
Cartoon – If You’d like some False Hope



The COVID-19 pandemic has catapulted the telehealth industry forward by decades in a matter of months, according to Amwell’s Roy Schoenberg.
That not only benefits the Amwell’s business, but it’s a win for patients, said Schoenberg, who serves as the company’s president and co-CEO.
“We are going to see an enormous amount of change, nothing short of a revolution, going forward,” he told Fierce Healthcare.
Roy and his brother Ido Schoenberg have been telehealth advocates for more than a decade since launching Amwell, formerly American Well, in 2006. The Boston-based telehealth company works with more than 240 health systems comprised of 2,000 hospitals and 55 health plan partners with over 36,000 employers, reaching over 150 million lives.
Like other virtual care companies, Amwell has seen skyrocketing demand for its services during the COVID-19 pandemic as stay-at-home orders and social distancing guidelines prevented many patients from visiting doctors in person. Shares in public digital health companies like Teladoc and Livongo have grown by double digits during the health crisis.
The momentum around telehealth also has attracted investors. The company recently raised $194 million in a series C funding round.
Amwell also is gearing up to go public later this year, according to CNBC’s Christina Farr and Ari Levy. The company confidentially filed for an IPO earlier this week and has hired Goldman Sachs and Morgan Stanley to lead the deal, Farr and Levy reported last week, citing people who asked not to be named because the plans have not been announced.
The company declined to comment on the CNBC report.
Before the COVID-19 pandemic began, Amwell was providing an average of 5,000 telehealth visits a day. That has jumped to 45,000 to 50,000 virtual visits a day due to the coronavirus, said Ido Schoenberg, who serves as chairman and co-CEO.
“We saw 30 times, 40 times higher volumes and we have clients that had 2% to 3% of their patient volume online that now have 75% of visits online,” he said. “It’s truly incredible. The number of active providers on our platform grew seven times over in two months.”
As visits surged, technology companies struggled to keep up with demand, and patients reported long wait times for virtual visits on some platforms.
Roy Schoenberg acknowledged Amwell also faced challenges rapidly scaling its technology and services almost overnight as it was “thrown into the center stage of trying to save the world.”
The company leverages automation for processes such as onboarding physicians, credentialing, licensing, and working with health plans and that capability proved critical to scaling its services, the executives said.
“We needed to allow 40,000 to 50,000 physicians to come on to our system and begin to use it. If this was a manual process, it would have been broken,” Roy Schoenberg said.
Regulatory barriers to telehealth also quickly fell away, at least temporarily. The Centers for Medicare and Medicaid Services and commercial health plans have expanded access to telehealth by offering payment parity for many telehealth services for the first time.
While questions remain about what regulatory flexibilities will remain in place to support the ongoing demand for telehealth, Amwell executives believe virtual care has proven its value to providers, payers and patients.
CMS will likely tighten up some of the relaxed requirements around telehealth which is a “fiscally responsible approach,” Roy Schoenberg said.
“At the end of the day, even though the government tends to be a little bit slow, it gravitates to where the value is. How long will it take for the payment structure to retract and then expand, that’s anyone’s guess. We have an election year coming in. Who knows what that is going to do? There may be some changes, but I think overall, the genie is out of the bottle, the toothpaste is out of the tube, or whatever phrase you want to use,” he said.
The executives never doubted that telehealth would, at some point, reach the mainstream. Now that it’s happened, health systems and patients have become advocates for the technology and that will also put pressure on CMS and commercial payers to continue to support it, they said.
The executives now see an opportunity for Amwell to use its platform to expand the reach of healthcare to more patients. There is a growing industry of telehealth providers, device makers, and technology-enabled disease management companies that will enable digital home healthcare services, they said.
“What we built is something way bigger than a video conference between doctor and patient, which you can easily do using Zoom or FaceTime,” Ido Schoenberg said.
Digital connectivity will enable providers to gather health data on patients from wearables and devices to better understand gaps in care, get an overall picture of patients’ health and then provide more effective interventions, all without patients leaving their living rooms. The combination of telehealth and remote devices will enable elderly, frail patients to receive care at home, where they want to be, rather than being moved to a skilled nursing facility, they said.
“It’s about the ability to democratize healthcare and make great care available to many more people that today don’t always have access to it,” Ido Schoenberg said.
Roy Schoenberg added, “These are the opportunities opening fast and furious in front of us and the promise is to make healthcare less painful as an individual experience. That’s the value proposition.”

Geisinger Health System has inked a 10-year technology agreement with Siemens Healthineers to access diagnostic imaging equipment and artificial intelligence applications.
