I have been both a frontline officer and a staff officer at
a health system. I started a solo practice in 1977 and
cared for my rheumatology, internal medicine and
geriatrics patients in inpatient and outpatient settings.
After 23 years in my solo practice, I served 18 years as
President and CEO of a profitable, CMS 5-star, 715-bed,
two-hospital healthcare system.
From 2015 to 2020, our health system team added
0.6 years of healthy life expectancy for 400,000 folks
across the socioeconomic spectrum. We simultaneously
decreased healthcare costs 54% for 6,000 colleagues and
family members. With our mentoring, four other large,
self-insured organizations enjoyed similar measurable
results. We wanted to put our healthcare system out of
business. Who wants to spend a night in a hospital?
During the frontline part of my career, I had the privilege
of “Being in the Room Where It Happens,” be it the
examination room at the start of a patient encounter, or
at the end of life providing comfort and consoling family.
Subsequently, I sat at the head of the table, responsible for
most of the hospital care in Southwest Florida. [1]
Many folks commenting on healthcare have never touched
a patient nor led a large system. Outside consultants, no
matter how competent, have vicarious experience that
creates a different perspective.
At this point in my career, I have the luxury of promoting
what I believe is in the best interests of patients —
prevention and quality outcomes. Keeping folks healthy and
changing the healthcare industry’s focus from a “repair shop”
mentality to a “prevention program” will save the industry
and country from bankruptcy. Avoiding well-meaning but
inadvertent suboptimal care by restructuring healthcare
delivery avoids misery and saves lives.
RESPONDING TO AN ATTACK
Preemptive reinvention is much wiser than responding to an
attack. Unfortunately, few industries embrace prevention. The
entire healthcare industry, including health systems, physicians,
non-physician caregivers, device manufacturers, pharmaceutical
firms, and medical insurers, is stressed because most are
experiencing serious profit margin squeeze. Simultaneously
the public has ongoing concerns about healthcare costs. While
some medical insurance companies enjoyed lavish profits during
COVID, most of the industry suffered. Examples abound, and
Paul Keckley, considered a dean among long-time observers of
the medical field, recently highlighted some striking year-end
observations for 2022. [2]
Recent Siege Examples
Transparency is generally good but can and has led to tarnishing
the noble profession of caring for others. Namely, once a
sector starts bleeding, others come along, exacerbating the
exsanguination. Current literature is full of unflattering public
articles that seem to self-perpetuate, and I’ve highlighted
standout samples below.
- The Federal Government is the largest spender in the
healthcare industry and therefore the most influential. Not
surprisingly, congressional lobbying was intense during
the last two weeks of 2022 in a partially successful effort
to ameliorate spending cuts for Medicare payments for
physicians and hospitals. Lobbying spend by Big Pharma,
Blue Cross/Blue Shield, American Hospital Association, and
American Medical Association are all in the top ten spenders
again. [3, 4, 5] These organizations aren’t lobbying for
prevention, they’re lobbying to keep the status quo. - Concern about consistent quality should always be top of
mind. “Diagnostic Errors in the Emergency Department: A
Systematic Review,” shared by the Agency for Healthcare
Research and Quality, compiled 279 studies showing a
nearly 6% error rate for the 130 million people who visit
an ED yearly. Stroke, heart attack, aortic aneurysm, spinal
cord injury, and venous thromboembolism were the most
common harms. The defense of diagnostic errors in emergency
situations is deemed of secondary importance to stabilizing
the patient for subsequent diagnosing. Keeping patients alive
trumps everything. Commonly, patient ED presentations are
not clear-cut with both false positive and negative findings.
Retrospectively, what was obscure can become obvious. [6, 7] - Spending mirrors motivations. The Wall Street Journal article
“Many Hospitals Get Big Drug Discounts. That Doesn’t Mean
Markdowns for Patients” lays out how the savings from a
decades-old federal program that offers big drug discounts
to hospitals generally stay with the hospitals. Hospitals can
chose to sell the prescriptions to patients and their insurers for much more than the discounted price. Originally the legislation was designed for resource-challenged communities, but now some hospitals in these programs are profiting from wealthy folks paying normal prices and the hospitals keeping the difference. [8] - “Hundreds of Hospitals Sue Patients or Threaten Their Credit,
a KHN Investigation Finds. Does Yours?” Medical debt is a
large and growing problem for both patients and providers.
