After decades of “doctor knows best,” the traditional physician-patient relationship is on the verge of a monumental shift. Generative AI tools like OpenAI’s ChatGPT, Google’s Bard and Microsoft’s Bing are poised to give people significantly more power and control—not just over their personal lives and professional tasks, but over their own medical health, as well.
As these tools become exponentially smarter, safer and more reliable (an estimated 32 times more powerful in the next five years), everyday Americans will gain access to unparalleled medical expertise—doled out in easily understandable terms, at any time, from any place.
Already, Google’s Med-PaLM 2 has scored an expert-level 86.5% on the U.S. medical license exam while other AI tools have matched the skill and accuracy of average doctors in diagnosing complex medical diseases.
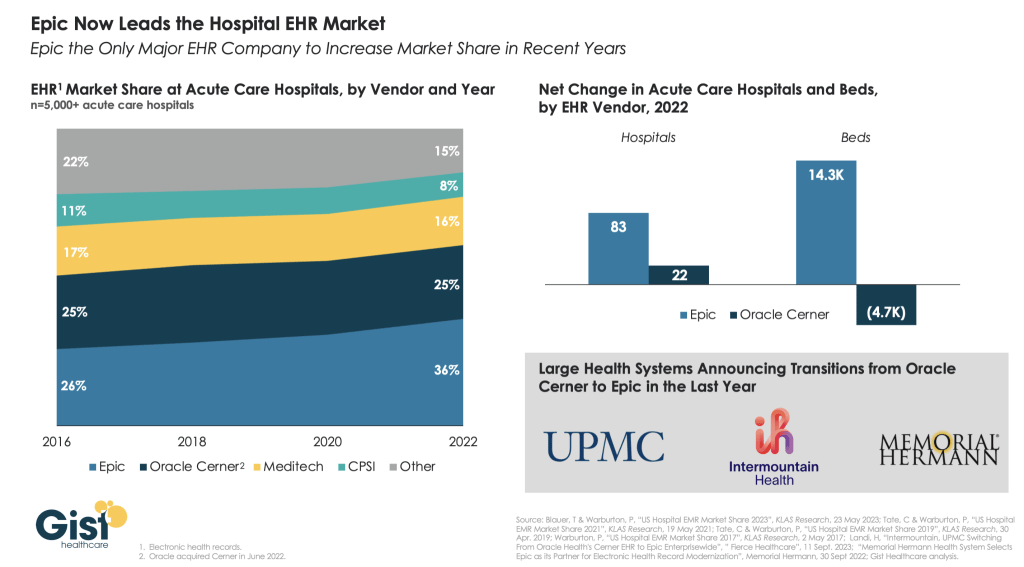
Soon, AI tools will be able to give patients detailed information about their specific medical problems by integrating with health monitors and electronic medical records (such EHR projects are already underway at Oracle/Cerner and Epic). In time, people will be able to self-diagnose and manage their own diseases as accurately and competently as today’s clinicians.
This newfound expertise will shake the very foundation of clinical practice.
Although public health experts have long touted the concept of clinicians and patients working together through shared decision-making, this rarely happens in practice. Generative AI will alter that reality.
Building on part one of this article, which explained why generative AI constitutes a quantum leap ahead of all the tech that came before it, part two provides a blueprint for strengthening the doctor-patient alliance in the era of generative AI.
Patients Today: Sick And Confused
To understand how generative AI will impact the practice of medicine, it’s best to look closer at the current doctor-patient dynamic.
The relationship has undergone significant evolution. In the past century, patients and doctors held close, enduring relationships, built on trust and a deep understanding of the patient’s individual needs. These bonds were characterized by a strong sense of personal connection, as doctors had the time to listen to their patients’ concerns and provided not only medical treatment but also emotional support.
Today, the doctor-patient relationship remains vitally important, but it has undergone several meaningful changes. While medical advancements have greatly expanded the possibilities for diagnosis and treatment, the relationship itself has suffered from less trust and a more transactional focus. The average visit lasts just 15 minutes, barely enough time to address the patient’s current medical concerns. The doctor’s computer and electronic healthcare record systems sit, quite literally, between doctors and patients. The result is that patients feel rushed and find their medical care increasingly impersonal. Modern healthcare is characterized by time constraints, administrative burdens and a focus on efficiency. This can lead to a sense of impersonality and decreased communication between doctors and patients.
But throughout these changes, one thing has remained constant. The doctor-patient relationship, which dates back more than five millennia, has always existed on an uneven playing field, with patients forced to rely almost entirely on doctors to understand their diseases and what to do about them.
