Category Archives: Consumer Engagement
Patients Are Delaying Healthcare – Findings From 2022 BDO Patient Experience Survey
https://www.linkedin.com/pulse/patients-delaying-healthcare-findings-from-our-new-survey-shill/

Since the early days of the pandemic, the healthcare industry has faced seemingly insurmountable challenges to ensure access to high-quality care. While healthcare providers have performed admirably in the face of these challenges, patients are still seeing access challenges that are impacting their behaviors — which can lead to challenges in the long run.
In the 2022 BDO Patient Experience Survey, they sought to learn how patients feel about their providers and healthcare experience — from making appointments and interacting with care providers, to how patients access health insurance and who patients turn to for routine care.
From the survey of over 3,000 U.S. adults, they came across a few key takeaways:
1. Delaying routine care is the new norm
Americans face a troubling dilemma: While 92% have health insurance and 91% have a regular care provider, 58% admit to delaying routine medical care in the past 12 months.
For routine (non-emergency) care, 69% of respondents report seeing a primary care physician and 12% routinely visit primary care nurse/nurse practitioner or physician assistant. Just 9% do not have a provider for routine medical care. Our survey found that Americans use a wide variety of health insurance options with employer-sponsored insurance (32%) being the most popular, followed by Medicare (28%), Medicaid (14%) and individual private insurance (7%). While 8% report having no health insurance, even those with insurance faced significant barriers to care.
Of those who delayed seeking medical care in the past 12 months, 30% cite unaffordability due to high out-of-pocket costs and 19% say they could not afford to seek care due to a lack of insurance. In addition to the high costs of medical care, many Americans struggle with a lack of cost transparency.
2. Cost transparency is a continuing problem
Nearly a third of Americans (31%) have never tried to obtain cost estimates for medical care. When patients do not know what healthcare will cost, many avoid seeking necessary care. A critical way we can improve patient access to healthcare is to understand how patients like to obtain cost estimates.
Of patients surveyed who have sought cost estimates, most prefer to reach out to a person, with 38% preferring to contact their insurance provider and 37% opting to ask the healthcare provider’s administrative staff. On the digital side, 31% say they obtained cost estimates by looking at online patient portals and 27% look to health provider or medical facility websites.
3. Most patients experience frustration when seeking and receiving care
We know that long appointments lead times and high costs cause patients to put off care — but how do patients feel about the actual care they receive? 69% of Americans experience frustration during routine medical appointments, with having to wait for a late provider (29%), not getting enough time with the provider (22%) and having too much paperwork to fill out (21%) being the most common frustrations.
When providers make it easier for patients to receive care, their efforts are noticed. Patients say providers make care more accessible by offering telehealth appointments (32%), reaching out to proactively schedule appointments (29%), offering walk-in appointments (27%) and implementing online/self-service scheduling (23%).
Patients are facing a challenging care environment — and so are providers. Fortunately, there are ways that providers can improve access and the care experience for their patients without breaking their budgets.
More health systems are charging patients to message their physicians
https://mailchi.mp/0622acf09daa/the-weekly-gist-december-2-2022?e=d1e747d2d8

A growing number of health systems have begun to bill for certain electronic communications with patients via portals like MyChart. The systems instituting these practices, including Cleveland Clinic and Chicago-based Northwestern Medicine, have justified the billing based on the time demands placed on their providers to answer messages involving additional efforts, including extensive patient chart review. Northwestern shared that fewer than one percent of MyChart messages incurred fees, which are typically covered by insurance, and require patient consent before billing.
The Gist: In a time of significant margin pressure, we understand the instinct to seek additional revenue by collecting whatever reimbursement is available. However, in the ongoing transition to technology-enabled hybrid care, this practice has the potential to confuse, or even drive away, patients, who finally began to embrace virtual provider communication during the pandemic.
Viewing portal messaging as a “digital front door” for patients, rather than a revenue-generating service in and of itself, may prove more fruitful in the long run.
Amazon launches direct-to-consumer virtual care platform
https://mailchi.mp/4b683d764cf3/the-weekly-gist-november-18-2022?e=d1e747d2d8

