On Thanksgiving more than a century ago, many Americans were living under quarantines, and officials warned people to stay home for the holiday.
More than 200,000 dead since March. Cities in lockdown. Vaccine trials underway.
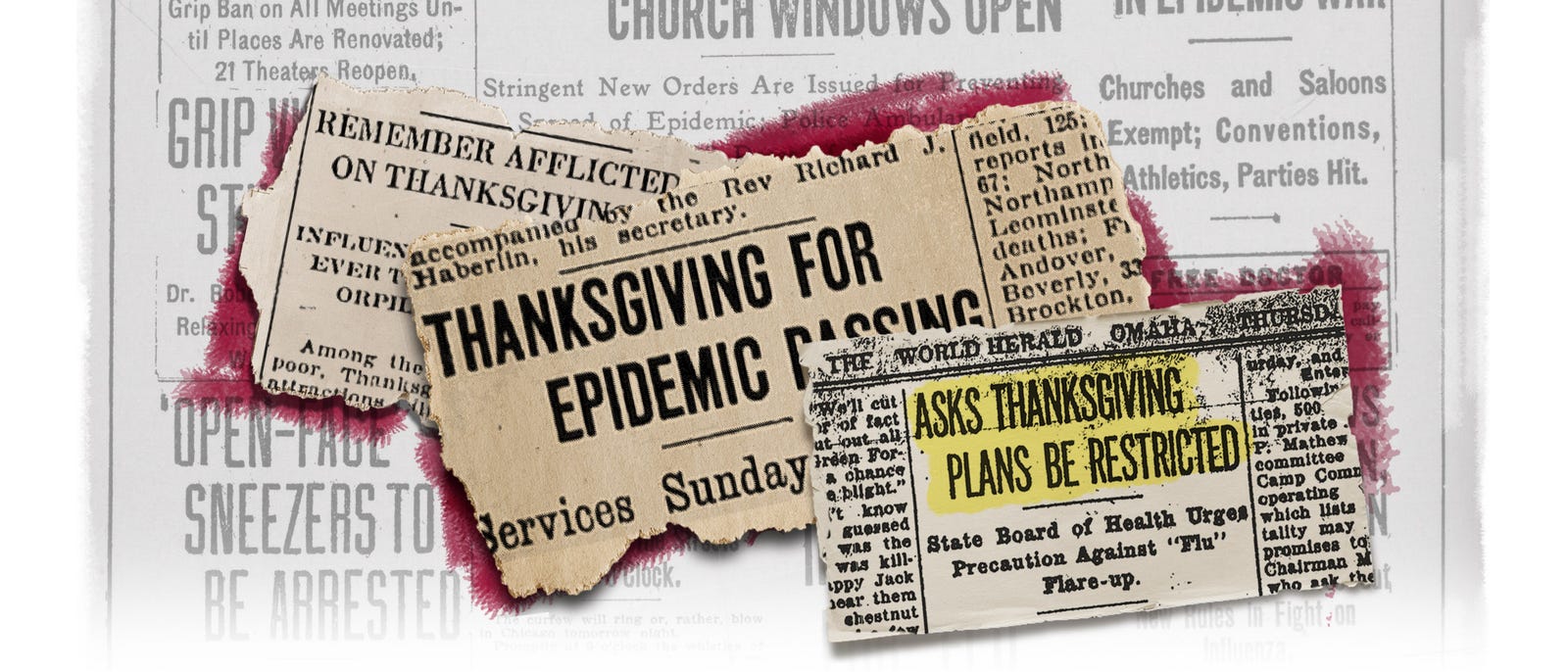
And a holiday message, of sorts: “See that Thanksgiving celebrations are restricted as much as possible so as to prevent another flare-up.”
It isn’t the message of Thanksgiving 2020. It’s the Thanksgiving Day notice that ran in the Omaha World Herald on Nov. 28, 1918, when Americans found themselves in a similar predicament to the millions now grappling with how to celebrate the holiday season amid the coronavirus pandemic.
“Every time I hear someone say these are unprecedented times, I say no, no, they’re not,” said Brittany Hutchinson, assistant curator at the Chicago History Museum. “They did this in 1918.”