Healthcare systems employ collection agencies that
typically assess and screen a patient’s ability to pay. If the
credit agency determines a patient has resources and has
avoided paying his/her debt, the health system send those
bills to a collection agency. Most often legitimately
impoverished folks are left alone, but about two-thirds
of patients who could pay but lack adequate medical
insurance face lawsuits and other legal actions attempting
to collect payment including garnishing wages or placing
liens on property. [9] - “Hospital Monopolies Are Destroying Health Care Value,”
written by Rep. Victoria Spartz (R-Ind.) in The Hill, includes
a statement attributed to Adam Smith’s The Wealth of
Nations, “that the law which facilitates consolidation ends in
a conspiracy against the public to raise prices.” The country
has seen over 1,500 hospital mergers in the past twenty
years — an example of horizontal consolidation. Hospitals
also consolidate vertically by acquiring physician practices.
As of January 2022, 74 percent of physicians work directly for
hospitals, healthcare systems, other physicians, or corporate
entities, causing not only the loss of independent physicians
but also tighter control of pricing and financial issues. [10]
The healthcare industry is an attractive target to examine.
Everyone has had meaningful healthcare experiences, many have
had expensive and impactful experiences. Although patients do
not typically understand the complexity of providing a diagnosis,
treatment, and prognosis, the care receiver may compare the
experience to less-complex interactions outside healthcare that
are customer centric and more satisfying.
PROFIT-MARGIN SQUEEZE
Both nonprofit and for-profit hospitals must publish financial
statements. Three major bond rating agencies (Fitch Ratings,
Moody’s Investors Service, and S & P Global Ratings) and
other respected observers like KaufmanHall, collate, review,
and analyze this publicly available information and rate health
systems’ financial stability.
One measure of healthcare system’s financial strength is
operating margin, the amount of profit or loss from caring
for patients. In January of 2023 the median, or middle value,
of hospital operating margin index was -1.0%, which is an
improvement from January 2022 but still lags 2021 and 2020.
Erik Swanson, SVP at KaufmanHall, says 2022,
“Is shaping up to be one of the worst financial years on
record for hospitals. Expense pressures — particularly
with the cost of labor — outpaced revenues and drove
poor performance. While emergency department visits
and operating room minutes increased slightly, hospitals
struggled to discharge patients due to internal staffing
shortages and shortages at post-acute facilities,” [11]
Another force exacerbating health system finance is the
competent, if relatively new retailers (CVS, Walmart, Walgreens,
and others) that provide routine outpatient care affordably.
Ninety percent of Americans live within ten miles of a Walmart
and 50% visit weekly. CVS and Walgreens enjoy similar
penetration. Profit-margin squeeze, combined with new
convenient options to obtain routine care locally, will continue
disrupting legacy healthcare systems.
Providers generate profits when patients access care.
Additionally, “easy” profitable outpatient care can and has
switched to telemedicine. Kaiser-Permanente (KP), even before
the pandemic, provided about 50% of the system’s care through
virtual visits. Insurance companies profit when services are
provided efficiently or when members don’t use services.
KP has the enviable position of being both the provider
and payor for their members. The balance between KP’s
insurance company and provider company favors efficient
use of limited resources. Since COVID, 80% of all KP’s visits are
virtual, a fact that decreases overhead, resulting in improved
profit margins. [12]
On the other hand, KP does feel the profit-margin squeeze
because labor costs have risen. To avoid a nurse labor strike,
KP gave 21,000 nurses and nurse practitioners a 22.5% raise over
four years. KP’s most recent quarter reported a net loss of $1.5B,
possibly due to increased overhead. [13]
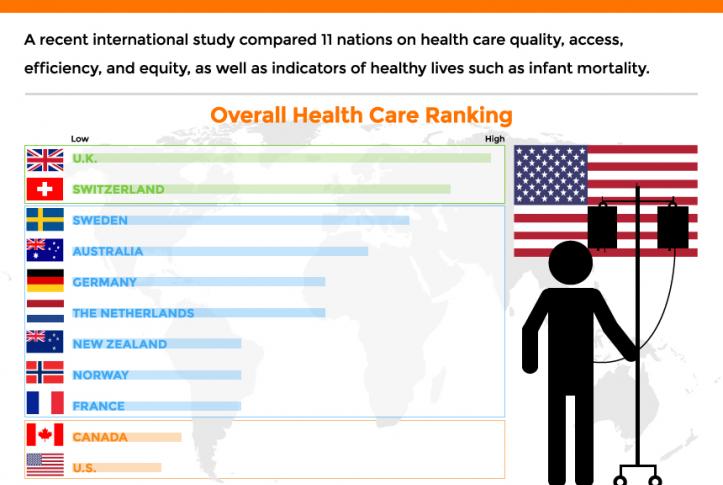
The public, governmental agencies, and some healthcare leaders
are searching for a more efficient system with better outcomes
at a lower cost. Our nation cannot continue to spend the most
money of any developed nation and have the worst outcomes.