On Tuesday, the e-commerce giant unveiled its latest healthcare endeavor, Amazon Clinic, a “virtual health storefront” that can asynchronously connect patients to third-party telemedicine providers. It offers diagnosis and treatment for roughly 20 low-acuity, elective health conditions—including acne, birth control, hair loss, and seasonal allergies—at flat, out-of-pocket rates. (The service does not currently accept insurance.) It also refills prescriptions, which customers can send to any pharmacy, including Amazon’s. At its launch, Amazon Clinic is available in 32 states.
The Gist: This is exactly the kind of venture at which Amazon excels: creating a marketplace that’s convenient for buyers and sellers (patients and telemedicine providers), pricing it competitively to pursue scale over margins, and upselling customers by pairing care with Amazon’s other products or services (like Amazon Pharmacy).
Its existing customer base and logistics expertise could position it to replace telemedicine storefront competitors, including Ro and Hims & Hers, as the leading direct-to-consumer healthcare platform, at least among those that don’t take insurance.
It bears watching to see how Amazon builds on this service, including whether it eventually incorporates insurance coverage, partners with health systems (similar to Hims & Hers), or connects Amazon Clinic to Prime in order to attract greater numbers of—generally young, healthy, and relatively wealthy—consumers.
Telehealth blurs the line between Prescription and Over-the-Counter Drugs
https://mailchi.mp/e60a8f8b8fee/the-weekly-gist-september-23-2022?e=d1e747d2d8

A recent STAT News article highlights a concerning new trend in direct-to-consumer pharmaceutical marketing, enabled by access to virtual care. Pitched as a tool for patient empowerment, pharmaceutical companies are now offering consumers immediate treatment for a variety of health conditions at the click of a button that says, “Talk to a doctor now.”
Over 90 percent of eligible patients receive a prescription for the drug they “clicked” on, after connecting with a virtual care provider on a third-party telehealth platform. Not only does this practice give drug companies direct access to prospective patients, but it also delivers lucrative data on patient age, zip code, and medication history that can be used to target marketing efforts.
The Gist: Articles like this remind us why the US is one of only two countries in the world that allows direct-to-consumer marketing of prescription drugs (the other, interestingly, is New Zealand).
As the number of Americans with a primary care provider continues to decline, this kind of Amazon-style, easy-button drug shopping experience will be increasingly appealing to many consumers. But wherever innovation outpaces regulation, situations in which for-profit companies prioritize profits over providing the best care for patients are sure to occur.
While we support the idea of greater consumer empowerment in healthcare, we worry that this highly fragmented approach to consumer-driven health can result in abuse and patient harm.
Setting the post-COVID agenda for health systems
https://mailchi.mp/9e0c56723d09/the-weekly-gist-july-8-2022?e=d1e747d2d8

As the economic situation has worsened over the past few months, we’ve been working with several health systems to recalibrate strategy. For many, the anticipated “post-COVID recovery” period has turned into a struggle to reverse declining (often negative) margins, while still scrambling to address mounting workforce shortages. All this amid continued pressure from disruptive competitors and ever-rising consumer expectations.
In the graphic above, we’ve pulled together some of the most important changes we believe health systems need to make. These range from improvements to the operating model (shifting to a team-based approach to staffing, greater use of automation where appropriate, and moving to asset-light capital strategies) to transformations of the clinical model (moving care into lower-cost outpatient and community settings, integrating virtual care into clinical delivery, and creating tighter alignment with key physicians).
In general, the goal is to deliver lower-cost care in less expensive settings, using less expensive staff.
But those cost-saving strategies will need to be coupled with a new go-to-market approach, including new payment models that reward systems for shifting away from high-cost (and highly reimbursed) care models.
Employers and consumers will expect more solution-based offerings, which integrate care across the continuum into coherent bundles of service. This will require a more deliberate focus on service line strategies, moving away from a fragmented, inpatient-centric model.
Contracting approaches must align payment with this shift, changing incentives to reward coordinated, cost-effective, outcomes-driven care.
A key insight from our discussions with health system leaders: short-term cost-cutting initiatives to “stop the bleed” won’t suffice—instead, more permanent solutions will be required that address not only the core operating model, but also the approach to revenue generation.
The post-COVID environment is turning out to be a lot tougher than many had expected, to say the least.
Cartoon – Customer-Centric Engagement
Cartoon – Modern Service Station
How other industry players are expanding their healthcare platforms
https://mailchi.mp/31b9e4f5100d/the-weekly-gist-june-03-2022?e=d1e747d2d8

