Hospitals’ reliance on travel workers is nothing new. The pandemic intensified it and highlighted the gap between full-time workers’ pay and lucrative temporary contracts.
While the average salary for a travel nurse can vary based on location, regional demand, hospital type and specialty, the compensation for a travel nurse has increased significantly compared to pre-pandemic, Bill Morgan, president of the Orlando, Fla.-based travel nurse staffing firm Jackson Nurse Professionals, told Becker’s in September.
Meanwhile, hospitals and health systems have offered bonuses, increased wages and made other investments in employee retention for their staff workers. Still, the compensation gap between hospital employed nurses and travel or agency nurses remains stark.
The gap poses the seemingly simple question: Why aren’t hospitals paying full-time staff more instead of paying higher prices for travel workers?
Travel nursing’s start
Taking a look back at the history of why hospitals started using travel nurses in the first place helps answer that question, said Kathy Sanford, DBA, RN, chief nursing officer at Chicago-based CommonSpirit Health.
Dr. Sanford recalls first using local agencies and travel nurses in the 1980s as a cost-effective staffing strategy for periods when the patient census fluctuates, such as during flu epidemics.
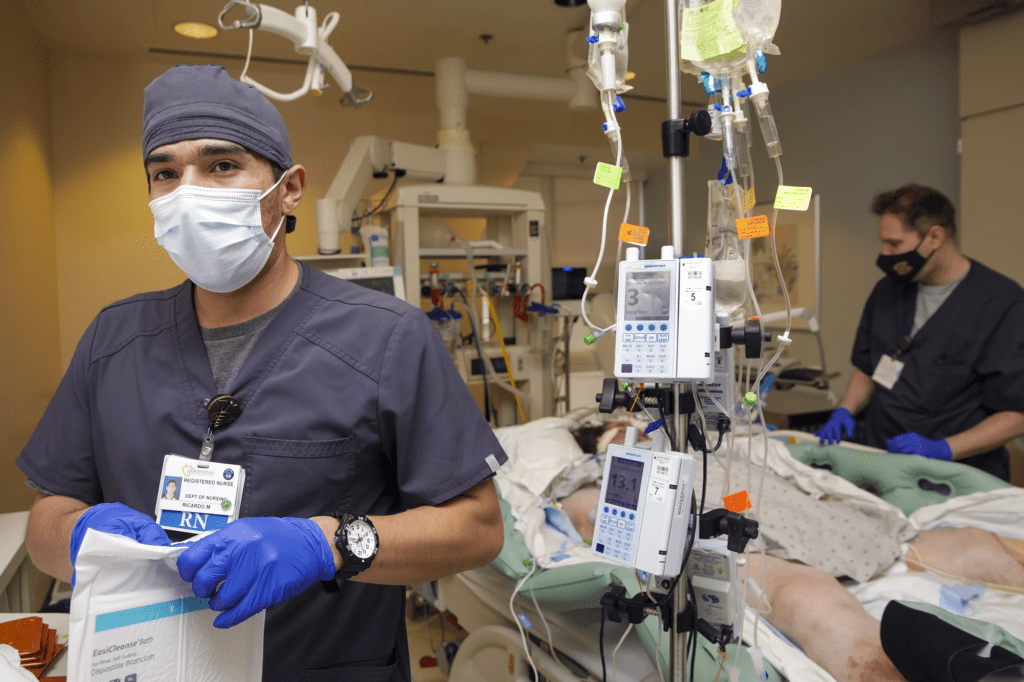
“When you have those fluctuations, you need to have a staffing strategy of what you want to do when the census goes up higher than we are staffed for, but it’s only going to last maybe a month, or a little longer,” she told Becker’s. “Because of the fluctuations, our nursing strategy for staffing was to use these non-employed nurses to fill in when there were gaps.”
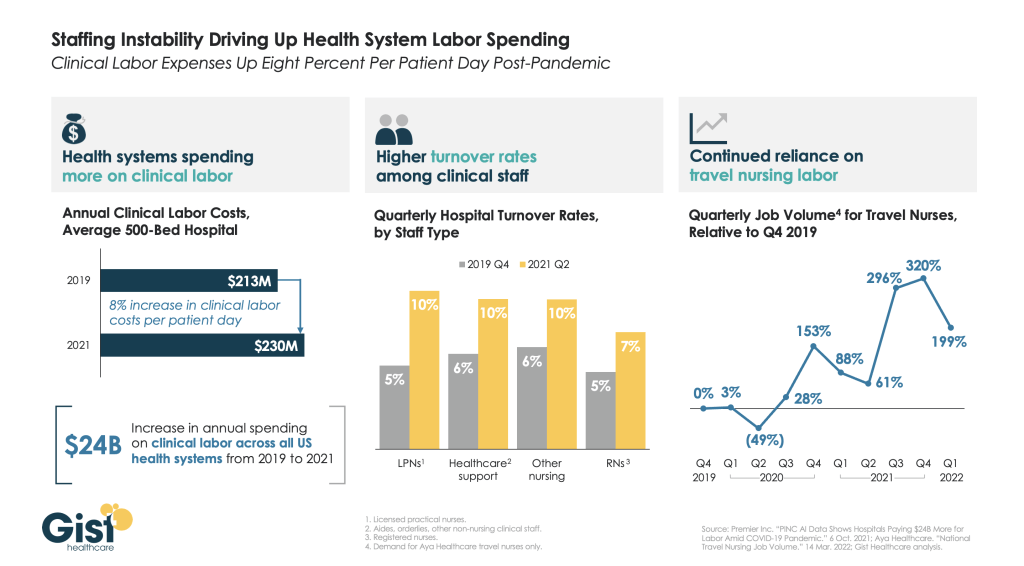
The COVID-19 pandemic, however, has created a situation where volumes are consistently higher than normal. And while rates for a travel or agency nurse have traditionally been higher than those of a hospital staff nurse, the current demand has pushed travel rates to record highs.