The Danville, Pennsylvania-based health system said the partnership will advance and support elements of its strategic priorities related to continually improving care for their patients, communities and the region.
The medical technology company will provide Geisinger access to its latest digital health innovations, diagnostic imaging equipment and on-site staff to support improvements. Education and workflow resources will also be available, which will provide Geisinger staff with the ability to efficiently make decisions and continually optimize workflows, the companies said.
Siemens provides AI-based radiology software that analyzes chest CT scans, brain MRIs and other images as well as AI-based clinical decision support tools and services to help advance digitization.
Financial terms of the deal were not disclosed.
“By expanding our relationship with Geisinger, this becomes one of the largest value partnership relationships in North America and will allow us to work together to improve the patient experience for residents of Pennsylvania and the region,” said David Pacitti, president and head of the Americas for Siemens Healthineers, in a statement.
“Making better health easier by bringing world-class care close to home is central to everything we do at Geisinger,” said Matthew Walsh, chief operating officer at Geisinger. “This partnership will allow us to continue to equip our facilities with the most advanced diagnostic imaging technology in the market to care for our patients.”
Michael Haynes, associate vice president of operations, Geisinger Radiology, said the collaboration with Siemens will enable the health system to identify and respond to health concerns more quickly.
Geisinger operates 13 hospitals across Pennsylvania and New Jersey as well as a 600,000-member health plan, two research centers and the Geisinger Commonwealth School of Medicine.
Partnerships between health systems and tech companies are becoming fairly common as the healthcare industry pushes forward to use data analytics, AI and machine learning to improve clinical diagnosis and better predict disease.
Mayo Clinic announced a high-profile, 10-year strategic partnership with Google in September to use advanced cloud computing, data analytics, machine learning and AI to advance the diagnosis and treatment of disease.
Providence St. Joseph Health inked a multiyear strategic alliance with Microsoft to modernize its health IT infrastructure and leverage cloud and AI technologies.

Effective pandemic response requires real-time, accurate data sharing between providers and public health agencies, allowing the government to track outbreaks and allocate resources as needed.
A lack of nationwide, interoperable reporting infrastructure has been one of the major criticisms of the Trump administration’s handling of the pandemic, which has infected almost 1.7 million and killed 99,000 people in the U.S. as of Wednesday.
CMS requires hospitals be able to electronically send and receive health information, including lab results and syndromic surveillance data, to and from public health agencies like their state’s department of health. For more than a decade, providers have funneled significant resources into their IT infrastructure due to a slurry of federal incentive programs, though EHR implementation remains piecemeal across the U.S. due to cost and other barriers.
The JAMIA study, one of the first looking at the state of health data reporting, analyzed 2018 American Hospital Association data to identify hospital-reported barriers to surveillance data reporting, and Harvard Global Health Institute data on the coronavirus pandemic’s projected impact on hospital capacity at the hospital referral region (HRR) level. Researchers assumed a 40% population infection rate over 12 months.
The group found 31 high-need HRRs, those in the top quartile of projected beds needed for COVID-19 patients, with more than half of the hospitals in the region saying the relevant public health agency couldn’t electronically receive data.
That suggests areas more likely to be overwhelmed by the pandemic had some of the least interoperable data-sharing capabilities going into it, hamstringing outbreak response.
Researchers found the most common barrier to data-sharing nationwide, reported by 41% of hospitals, was that public health agencies didn’t have the capacity to receive data electronically.
The next most common, reported by 32% of hospitals, was interface-related issues, such as costs or implementation complexity; followed by difficulty extracting data from the EHR (14% of hospitals reporting), different data standards (also 14%), hospitals lacking the capacity to send data (8%) and hospitals being unsure what public health agencies to send the data to (3%).
Researchers also found significant state variance in hospitals saying public health agencies couldn’t receive needed data electronically, running the gamut from 83% of hospitals saying so in Hawaii and Rhode Island to 40% in New Jersey and Virginia to none in Delaware.
Geographic variation is likely due to different funding priorities in different places, as some agencies may only be able to receive specific data elements or interface with a select number of EHRs. This spotty IT implementation results in a patchwork picture of disease progression across the U.S., though the Centers for Disease Control and Prevention is working to automate the COVID-19 reporting process.
The study does have some significant limitations. It’s a relatively one-sided portrayal of the issue, as researchers did not have access to data or survey results from public health agencies. And, since AHA survey results were from two years ago, the EHR landscape could have shifted since 2018.
However, researchers called upon policymakers to build up public health agencies’ IT capabilities, especially as states begin to reopen despite an increasingly likely resurgence of the virus in the fall.