In a globally competitive world, limited resources must go to
effective healthcare, balanced with education, infrastructure, the
environment, and other societal needs. A new healthcare model
could satisfy all these desires and needs.
Even iconic giants are starting to feel the pain of recent annual
losses in the billions. Ascension Health, Cleveland Clinic,
Jefferson Health, Massachusetts General Hospital, ProMedica,
Providence, UPMC, and many others have gone from stable
and sustainable to stressed and uncertain. Mayo Clinic had
been a notable exception, but recently even this esteemed
system’s profit dropped by more than 50% in 2022 with higher
wage and supply costs up, according to this Modern Healthcare
summary. [14]
The alarming point is even the big multigenerational health
system leaders who believed they had fortress balance sheets
are struggling. Those systems with decades of financial success
and esteemed reputations are in jeopardy. Changing leadership
doesn’t change the new environment.
Nonprofit healthcare systems’ income typically comes from three
sources — operations, namely caring for patients in ways that are
now evolving as noted above; investments, which are inherently
risky evidence by this past year’s record losses; and philanthropy,
which remains fickle particularly when other investment returns
disappoint potential donors. For-profit healthcare systems don’t
have the luxury of philanthropic support but typically are more
efficient with scale and scope.
The most stable and predictable source of revenue in the
past was from patient care. As the healthcare industry’s cost
to society continues to increase above 20% of the GDP, most
medically self-insured employers and other payors will search for
efficiencies. Like it or not, persistently negative profit margins
will transform healthcare.
Demand for nurses, physicians, and support folks is increasing,
with many shortages looming near term. Labor costs and burnout
have become pressing stresses, but more efficient delivery of
care and better tools can ameliorate the stress somewhat. If
structural process and technology tools can improve productivity
per employee, the long-term supply of clinicians may keep up.
Additionally, a decreased demand for care resulting from an
effective prevention strategy also could help.
Most other successful industries work hard to produce products
or services with fewer people. Remember what the industrial
revolution did for America by increasing the productivity of each
person in the early 1900s. Thereafter, manufacturing needed
fewer employees.
PATIENTS’ NEEDS AND DESIRES
Patients want to live a long, happy and healthy life. The best
way to do this is to avoid illness, which patients can do with
prevention because 80% of disease is self-inflicted. When
prevention fails, or the 20% of unstoppable episodic illness kicks
in, patients should seek the best care.
The choice of the “best care” should not necessarily rest just on
convenience but rather objective outcomes. Closest to home may
be important for take-out food, but not healthcare.
Care typically can be divided into three categories — acute,
urgent, and elective. Common examples of acute care include
childbirth, heart attack, stroke, major trauma, overdoses, ruptured
major blood vessel, and similar immediate, life-threatening
conditions. Urgent intervention examples include an acute
abdomen, gall bladder inflammation, appendicitis, severe
undiagnosed pain and other conditions that typically have
positive outcomes even with a modest delay of a few hours.
Most every other condition can be cared for in an appropriate
timeframe that allows for a car trip of a few hours. These illnesses
can range in severity from benign that typically resolve on their
own to serious, which are life-threatening if left undiagnosed and
untreated. Musculoskeletal aches are benign while cancer is life-threatening if not identified and treated.