Rising rates
Pittsburgh-based UPMC, for example, paid an estimated $85 an hour for a traveling nurse or a nurse from an agency before the pandemic. The health system is now experiencing rates between $225 and $250 an hour. Such rates have made nurses who may not have considered traveling before take the leap.
“And the nurses are making more, and we don’t fault the nurses for taking advantage of that opportunity. But … now not only are nurses making more, but the agencies have taken the opportunity to triple their profits … and it shouldn’t be permitted during a pandemic, just like we don’t permit building companies to triple the price of lumber after a hurricane. It just shouldn’t be allowed,” said John Galley, chief human resource officer at UPMC.
“Hospitals are all trying to fill the positions that need to be filled to help us get through this crisis with travel nurses, but because there aren’t enough, it becomes a cycle of bidding of who will pay me the most to travel,” Dr. Sanford said. Because of that, many nurses who may have never considered traveling before are now choosing to do so and leaving hospitals in areas of the country with a lower wage index, she said.
Pay for travel nurses has always been higher for the same reasons hospitals pay float pool nurses more, Dr. Sanford explained.
“Nurses are specialists and they work on a particular type of unit, and sometimes one unit’s census will be down and another unit’s census will be up,” she said. Float pool nurses are willing to shift to different units that need help “and it’s not a favorite thing for nurses to do,” Dr. Sanford said. “You have to pay them a little extra to be willing to learn different types of nursing and be willing to float.”
The same line of thinking applies to agency or travel nurses. Travelers don’t have the perks that come with a full-time job, like job security and benefits. That coupled with the burden of travel itself and short-term assignments was the initial justification for why travel nurses had higher rates.
Simply put, hospitals can’t afford to pay full-time staff wages that were meant for temporary assignments.
“The bottom line is it would not be sustainable for hospitals to pay the kind of dollars that they’re paying right now for travel nurses in the long run. Because nurses are our backbone … they’re our heart, but they’re also our backbone. They’re the majority of our staff.” Dr. Sanford said.
Mr. Galley of UPMC echoed that sentiment, noting that salaries and benefits make up about 50 percent of a health system’s entire expenses. “If you were to double a good portion of that — the nursing salaries — you’d completely wipe out any operating margin. Then you wouldn’t be able to invest in anything to keep the hospitals going,” he said.
And healthcare has a lot of costly demands that would go unaddressed if such rates became the expectation for staff nurses.
“There are a lot of needs that healthcare has in technology, and making sure that we have the equipment to take care of patients, and that we can do programs for the poor and vulnerable that we wouldn’t be able to afford if we pay these non-sustainable prices forever,” Dr. Sanford of CommonSpirit said.
The value of in-house agencies
To combat skyrocketing travel nursing costs, some health systems have introduced their own travel agencies, including CommonSpirit and UPMC, where travel nurses work within the system.
Mr. Galley said UPMC started the agency for its 40-hospital system not only to combat the nursing shortage — and attract back nurses the health system has lost to outside travel agencies — but also to address increased rates from outside travel agencies.
Nurses and surgical techs who qualify for UPMC’s in-house agency will earn $85 an hour and $63 an hour, respectively, in addition to a $2,880 stipend at the beginning of each six-week assignment.
Compensation for travel nurses at UPMC is still higher than full-time employees because the job comes with its own set of challenges. While full-time nurses get to know their facilities and have a more regular schedule, travel nurses are constantly on the move.
“They’re going to have assignments for a few weeks at a time at a particular location, then we’re going to pick them up and move them somewhere else, so they’re going to be constantly traveling, living out of a suitcase, and that’s what external travelers do, so we want to be just like the market, create roles like that and pay like that,” Mr. Galley said. “I think our employees understand the difference between that kind of a lifestyle that goes along with the higher salary.”
CommonSpirit’s internal agency plans to start traveling in the early spring and is in the process of hiring a national director for the program. The system’s goal is to have 500 nurses.
Dr. Sanford said the program will be beneficial because it will bring down competition, and people who want to travel can still be employees within the health system.
“It gives nurses who are our employees a choice if they want to be travelers or if they want to do it part time and then come back to a job within one of our hospitals or in one of our clinics. … They won’t lose their benefits, they won’t lose their seniority. They’ll be our employees,” Dr. Sanford said.
Other systems are exploring similar programs, such as Charlotte, N.C.-based Atrium Health, which recently ran a pilot in-house traveler program. The health system has also used outside agencies, which cost about triple compared to pre-pandemic.
“This program was very successful, less expensive than using an external travel agency and worked really well across our large health system that covers multiple states,” said Patricia Mook, MSN, RN, vice president of nursing operations at Atrium Health.
But internal travel programs may not be easy for other health systems to mimic, especially smaller ones. Hospitals have to be of a certain size for an internal travel program to work, meaning an individual hospital wouldn’t be able to have one, Mr. Galley said.
More than that, it’s a complex undertaking, he said.
“It’s not without its challenges,” Mr. Galley said. “I just think it’s something that takes the resources and thought leadership to be able to do. But you’re not going to find independent hospitals being able to mirror this.”
Dr. Sanford also recommends having a few different strategies in place to combat nurse shortages.
“Don’t make it your only strategy because there are so many issues that we could do better with our nursing staff. … You need to be looking at all of the different things that give nurses voice in your organization,” Dr. Sanford said.