Though patients can and do access the internet for a list of possible diagnoses and treatment options, that’s not the same as possessing medical expertise. In fact, sorting through dozens of online sources—often with conflicting, inaccurate, outdated and self-serving information—proves more confusing than clarifying. Nowhere can web-surfers find personalized and credible advice based on their age, medical history, genetic makeup, current medications and laboratory results.
What’s needed now is modern doctor-patient relationship, one that is strong enough to meet the demands of medicine today and restore the vital, personal and emotional connections of the past.
Patients Tomorrow: Self-Diagnosing And Confident
In the future, generative AI will alter the doctor-patient dynamic by leveling the playing field.
Already, consumer AI tools can equip users with not just knowledge, but expertise. They allow the average person to create artistic masterpieces, produce hit songs and write code with unimagined sophistication. Next generations will offer a similar ability for patients, even those without a background in science or medicine.
Like a digitized second opinion, generative AI will shrink the knowledge gap between doctors and patients in ways that search engines can’t. By accessing millions of medical texts, peer-reviewed journals and scientific articles, ChatGPT will deliver accurate and unbiased medical expertise in layman’s language. And unlike internet sources, generative AI tools don’t have built-in financial incentives or advertising models that might skew responses.
To help patients and doctors navigate the upcoming era of generative AI, here’s a model for the future of medical practice based on proven approaches in education:
Introducing The ‘Flipped Healthcare’ Model
The “flipped classroom” can be traced back nearly four decades, but it became popularized in the United States in the early 2000s through the Khan Academy in Northern California.
Students begin the learning process by watching videos and engaging with interactive tools online rather than sitting through traditional lectures. This pre-class preparation (or “homework in advance”) allows people to learn at their own pace. Moreover, it enhances classroom discussions, letting teachers and students dive much deeper into topics than they ever could before. Indeed, students spend time in class applying knowledge and collaborating to solve problems—not merely listening and taking notes.
The introduction of generative AI opens the door to a similar approach in healthcare. Here’s how that might work in practice:
- Pre-Consultation Learning: Before visiting a doctor, patients would use generative AI tools to understand their symptoms or medical conditions. This foundational knowledge would accelerate the diagnostic process and enhance patient understanding. Even in the absence of advanced diagnostic testing (X-rays or bloodwork), this pre-consultation phase allows the patient to understand the questions their clinicians will ask and the steps they will take.
- In-Depth Human Interactions: With the patient’s knowledge base already established, consultations will dive deep into proactive health strategies and/or long-term chronic-disease management solutions, rather than having to start at square one. This approach maximizes the time patients and clinicians spend together. It also addresses the reality that at least 50% of patients leave the doctor’s office unsure of what they’ve been told.
- Home Monitoring: For the 60% of American patients living with chronic diseases, generative AI combined with wearable monitors will provide real-time feedback, thereby optimizing clinical outcomes. These patients, instead of going in for periodic visits (every three to six months), will obtain daily medical analysis and insights. And in cases where generative AI spots trouble (e.g., health data deviates from the doctor’s expectations), the provider will be able to update medications immediately. And when the patient is doing well, physicians can cancel follow-up visits, eliminating wasted time for all.
- Hospital At Home: Inpatient (hospital) care accounts for 30% of all healthcare costs. By continuously monitoring patients with medical problems like mild pneumonia and controllable bacterial infections, generative AI (combined with home monitoring devices and telemedicine access) would allow individuals to be treated in the comfort of their home, safely and more affordably than today.
- Lifestyle Medicine: Generative AI would support preventive health measures and lifestyle changes, reducing the overall demand for in-person clinical care. Studies confirm that focusing on diet, exercise and recommended screenings can reduce the deadliest complications of chronic disease (heart attack, stroke, cancer) by 30% or more. Decreasing the need for intensive procedures is the best way to make healthcare affordable and address the projected shortage of doctors and nurses in the future.
The Future: Collaborative Care For Superior Outcomes
The U.S. healthcare model often leaves patients feeling frustrated and overwhelmed. Meanwhile, time constraints placed on doctors lead to rushed consultations and misdiagnoses, which cause an estimated 800,000 deaths and disabilities annually.
The “flipped” approach, inspired by the Khan Academy, leverages the patient expertise that generative AI will create. Following this model will free up clinician time to make the most of every visit. Implementing this blueprint will require improvements in AI technology and an evolution of medical culture, but it offers the opportunity to make the doctor-patient relationship more collaborative and create empowered patients who will improve their health.
Talk with educators at the Khan Academy, and they will tell you how their innovative model results in better-educated students. They’ll also tell you how much more satisfied teachers and students are compared to those working in the traditional educational system. The same can be true for American medicine.