Getting the right diagnosis and treatment for both benign and
malignant conditions is crucial but we’re not even near perfect for
either. That’s unsettling.
In a 2017 study,
“Mayo Clinic reports that as many as 88 percent of those
patients [who travel to Mayo] go home [after getting a
second opinion] with a new or refined diagnosis — changing
their care plan and potentially their lives. Conversely, only
12 percent receive confirmation that the original diagnosis
was complete and correct. In 21 percent of the cases, the
diagnosis was completely changed; and 66 percent of
patients received a refined or redefined diagnosis. There
were no significant differences between provider types
[physician and non-physician caregivers].” [15]
The frequency of significant mis- or refined-diagnosis and
treatment should send chills up your spine. With healthcare
we are not talking about trivial concerns like a bad meal at a
restaurant, we are discussing life-threatening risks. Making an
initial, correct first decision has a tremendous influence on
your outcome.
Sleeping in your own bed is nice but secondary to obtaining the
best outcome possible, even if car or plane travel are necessary.
For urgent and elective diagnosis/treatment, travel may be a
good option. Acute illness usually doesn’t permit a few hours of grace, although a surprising number of stroke and heart attack victims delay treatment through denial or overnight timing. But even most of these delayed, recognized illnesses usually survive. And urgent and elective care gives the patient the luxury of some time to get to a location that delivers proven, objective outcomes, not necessarily the one closest to home.
Measuring quality in healthcare has traditionally been difficult for the average patient. Roadside billboards, commercials, displays at major sporting events, fancy logos, name changes and image building campaigns do not relate to quality. Confusingly, some heavily advertised metrics rely on a combination of subjective reputational and lagging objective measures. Most consumers don’t know enough about the sources of information to understand which ratings are meaningful to outcomes.
Arguably, hospital quality star ratings created by the Centers for Medicare and Medicaid Services (CMS) are the best information for potential patients to rate hospital mortality, safety, readmission, patient experience, and timely/effective care. These five categories combine 47 of the more than 100 measures CMS publicly reports. [16]
A 2017 JAMA article by lead author Dr. Ashish Jha said:
“Found that a higher CMS star rating was associated with lower patient mortality and readmissions. It is reassuring that patients can use the star ratings in guiding their health care seeking decisions given that hospitals with more stars not only offer a better experience of care, but also have lower mortality and readmissions.”
The study included only Medicare patients who typically are over
65, and the differences were most apparent at the extremes,
nevertheless,
“These findings should be encouraging for policymakers
and consumers; choosing 5-star hospitals does not seem to
lead to worse outcomes and in fact may be driving patients
to better institutions.” [17]
Developing more 5-star hospitals is not only better and safer
for patients but also will save resources by avoiding expensive
complications and suffering.
As a patient, doing your homework before you have an urgent or
elective need can change your outcome for the better. Driving a
couple of hours to a CMS 5-star hospital or flying to a specialty
hospital for an elective procedure could make a difference.
Business case studies have noted that hospitals with a focus on
a specific condition deliver improved outcomes while becoming
more efficient. [18] Similarly, specialty surgical areas within
general hospitals have also been effective in improving quality
while reducing costs. Mayo Clinic demonstrated this with its
cardiac surgery department. [19] A similar example is Shouldice
Hospital near Toronto, a focused factory specializing in hernia
repairs. In the last 75 years, the Shouldice team has completed
four hundred thousand hernia repairs, mostly performed under
local anesthesia with the patient walking to and from the
operating room. [20] [21]
THE BOTTOM LINE
The Mayo Brother’s quote, “The patient’s needs come first,” is
more relevant today than when first articulated over a century
ago. Driving treatment into distinct categories of acute, urgent,
and elective, with subsequent directing care to the appropriate
facilities, improves the entire care process for the patient. The
saved resources can fund prevention and decrease the need for
future care. The healthcare industry’s focus has been on sickness,
not prevention. The virtuous cycle’s flywheel effect of distinct
categories for care and embracing prevention of illness will decrease
misery and lower the percentage of GDP devoted to healthcare.
Editor’s note: This is a multi-part series on reinventing the healthcare
industry. Part 2 addresses physicians, non-physician caregivers, and
communities’ responses to the coming transformation.