https://www.politico.com/story/2018/03/06/obamacare-democrats-white-house-insurance-stable-388816

The White House is seeking a package of conservative policy concessions — some of which are certain to antagonize Democrats — in return for backing a legislative package bolstering Obamacare markets, according to a document obtained by POLITICO.
The document indicates the administration will support congressional efforts to prop up the wobbly marketplaces, in exchange for significantly expanding short-term health plans and loosening other insurance regulations.
The document also makes severalreferences to abortion language that will be problematic for Democrats. A potential stumbling block in passing any stabilization package is whether conservatives will insist on including language prohibiting the use of government dollars to pay for abortions.
“Although congressional efforts to provide taxpayer money to prop up the exchanges is understandable, any such efforts must also provide relief to middle-class families harmed by the law and protect life,” the document states.
The source of the document provided to POLITICO isn’t identified and it isn’t dated. The White House declined to comment on the document but didn’t question its authenticity. A spokesperson for HHS said the department does not comment on leaked documents.
Two health policy experts who have been in contact with White House officials indicated that the document is consistent with ideas the administration has discussed for creating more stability and flexibility in the insurance markets.
“It’s legit,” said one former White House policy official.
Republican and Democratic lawmakers have been in delicate negotiations over a stabilization package that could clear the House and Senate. Democrats want to bolster the federal health care law after Republicans failed in their efforts to repeal it last year.
The list of White House policy requests includes allowing insurers to charge older enrollees up to five times as much as their younger counterparts, as opposed to the current three-to-one cap. That policy would require amending the Affordable Care Act.
The White House is also seeking to allow short-term plans — which offer skimpier benefits with lower premiums — to be renewed. Short-term plans, exempt from Obamacare rules, can deny people coverage or charge them more based on a health condition, in a process known as underwriting. The Trump administration recently proposed expanding the maximum length of these plans from three months to one year. However, the White House document envisions allowing people to renew this coverage “without those individuals going through health underwriting.”
The document doesn’t include support for reinsurance, which insurers have been pushing to shield them from the costs of particularly expensive customers.
The document also reiterates that the administration supports funding for cost-sharing reduction payments, which Trump cut off in October. The president’s budget proposal including funding for the payments, which help insurers reduce out-of-pocket costs for low-income Obamacare customers.
There is at least one item on the White House list that could garner bipartisan support: Expanding the use of health savings accounts. Last week, a bipartisan group of House members introduced a package of potential changes, and business groups have been pushing for HSA proposals to be part of the appropriations package Congress must pass by March 23.
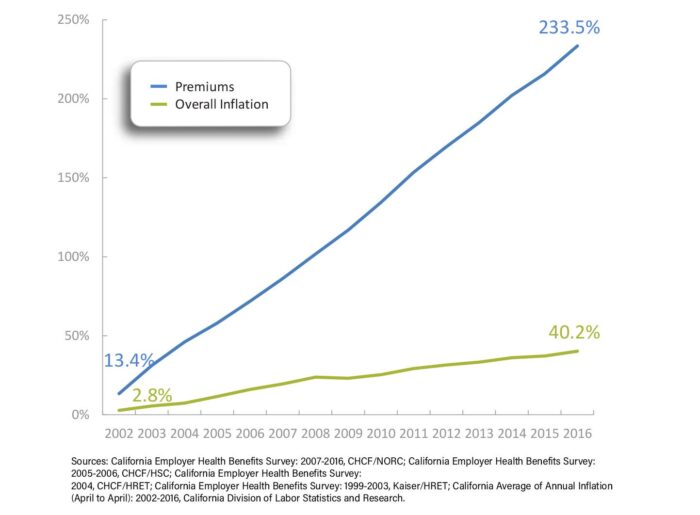
Republicans fear another year of eye-popping premium increases will hit voters just before Election Day — and that they’ll get the blame this time since they’re now in charge.
But the White House asks could further unsettle those talks. In particular, the emphasis on abortion language tripped up earlier negotiations.
Democrats have been seeking a very different list of policies to boost the markets. They want to increase the subsidies provided to Obamacare customers, reinstate funding for outreach and marketing, and prevent the executive branch from expanding the availability of what they deride as “junk” insurance plans.
“People nationwide are looking at higher premiums and out-of-pocket costs as a direct result of the damage President Trump has done on health care,” said Sen. Patty Murray (D-Wash.), who has been in the middle of negotiations over a stabilization package, in a statement to POLITICO. “I certainly hope the president and Republican leaders won’t once again sabotage an opportunity to undo some of the damage they’ve done by choosing to play politics with women’s health and making last-minute, harmful demands that would raise families’ costs even more and place an age tax on seniors.”