This approach combines the payment standard with arbitration to resolve disputes. An insurer pays a set amount, and if the provider disagrees, it can initiate arbitration.
State Laws
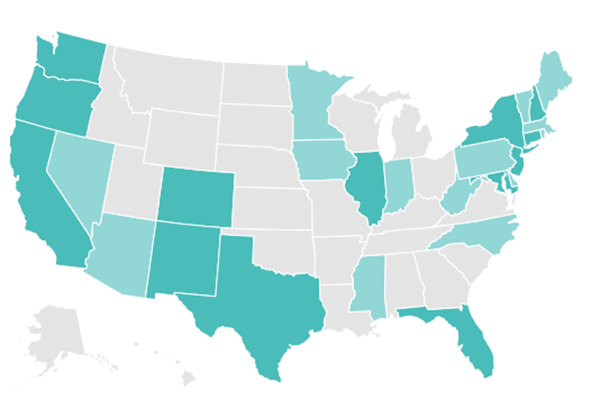
With federal solutions at a standstill, 30 states have passed varying levels of protections from surprise billing. As of July, 2020, 16 states have more comprehensive protections, which ensure that insured patients are only responsible for paying in-network costs, even when receiving care from out-of-network providers or emergency services at an out-of-network facility. Georgia was the latest state to pass such a law in July 2020. The other 14 states offer far more limited protections.
But even states with comprehensive protections cannot protect all patients from surprise medical bills. States are not able to regulate job-based coverage that falls under a federal law known as the Employee Retirement Income Security Act, which applies to most employer sponsored insurance. These patients remain vulnerable to surprise medical bills until Congress takes action to ban the practice.
Click on the map below for an interactive map from the Commonwealth Fund that details each state’s protections.
The Sticking Point: Will Congress Pass Protections?
Despite strong bipartisan support for protecting patients from surprise bills, disagreement comes over how much physician groups should charge and how much insurers should pay. Essentially, resolving this issue may mean Congress has to pick sides.
As a result, stakeholders such as hospitals and private equity-backed physician groups, in particular, have pushed back on federal legislation, arguing that banning surprise billing will cripple their bottom line. These equity-backed physician groups have powerful lobbying groups, and in 2019, spent at least $5 million to persuade lawmakers to halt the legislation.
The pandemic has increased the risk that patients will unknowingly receive care from an out-of-network provider or at an out-of-network facility. The Trump administration tried to limit surprise bills for those in need of COVID-19 treatment by banning hospitals and providers that receive money from its Provider Relief Fund from sending balance bills to patients. But this approach leaves significant gaps and has had mixed success.