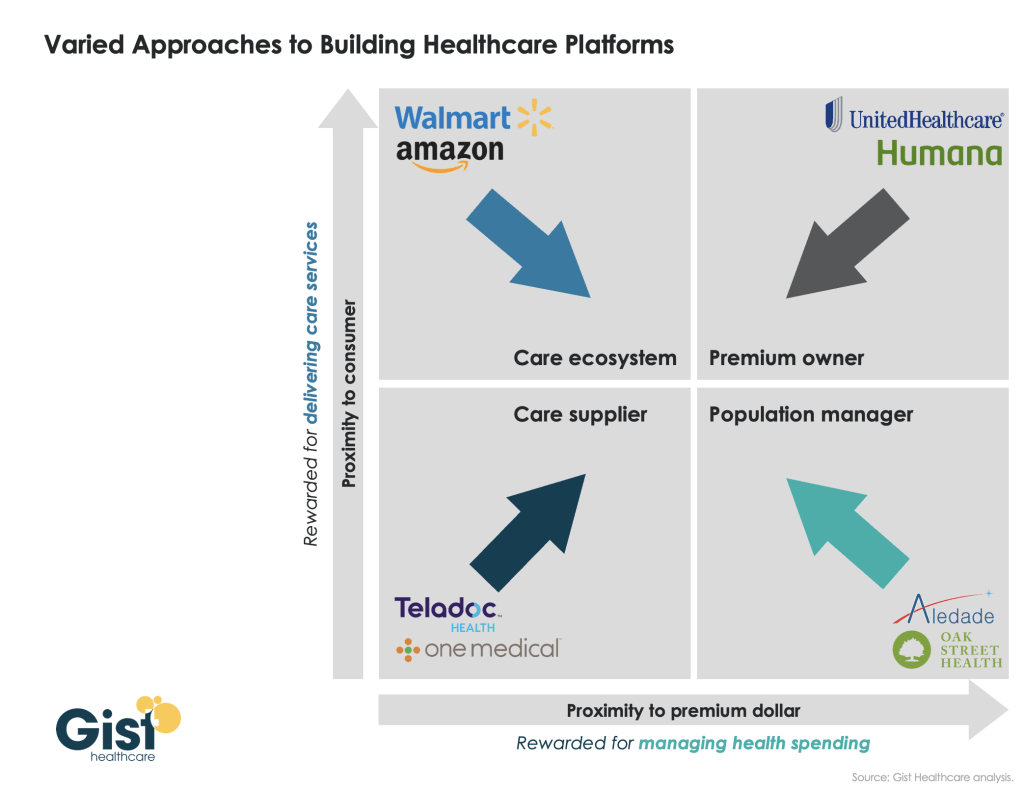
Last week, we introduced our framework for value delivery as a “healthcare platform”, in which an organization’s proximity to both the consumer and to the premium dollar determines how it competes as a “care supplier,” a “care ecosystem,” a “premium owner,” or a “population manager.” Traditionally, different healthcare companies have operated primarily in one of these four domains. However, as shown in the graphic below, we’ve recently seen many shift their business into one or more additional quadrants, as they seek to expand their value propositions. UnitedHealth Group is an obvious example: it has moved well beyond the traditional insurance business, via numerous provider and care delivery acquisitions across the continuum.
Other players have shifted from their own “pure play” positions toward more comprehensive “platform” strategies as well: One Medical adding Iora Health to enhance population health capabilities; Walmart moving beyond retail and pharmacy services, partnering with Oak Street Health to expand its ability to manage Medicare patients; Amazon getting into the employer health business.
There’s a clear pattern emerging—value propositions are converging on a “strategic high ground” that encompasses all four dimensions of platform value, creating a comprehensive set of solutions to deliver accessible care, promote health, and grow consumer loyalty, with an aligned financial model centered on managing the total cost of care. Health systems looking to build platform strategies will find many of these competitors also vying for pride of place as the “platform of choice” for healthcare consumers and purchasers.
CVS Health to launch a virtual-first primary care platform
https://mailchi.mp/31b9e4f5100d/the-weekly-gist-june-03-2022?e=d1e747d2d8

The digital platform is designed to provide consumers with a coordinated healthcare experience across care settings. It’s being sold to Aetna’s fully insured and self-insured plan sponsors, as well as CVS Caremark clients, and is due to go live next year. According to CVS Health, the new offering “enables consumers to choose care when and where they want,” whether that’s virtually, in a retail setting (including at a MinuteClinic or HealthHUB), or through at-home services.
Patients will have access to primary care, on-demand care, medication management, chronic condition management, and mental health services, as well as help in identifying other in-network care providers.
The Gist: CVS Health has been working to integrate its retail clinics, care delivery assets, and health insurance business. This new virtual-first care platform is aimed at coordinating care and experience across the portfolio, and streamlining how individuals access the range of services available to them.
CVS is not alone in focusing here: UnitedHealth Group, Cigna, and others have announced virtual-first health plans with a similar value proposition. Any payer or provider who aims to own the consumer relationship must field a similar digital care platform that streamlines and coordinates service offerings, lest they find themselves in a market where many patients turn first to CVS and other disruptors for their care needs.