“Policymakers should prioritize investment in public health IT infrastructure along with broader health system information technology for both long-term COVID-19 monitoring as well as future pandemic preparedness,” authors A Jay Holmgren, a doctoral candidate at Harvard Business School; Nate Apathy, a doctoral candidate at Indiana University’s Richard M. Fairbanks School of Public Health; and Julia Adler-Milstein, a professor at University of San Francisco Department of Medicine, wrote.
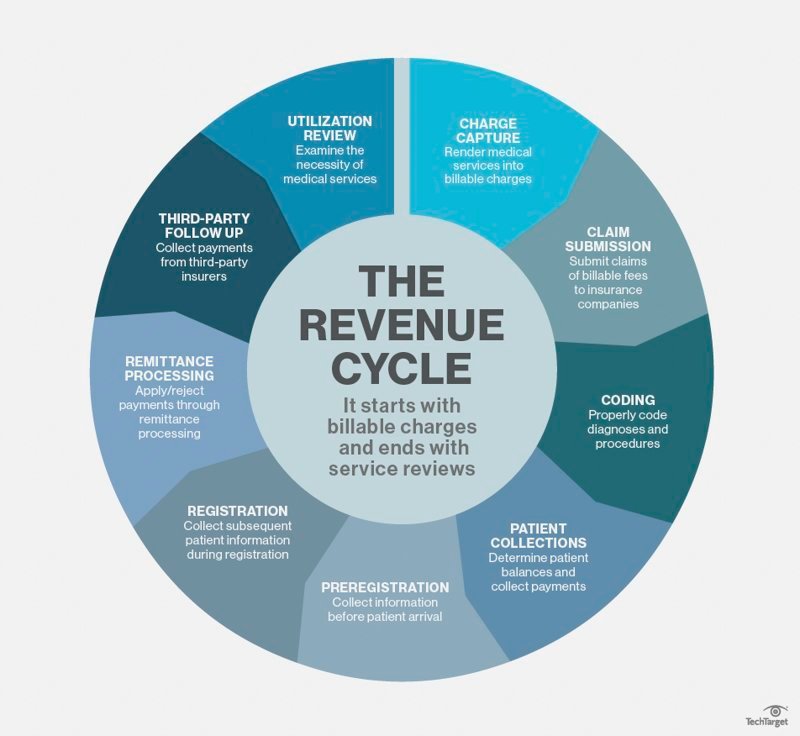
Keys to achieving revenue integrity and compliance across your organization
It’s old news: Revenue cycle complexity continues to increase, exacerbating existing challenges. And as we tackle those, new ones arise to take their place.
Ever-changing regulations are a given, but adopting value-based reimbursement (VBR) models currently poses a major challenge. New payment models complicating revenue cycle activity become more difficult with additional quality reporting and other requirements. Add in the operational realities of siloed workflows, data proliferation, and disparate systems, and it’s clear why efficient collaboration can seem nearly impossible. Intelligent middle revenue cycle operations that manage to these challenges are vital to achieving revenue integrity and financial stability.
Use the right solutions at the right time
Today’s environment requires sharpening the way you ensure revenue integrity. Providers need an easy, seamless way to manage middle revenue cycle operations, and there are several effective strategies to accomplish that. Of course, it’s important to recognize and make use of your EMR system’s capabilities. It’s also essential to leverage complementary technologies with specific core competencies that will improve revenue cycle performance. For example, a solution that continuously monitors records in real time enables timely auditing, coding adjustments and case completion to reduce billing turnaround and reimbursement delays.
Take a smart approach to enabling technology
Augmenting your core systems with complementary technologies or capabilities on a single, integrated platform makes it much easier to support internal collaboration between different departments or teams. An integrated platform also enables you to seamlessly deploy additional capabilities onto that platform, ensuring speed to value. Instead of using multiple disparate tools, a shared platform enables interdepartmental communication and helps minimize inefficiency. A smart technology platform that crosses departmental siloes and brings transparency across teams is critical. Platforms that leverage clinically aware artificial intelligence and other automation enable staff to proactively focus on the areas where their expertise has the most impact. In addition, when leveraging an integrated platform, one expert team’s work will not get cancelled out by another team’s contributions.
Regardless of which core system you use, integrating technology with targeted competencies and connectivity adds value to the EMR. It can provide a depth of specialized expertise that drives better documentation, coding and real time audit interaction — keys to a high-performing revenue cycle.
