Twenty-five percent of the 1,430 rural hospitals in the U.S. are at high risk of closing unless their finances improve, according to an annual analysis from Guidehouse, a consulting firm.
The 354 rural hospitals at high risk of closing are spread across 40 states and represent more than 222,000 annual discharges. According to the analysis, 287 of these hospitals — 81 percent — are considered highly essential to the health and economic wellbeing of their communities.
Several factors are putting rural hospitals at risk of closing, according to the analysis, which looked at operating margin, days cash on hand, debt-to-capitalization ratio, current ratio and inpatient census to determine the financial viability of rural hospitals. Declining inpatient volume, clinician shortages, payer mix degradation and revenue cycle management challenges are among the factors driving the rural hospital crisis.
The Guidehouse study analyzed the financial viability of rural hospitals prior to the COVID-19 pandemic, and the authors noted that the rural hospital crisis could significantly worsen due to the pandemic or any downturn in the economy.
Here are the number and percentage of rural hospitals at high risk of closing in each state based on the analysis:
Tennessee
Rural hospitals at high risk of closing: 19 (68 percent)
Alabama
Rural hospitals at high risk of closing: 18 (60 percent)
Oklahoma
Rural hospitals at high risk of closing: 28 (60 percent)
Arkansas
Rural hospitals at high risk of closing: 18 (53 percent)
Mississippi
Rural hospitals at high risk of closing: 25 (50 percent)
West Virginia
Rural hospitals at high risk of closing: 9 (50 percent)
South Carolina
Rural hospitals at high risk of closing: 4 (44 percent)
Georgia
Rural hospitals at high risk of closing: 14 (41 percent)
Kentucky
Rural hospitals at high risk of closing: 18 (40 percent)
Louisiana
Rural hospitals at high risk of closing: 11 (37 percent)
Maine
Rural hospitals at high risk of closing: 7 (33 percent)
Indiana
Rural hospitals at high risk of closing: 8 (31 percent)
Kansas
Rural hospitals at high risk of closing: 26 (31 percent)
New Mexico
Rural hospitals at high risk of closing: 3 (30 percent)
Michigan
Rural hospitals at high risk of closing: 13 (29 percent)
Missouri
Rural hospitals at high risk of closing: 10 (26 percent)
Virginia
Rural hospitals at high risk of closing: 5 (25 percent)
Oregon
Rural hospitals at high risk of closing: 4 (24 percent)
California
Rural hospitals at high risk of closing: 6 (23 percent)
North Carolina
Rural hospitals at high risk of closing: 6 (23 percent)
Florida
Rural hospitals at high risk of closing: 2 (22 percent)
North Dakota
Rural hospitals at high risk of closing: 7 (21 percent)
Ohio
Rural hospitals at high risk of closing: 6 (20 percent)
Vermont
Rural hospitals at high risk of closing: 2 (20 percent)
Idaho
Rural hospitals at high risk of closing: 4 (19 percent)
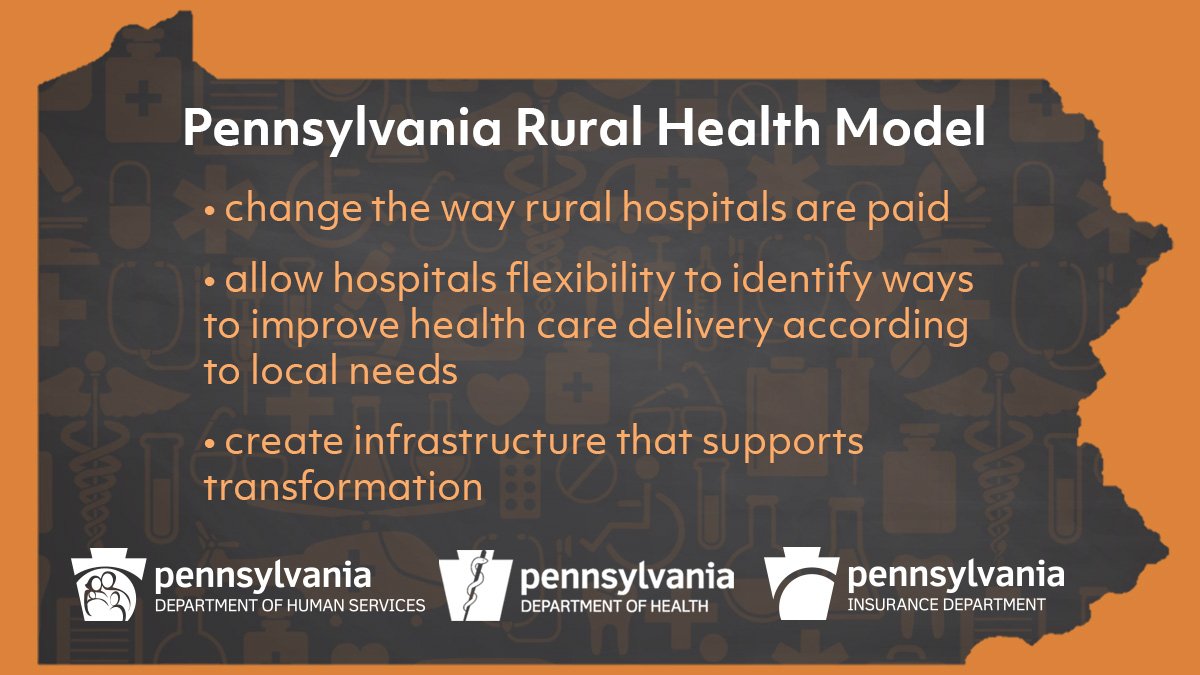
Pennsylvania
Rural hospitals at high risk of closing: 4 (19 percent)
Washington
Rural hospitals at high risk of closing: 5 (18 percent)
Wyoming
Rural hospitals at high risk of closing: 3 (18 percent)
Texas
Rural hospitals at high risk of closing: 14 (16 percent)
Colorado
Rural hospitals at high risk of closing: 4 (14 percent)
Illinois
Rural hospitals at high risk of closing: 7 (14 percent)
Montana
Rural hospitals at high risk of closing: 7 (14 percent)
Nebraska
Rural hospitals at high risk of closing: 8 (13 percent)
New York
Rural hospitals at high risk of closing: 4 (13 percent)
Iowa
Rural hospitals at high risk of closing: 9 (12 percent)
Minnesota
Rural hospitals at high risk of closing: 8 (11 percent)
Alaska
Rural hospitals at high risk of closing: 1 (10 percent)
Arizona
Rural hospitals at high risk of closing: 1 (10 percent)
New Hampshire
Rural hospitals at high risk of closing: 1 (9 percent)
Wisconsin
Rural hospitals at high risk of closing: 5 (9 percent)