The COVID-19 pandemic is rife with scientific and medical uncertainty, including debates about the ethics of using experimental treatments.
The big picture: As the global pandemic continues, the tension between providing the best available care for patients and performing trials to determine whether that care is effective risks complicating the medical response.
The big question: Is it unethical to withhold a possible treatment from someone who instead receives a placebo, or to continue to administer that treatment without having collected data on whether it works?
Driving the news: President Trump received an experimental monoclonal antibody cocktail via expanded access or “compassionate use,” which allows someone to access a treatment outside of a clinical trial before it is approved, provided their doctor, the drug company and the FDA agree.
- Experts say his subsequent claims of the treatment being a cure risks reducing enrollment in clinical trials, flooding companies with requests for access to a limited number of doses and creating false hope for patients.
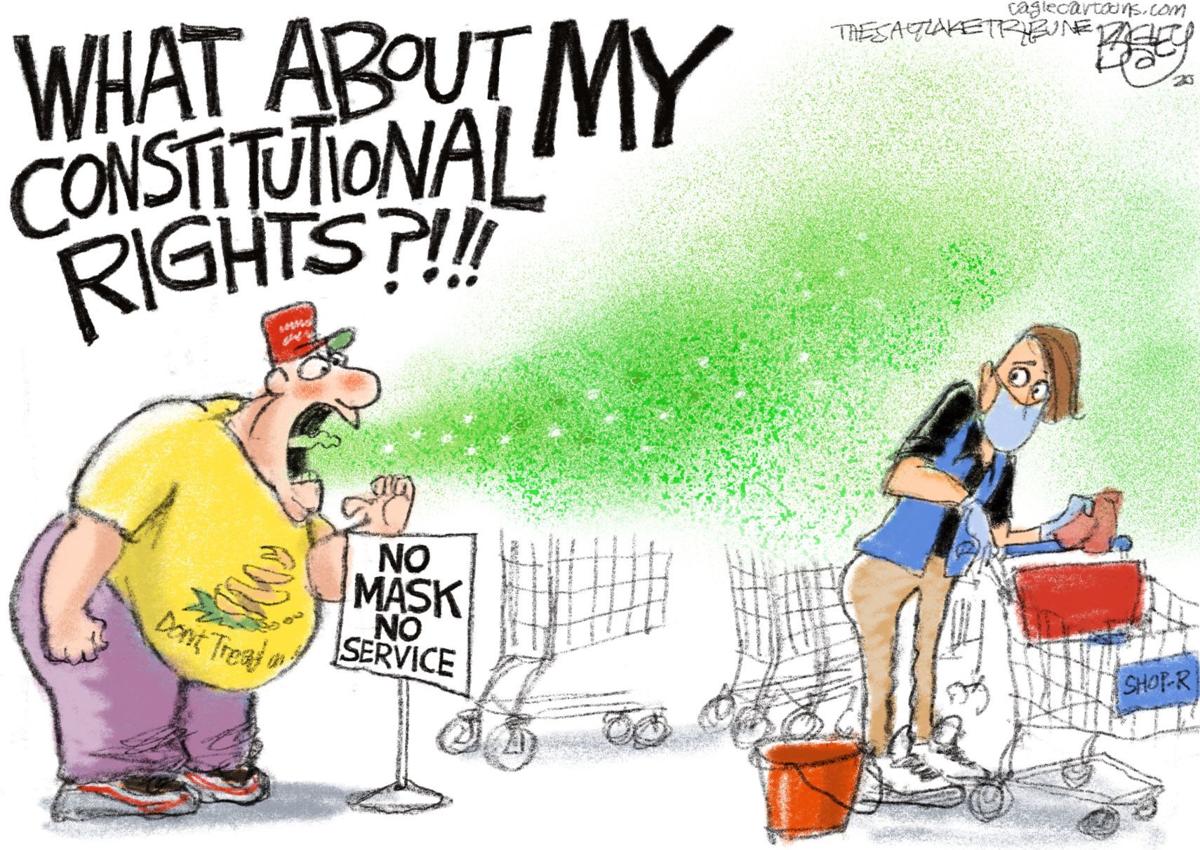
- And the president’s treatment raised questions about fairness — would other COVID-19 patients have similar access?
- “It’s important that we not say the president got access to a beneficial experimental intervention because we don’t know if it is beneficial or if there are adverse events associated with it,“ says Alex John London, director of the Center for Ethics and Policy at Carnegie Mellon University.
He and other ethicists say the president’s treatment highlights a broader question about the ethical obligation doctors have to the science needed to determine if those treatments are effective.
Between the lines: Offering patients experimental COVID-19 drugs via emergency use authorizations, expanded access programs and compassionate use can slow needed clinical trials.
- Researchers have struggled to enroll people in clinical trials in which they may receive a placebo if patients can access a drug directly.
- One example: “There’s been some hiccups with the expanded access use for convalescent plasma, because it was something that precluded people from enrolling in a randomized control trial, so it took longer, and we still don’t quite know how well convalescent plasma works,” says Amesh Adalja, an infectious disease physician and senior scholar at the Johns Hopkins Center for Health Security.
More than 100,000 COVID-19 patients at almost 2,800 U.S. hospitals received convalescent plasma from people who survived the virus and developed antibodies to it.
- “It’s easy for people to say you enrolled 100,000 people, there should have been a trial. But a small number of those 2,800 hospitals would have been capable of doing those trials,” says the Mayo Clinic’s Michael Joyner, who leads the program.
- There are now smaller trials taking place to answer questions about the effectiveness of plasma in treating the disease in different stages.
- But if this happens again, Joyner says programs at academic medical centers should be peeled off earlier to form clinical trials run in parallel.
The gold standard for determining whether a treatment works is through randomized controlled trials in which people are randomly assigned to receive a treatment or to be in a control group.
- In the uncertainty and urgency of a pandemic, some physicians argue randomizing people to receive a placebo goes against physicians’ ethics and that it is better to do something to help patients than do nothing.
- “That’s a false dichotomy because the question is, what should we do?” says London.
From a doctor’s perspective, it’s important to weigh the collective value of theearly drug data and the individual needs of the patient, Adalja says.
- “I do think you have to be extra careful when you’re thinking about drugs that you don’t have strong randomized control trial data for, or the data is incomplete or inconclusive,” he adds.
- “What people have to ask themselves is what constitutes evidence or proof and where do you want to make the bets in a pandemic?” says Joyner.
- “There is a moral, legal and public health obligation to do those trials before people use those products,” says Alison Bateman-House, a professor of medical ethics at NYU’s Grossman School of Medicine who co-chairs an international working group on pre-approval access to treatments.
- She says she understands the emotional pull on doctors to help patients whose health is quickly deteriorating, “but it is not evidence-based medicine.”
“There is no ethical obligation to give anyone an unproven substance.”
— Alison Bateman-House, NYU Grossman School of Medicine
In a forthcoming paper, London argues that when medical professionals don’t have the knowledge they need to treat patients, it is their responsibility “to band together and run studies to get evidence to discharge [their] very ancient medical obligation.”
- Medical ethics should be updated to include a responsibility to learn in the face of uncertainty, says London, who was part of a committee that called for research to be incorporated into the response to the Ebola outbreak in West Africa in 2014.
- The U.K.’s large randomized RECOVERY trial is based in part on the Ebola experience, says London. “Because of it, we know dexamethasone is effective and hydroxychloroquine is not.”
What to watch: How the FDA’s handling of treatments during the pandemic influences other drugs and diseases once the pandemic ends.
The bottom line: “Medicine doesn’t have a good handle on uncertainty, and that is a problem,” says London.