Prioritize comprehensive, correct documentation and coding
Unfortunately, it seems the battle against claim denials is here to stay. You can’t overlook the importance of front-end data validation to eliminate rework and inefficiency. However, the ability to ensure complete and accurate clinical documentation for every case will significantly impact revenue capture and reduce the inefficiency of denials and rework.
Broaden the scope of your CDI program with technology that uses clinical intelligence to drive concurrent documentation review for all payers. Getting it right up front contributes to better coding, accurate reimbursement, and appropriate quality measures, all of which are vital to success under VBR.
Increase collaboration with payers
As long as payers and providers continue working at odds, the costly onslaught of denials will persist. In a perfect world, both sides would join forces to find mutually beneficial solutions for claim errors, denials and payment delays. Imagine the savings in administrative inefficiency alone. However, we’re not in that world yet. Therefore, it’s important to make a proactive effort to understand the specifics of each payer’s contract and adjust your internal processes and technology rules accordingly. As operating margins get smaller, organizations have no choice but to increase efficiency and accuracy, and working together with payers can contribute significantly to that goal.
Consolidate, collaborate, communicate
Industry pressures to improve performance are unrelenting, especially around smart solutions, innovation, and increasing both efficiency and the bottom line. Organizations are expected to improve these areas while, at the same time, enabling patient-centric operations. One way to achieve this is to leverage innovative, integrated tools to augment core systems and promote partnership, communication and efficiency across multiple related disciplines.
Consider clinical documentation, coding and auditing. Numerous departments need pieces of that information for different reasons, including utilization review, medical necessity determinations, chart audits and quality monitoring, in addition to bill preparation. A single repository containing up-to-date data in a real-time view driven by supporting workflow, rules and alerts provides consistent and reliable information when and where it’s needed.
As patient care becomes more complex, so does the middle revenue cycle. Seek solutions that will simplify and manage the complexity in an administratively efficient way. Consider your prospective vendor’s core competencies when evaluating solutions and look for integration and intelligent automation that will add the most value to your organization.

HP has unveiled advanced security for businesses and their remote workforces and disclosed an extensive guide to disinfecting your laptop and other computer equipment.
The new offerings include HP Pro Security Edition, HP Proactive Security, and HP Sure Click Enterprise. These are aimed at the security threats that evolve and disrupt business every day.
With the recent surge of remote workers — due to work-from-home rules forced upon us by COVID-19 — HP said we must all be aware of the increased risks of working from home. Over 80% of home office routers have been found to be vulnerable to potential cyberattacks.
Emails also pose a significant risk to organizations, with over 90% of PC infections originating from attachments and 96% of security breaches not discovered until months later. There are 5 billion new threats per month, based on HP’s estimates.
“Our HP Pro Security Edition takes Sure Sense and Sure Click and bundles [them] with our system,” said Andy Rhodes, global head of commercial PCs, in a press briefing. “Endpoints are still an enormous risk — 90% of infections originate with emails. Every user is at risk here.”
HP Pro Security for small businesses.

With public health concerns over COVID-19 spreading worldwide, HP wants customers to have the information they need to effectively clean HP devices and maintain a healthy work environment.
The Centers for Disease Control and Prevention (CDC) recommends cleaning surfaces, followed by disinfection, as a best practice for the prevention of COVID-19 and other viral respiratory illnesses in households and community settings.
In fact, HP has issued its own whitepaper for cleaning your devices.
“We get asked [about] this every day,” said Rhodes. “If you use the wrong disinfectant, you can actually damage the product.”
A CDC-recommended disinfectant that is also within HP’s cleaning guidelines is an alcohol solution consisting of 70% isopropyl alcohol and 30% water.
The steps below use the CDC-recommended alcohol solution to clean high-touch, external surfaces on HP products:

Here are five quick notes on Epic and the EHR market.
1. More than 250 million patients have electronic records in Epic.
2. Epic has 28 percent of the acute care hospital market, according to a KLAS report.
3. There were 163 hospitals with 500-plus beds that used Epic in 2018, the most recent year reported. The second most-used EHR in that group was Cerner, with 77 hospitals that have 500 or more beds.
4. Epic implementation among small practices is increasing as those practices with one to 10 physicians join or affiliate with larger organizations. Among those groups, 93 percent said Epic Community Connect is part of their organization’s long-term plans and 93 percent said they would purchase the software again, according to KLAS.
5. Over the past five years, at least 11 hospitals and health systems switched from Cerner to Epic, including most recently AdventHealth in Florida and Atrium Health in North Carolina.
