally agreed on a new package after months of stalemate.
The number of new jobless claims has come down since the earliest days of the pandemic, but remains at a extremely high level week in and week out.
The total number of continuing people in any of the unemployment programs at the end of the year was 18.4 million, although officials have cautioned that the number is inflated by accounting issues and duplicate claims.
The increase in claims is not entirely unexpected. As the aid package passed by Congress in December kicks in, including a $300 a week unemployment supplement, some economists expected that to result in more workers filing claims.


Fewer than four in every 10 American adults can afford a $1,000 surprise medical bill, according to survey results released Jan. 11 by finance company Bankrate.
Bankrate surveyed 1,003 Americans about their personal finances from Dec. 8 to 13, finding a 2 percent drop from the previous year in respondents who said they could comfortably cover a $1,000 expense. The study noted that credit card finance charges can often add up to hundreds of additional dollars when surprise expenses are not paid quickly.
However, some Americans have an optimistic outlook on their financial situation going forward, with 44 percent of respondents believing their personal finances will improve in 2021.
https://thehill.com/policy/finance/533242-december-jobs-report
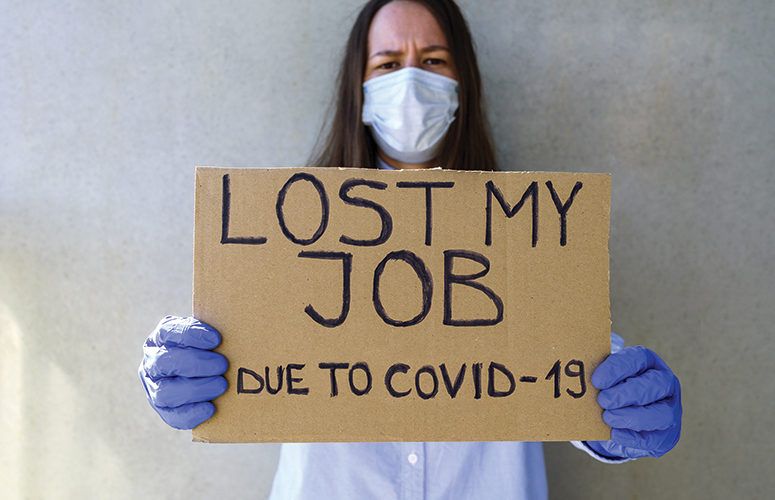
The economy lost 140,000 jobs in December, the first reported losses since April, as the unemployment rate remained steady at 6.7 percent.
Economists expected a small jobs gain of nearly 50,000. The drop is the latest sign of a weakening economy amid the ongoing COVID-19 crisis. All in all, the economy remains about 10 million jobs below its pre-pandemic levels.
“There’s not much comfort to be taken from the stable unemployment rate, given that millions of Americans have left the labor force with nearly 11 million listed as officially out of work,” said Mark Hamrick, senior economic analyst at Bankrate.com.
“Between the human and economic tolls taken by the pandemic, these are some of the darkest hours of this soon-to-be yearlong tragedy.”
The biggest losses were concentrated in leisure and hospitality, a sector particularly vulnerable to the effects of the pandemic, which lost an astonishing 498,000 jobs.
State and local government payrolls shed 51,000 jobs. Congress deferred passing state and local aid in its latest COVID-19 relief bill.
But the overall loss would have been worse had it not been for gains in professional and business services, which added 161,000 jobs; retail trade, which added 120,500 jobs; and construction, which added 51,000.
Some demographic groups have been hit harder by the economic downturn.
The unemployment rate for Hispanics rose to 9.3 percent in December, while Black unemployment remained elevated at 9.9 percent. The rate for whites was 6 percent, and for Asians it was 5.9 percent.
Over a third of jobless people have been unemployed for over 27 weeks.