A bipartisan Senate report on private equity ownership of two health systems shows PE investment puts a priority of profit over patient health and hospital finances.
A yearlong investigation found that patient care deteriorated at both systems, while private equity owners received millions, according to the Senate Budget Committee’s bipartisan staff report, “Profits Over Patients: The Harmful Effects of Private Equity on the U.S. Health Care System.”
The investigation was led by Senate Budget Committee Chairman Sheldon Whitehouse, D-R.I., and Ranking Member Charles E. Grassley, R-Iowa.
WHY THIS MATTERS
The report centered on the hospital Ottumwa Regional Health Center in Iowa and its operating company, Lifepoint Health in Tennessee.
Private equity company Apollo Global Management owns Lifepoint Health.
The investigation expanded to include other entities, including PE firm Leonard Green & Partners and hospital operator Prospect Medical Holdings, in which Leonard Green & Partners held a majority stake. Leonard Green & Partners (LGP) is a private equity firm in Los Angeles that owns hospitals under Prospect Medical Holdings (PMH).
“LGP and PMH’s primary focus was on financial goals rather than quality of care at their hospitals, leading to multiple health and safety violations as well as understaffing and the closure of several hospitals,” the report said.
The investigation originated from questions over the role, if any, private equity played in a series of patient sexual assaults by a nurse practitioner at the Iowa hospital. In 2022, a nurse practitioner fatally overdosed on drugs acquired at the hospital. Police discovered the nurse had sexually assaulted nine incapacitated female patients over a two-year period, the report said.
Prospect Medical Holdings owns and operates hospitals in urban and suburban areas, primarily on the East and West Coasts, including Connecticut, Rhode Island, Pennsylvania and California.
It is a previously public traded company that went private in 2010 when LGP acquired a 61% majority stake. During the course of LGP’s majority ownership, Prospect Medical Holdings acquired 16 hospitals over a span of four years. PMH has operated a total of 21 unique hospitals, the report said.
Apollo has a 97% ownership stake in Lifepoint Health, a company that owns and operates acute care hospitals in predominantly rural areas. This includes Ottumwa Regional Health Center. Apollo owns around 220 hospitals nationwide, making it the single largest private equity owner of hospitals in the United States, the report said.
Ottumwa has been under PE ownership since 2010, when it was acquired by the PE-owned hospital operator RegionalCare, which was later acquired by Apollo.
KEY FINDINGS
The report’s key findings show that LGP controlled the Prospect Medical Holding board of directors, which incentivized management to satisfy financial goals regardless of patient outcomes.
“According to documents obtained by the committee, discussion amongst PMH and LGP leadership during board meetings centered around profits, costs, acquisitions, managing labor expenses and increasing patient volume – with little or no discussion of patient outcomes or quality of care.”
Current PMH leadership has overseen the closure of eight hospitals, with three-fourths coming during or directly after LGP’s majority ownership, including four in Texas and two in Pennsylvania.
Several hospitals suffered from labor cuts, decreased patient capacity, unsafe building maintenance and financial distress, the report said.
Despite this, LGP took home $424 million of the $645 million that PMH paid out in dividends and preferred stock redemption, in addition to over $13 million in fees, leaving PMH in severe financial distress.
In order to pay investors dividend distributions, PMH was forced to take on hundreds of millions of dollars in debt, running out of cash and defaulting on its loans, the report said.
ORHC’s PE owned companies, including Lifepoint Health, have failed to fulfill at least seven promises, including legally binding ones made to Ottumwa, including those related to growth, physician recruitment, routine capital expenditures, charity care, patient satisfaction and continuation of services.
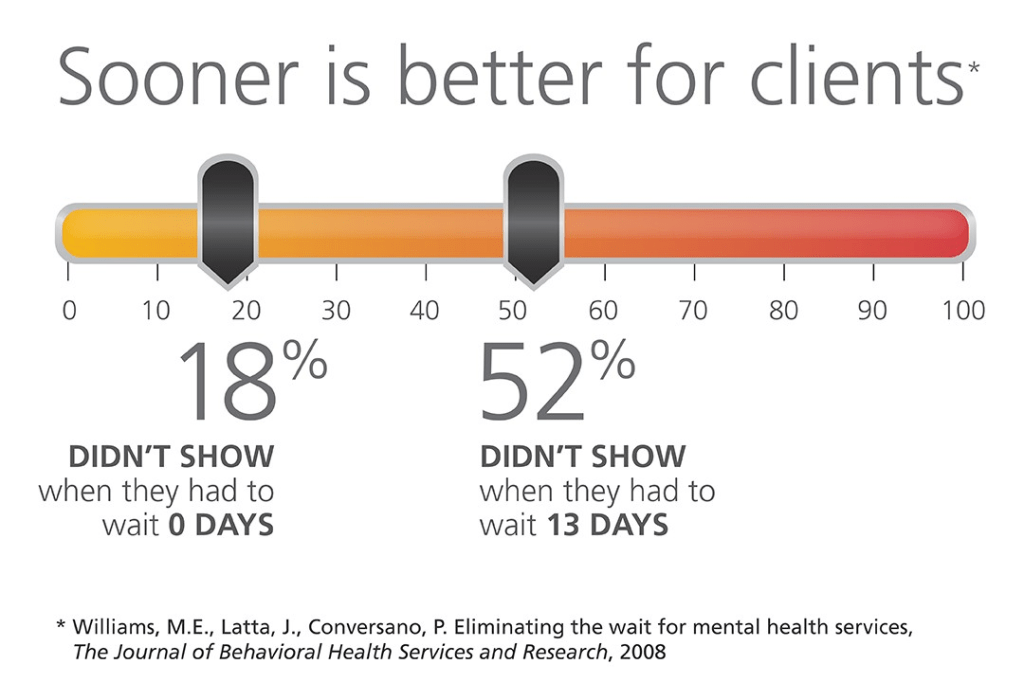
Patient volumes have decreased, likely due to long wait times in the ER, outgoing transfers, insufficient staffing and a lack of specialists, the report said. This has also resulted from having a poor reputation in the community.
Because of financial harm, OTHC is dependent on Lifepoint Health to pay its expenses.
However, Lifepoint pays Apollo $9.2 million annually in management fees, as well as a 1% transaction fee each time Lifepoint completes an acquisition, which included a $55 million fee in relation to the acquisition of Lifepoint Health in 2018.
THE LARGER TREND
PE and other private funds had less than $1 trillion in managed assets in 2004, but now manage more than $13 trillion globally. PE firms create affiliated funds with money raised from investors, such as pension funds, foundations and insurance companies. The intention is generating returns for their investors within a short period of time.
PE has grown in healthcare. In the 2010s investors spent more than $1 trillion. By 2021 PE investment had reached an all-time high of 515 deals valued at $151 billion.
ON THE RECORD
“Recent peer reviewed studies have generally found negative consequences for general acute care hospitals during the first three years of PE ownership as compared to non-PE owned hospitals, including lower quality of care, increased transfers to other hospitals, decreased staffing and higher prices,” the report said.