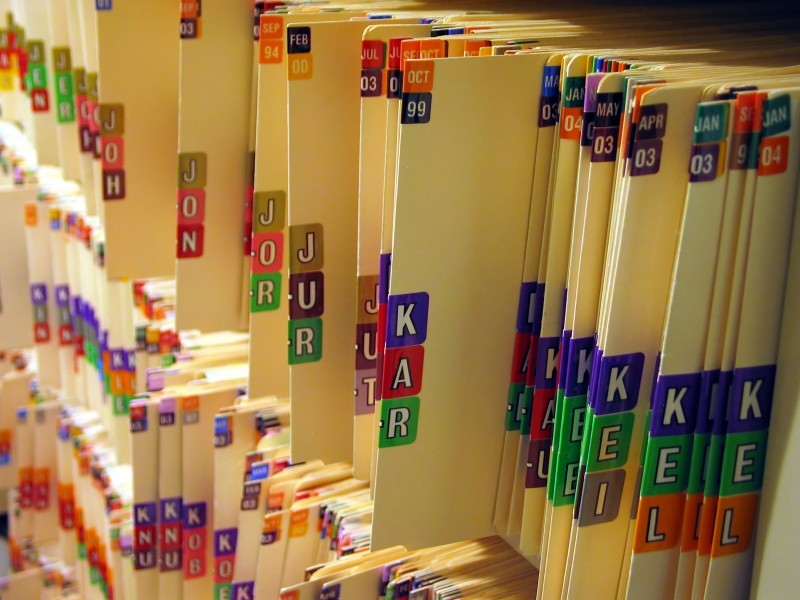
HHS released its much-anticipated final rules on EHR interoperability, ruling against “information blocking” tactics by EHR vendors and giving patients more control over their medical records.
The new rule will be applied over the next two years and will make patient records downloadable to smartphones using consumer apps. Overall, members of the healthcare industry applaud these efforts to make patient information more accessible to improve healthcare delivery. However, there are privacy concerns around how patient data can be used once downloaded to third-party consumer apps that weren’t addressed in the final rule.
Here is a brief list of a few potential winners and losers of the new rule.
WINNERS
Patients. Patients now have more control over their medical records and will be able to access them through third-party apps for free, which will make it easier for them to take their medical records to new providers outside of their previous provider’s system. As a result, they will have more choice in where they go for healthcare.
Hospitals and physicians. The lengthy process of trying to convert a patient’s medical records will be unnecessary. Patients will no longer need to have their medical records faxed between healthcare facilities in different networks and the rule will streamline workflow around gathering patient data to provide the best possible care. Hospitals participating in Medicare and Medicaid will also be able to send electronic notifications to other facilities or providers when a patient is admitted, transferred or discharged under its new “Coordination of Participation” rule.
App developers and health IT startups. App developers that allow patients to store their health data and medical information will have access to that data, a virtual gold mine. The federal privacy protections limiting how providers and insurers share medical records do not apply when patients transfer data to consumer apps, according to the New York Times.
Apple and Microsoft. Healthcare providers will be required to send medical data in a format that is compatible on third-party apps including Apple Health Records. Microsoft is also working to sell technology in the health sector, and the new rule will make it easier, according to CNBC.
LOSERS
Patients. While the rule has many benefits to patients, there is also potential for disaster. Patients who download their medical information on consumer apps may find their information shared or sold. There could also be additional security issues if those apps are hacked. Finally, some patients may become confused by their medical records and notes if the information isn’t stated clearly, causing further anxiety around their care.
Hospitals and clinics. Patient leakage may become more common if it’s easier for patients to take their medical records with them. Healthcare organizations will also need to prepare for an influx of patient data and have strong governance procedures in place as they partner with payers and other organizations to incorporate clinical data with patient-gathered data and potentially social determinants of health data.
EHR vendors. EHR companies must now adopt application programming interfaces so their systems can communicate with third-party apps. EHR companies have two years to comply and face up to $1 million per violation for engaging in “information blocking.” The new focus on interoperability may also pave the way for competitors to gain market share over the two most dominant players, Epic and Cerner.
Epic. Epic was a notable opponent to the HHS interoperability rules, citing patient privacy concerns. If forced to collaborate with other companies, Epic could potentially lose its edge over competitors, according to an op-ed written by former HHS Secretary Tommy Thompson in the Wisconsin State Journal. He contended Epic would have to “give its trade secrets away to venture capitalists, Big Tech, Silicon Valley interests and overseas competitors for little or no compensation.” Epic is also the most dominant EHR, holding 28 percent of the acute care hospital market, which could be threatened by greater interoperability. However, in response to the final rule’s release, Epic issued a statement saying that it would focus on “standards-based scope for meaningful interoperability.”