Last week, J.P. Morgan hosted its 44th annual healthcare conference, with over 500 companies and 8,000 people in attendance to discuss health system performance, pharmaceutical trends, and new AI offerings.
The State of the Healthcare Industry in 2026
Health systems outline current performance, future plans
According to STAT, many health systems took a measured tone at this year’s conference, focusing largely on stability and consistency, especially in the face of significant Medicaid funding cuts from the One Big Beautiful Bill Act.
“For me, it’s been about stabilizing,” said Kevin Smith, CFO of SSM Health. “Taking a look at the operations, doing a lot of blocking and tackling. Getting back to the basics.”
Separately, Paul Rathbun, outgoing CFO at AdventHealth, said that “[i]t all begins and ends with consistent financial performance.” He also emphasized sustainability and the importance of a solid foundation to handle future uncertainty.
As hospitals and health systems face financial challenges, many are focusing on boosting efficiency and reducing expenses. For example, Intermountain Health is focusing on optimizing its supply chain and simplifying healthcare with value-based arrangements.
Some health systems, like CommonSpirit Health, are planning to sell some facilities to help boost finances and expand ambulatory networks. Providence is also considering selling some of its assets, potentially including some hospitals.
“We have 51 hospitals, most of which have No. 1 market share in their communities, but we do have a handful that we may have to find a different purpose or different sponsors for,” said Providence CFO Greg Hoffman.
Other health systems, like Mass General Brigham and Hackensack Meridian, are aiming to expand their partnerships with other providers or outside organizations. Currently, Mass General Brigham has a new ambulatory care venture with Tampa General Hospital, and Hackensack Meridian is planning to add 20 new primary care clinics in New Jersey with Amazon One Medical.
Top CMS officials meet with hospital, insurance leaders
At the conference, CMS Administrator Mehmet Oz, along with four top members of his staff, hosted an event with hundreds of top hospital and health insurance leaders to discuss the Trump administration’s healthcare policies.
During the event, Oz downplayed the potential impact of upcoming Medicaid cuts, saying that they won’t be felt for at least a year and a half. “The catastrophizing over the idea that it’s going to rip the guts out of the system, I don’t think that’s fair,” he said.
CMS leaders also discussed efforts to combat fraud, the Trump administration’s focus on deregulation, recent vaccine changes, and more.
“The catastrophizing over the idea that it’s going to rip the guts out of the system, I don’t think that’s fair.”
According to David Joyner, CEO of Hill Physicians Medical Group, the general mood among attendees was skeptical and pessimistic, particularly about cuts to Medicaid and the impact of declining Affordable Care Act membership. At the same time, people were curious and optimistic about CMS’ potential to promote new innovation and technology that could address some of the healthcare industry’s most persistent challenges.
AI offerings continue to expand
AI was a large focus of the conference, with many organizations announcing new tools or collaborations.
At the conference, Anthropic announced Claude for Healthcare, a new AI model that includes HIPAA-ready infrastructure for enterprise customers, native integration to commonly used medical and scientific databases, and a model specifically trained for healthcare and life sciences tasks.
The new model follows Claude for Life Sciences, which was launched last October. Anthropic also announced new capabilities for life sciences, which ranged from preclinical research and development and regulatory affairs.
According to Eric Kauderer-Abrams, head of biology and life sciences at Anthropic, healthcare and life sciences are one of the company’s largest bets.
“Anthropic is a very natural fit for the healthcare and life sciences world because our identity as an AI company is built around safety and responsibility and rigor and reproducibility, and these are all the central tenants of the healthcare and life sciences industries,” Kauderer-Abrams said.
Currently, several healthcare organizations already use Anthropic’s Claude model, including Banner Health, Novo Nordisk, and AbbVie. At the conference, Elation Health announced that it integrated Claude into its EHR to create chart summaries and clinical insights.
Other AI companies at the conference also announced new expansion efforts. For example, Hippocratic AI, which develops patient-facing generative AI healthcare agent, said it acquired Grove AI, a startup that provides agentic AI for pharma research and development and clinical trial operations. According to Hippocratic, the acquisition will help it build its life sciences division and accelerate the use of generative and agentic AI in the biopharma and med tech sectors.
Separately, Open Evidence said it plans to move toward “medical super-intelligence” by building its AI platform on top of a group of specialist medical AI models (oncology, neurology, radiology, etc.) instead of a single centralized model.
Pharma companies discuss new products, drug pricing deals
According to Johnson & Johnson (J&J) CEO Joaquin Duato, 2026 should be a better financial year for the company as it focuses on three high-growth areas for its med tech business: cardiovascular, surgery, and vision. Currently, J&J has around a dozen upcoming product launches across its med tech and innovative medicine businesses, including its new Ottava Robotic Surgical System.
Separately, BioNTech, which is most known for developing a COVID-19 vaccine with Pfizer, is turning its attention to cancer treatment. The company has an $11 billion partnership with Bristol Myers Squibb for its bispecific PDL1-VEGF antibody.
Pharmaceutical leaders also discussed the “most favored nation” (MFN) deals they signed with the Trump administration to reduce the prices of certain prescription drugs.
Paul Hudson, CEO of Sanofi, said that while it may sound like everyone won with these deals, there were compromises from both sides.
“I would say the government got what it needed, and we worked very hard to make sure that we could still deliver what we think is an attractive investment thesis for the company without breaking stride,” Hudson said. “So it was a very difficult needle to thread. I don’t want to give the impression that there’s no impact from MFN, because the question for us is: Can we manage that and deliver an attractive long-range plan?”
Christopher Boerner, CEO of Bristol Myers Squibb, had a similar view. “I think what we did with the agreement we signed at the end of last year is find a way to balance the interest of the administration in ‘most-favored nation’ with, obviously, what’s best for the company, but importantly, how can we find ways to provide real value to patients?”
The digital health market ramps up
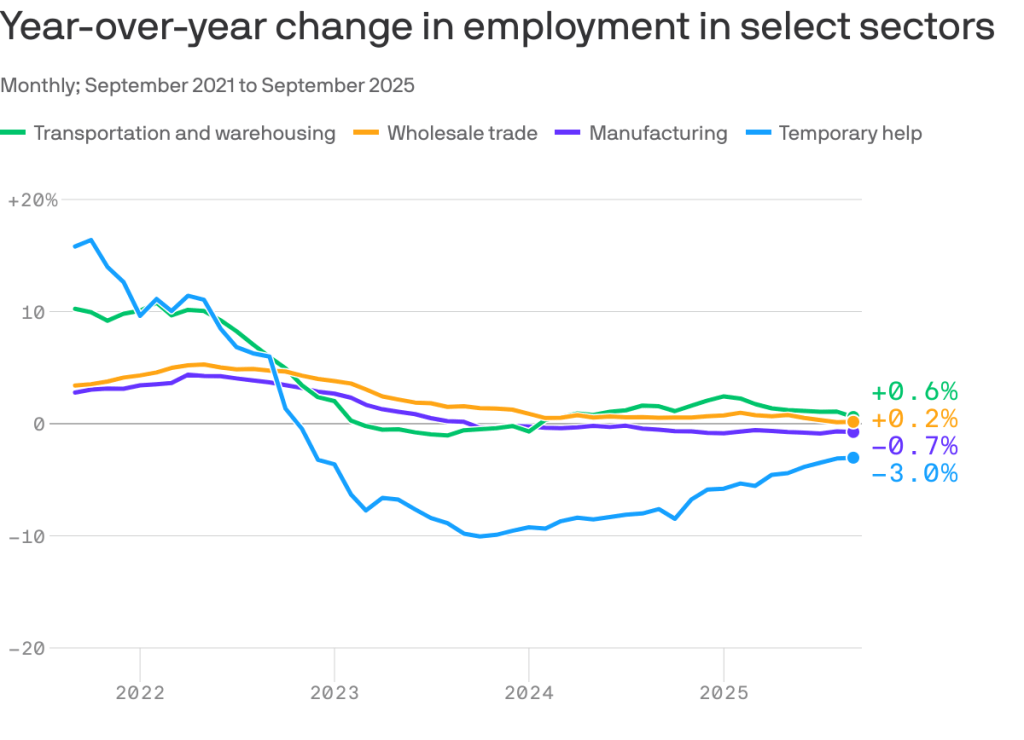
In 2025, digital health investments reached $14.2 billion in funding, a 35% increase from 2024 and the highest total since 2022. Last year, there were 26 megadeals, or those that raised over $100 million, and 15 new “unicorn” companies, or those valued at over $1 billion, up from just six in 2024.
Although the digital health market is still below its pandemic-era peak, there was significant growth in the market in 2025, largely driven by excitement around AI, according to analysts from Rock Health. The analysts also noted that there is a growing concentration of power in the digital health space, with certain companies having outsized influence.
“On one side, AI-native upstarts attracted huge rounds at unprecedented speed, a handful of companies broke the IPO drought, and private equity made major moves, signaling real bets on an emerging ‘winner’ class,” wrote Rock Health analysts Megan Zweig, Jacqueline Kimmell, and Maddie Knowles. However, on the other side, “… many companies are still grappling with valuation overhangs from prior cycles while operating in a more competitive market.”