On Thanksgiving more than a century ago, many Americans, like today, lived under various phases of quarantines and face mask orders. Millions mourned loved ones. And health officials in many cities issued the same holiday warning: Stay home and stay safe.
Giving thanks for WWI victory, beating pandemic
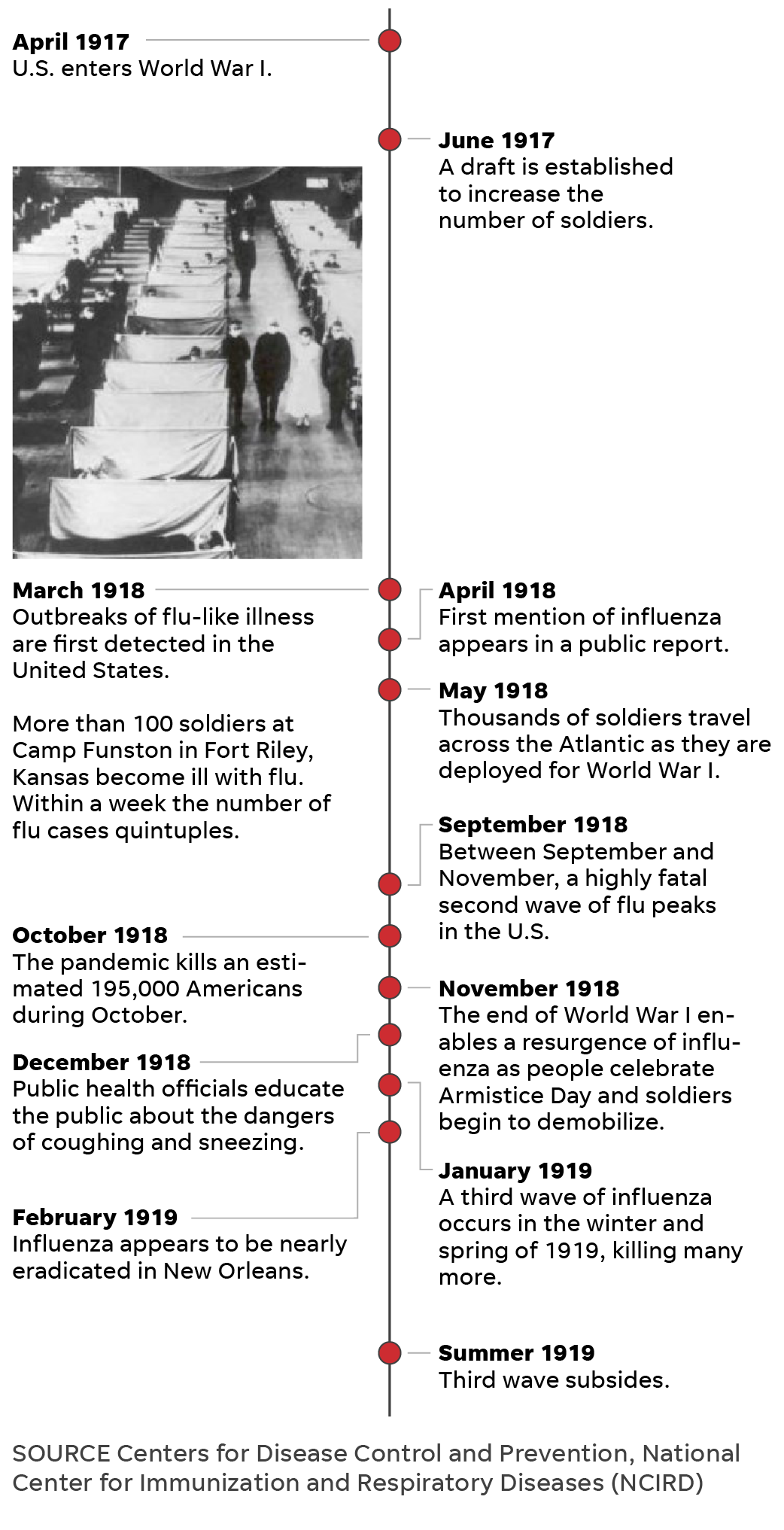
By late November 1918, the USA – in the midst of the suffrage movement, Jim Crow and the tail end of WWI – battled the ebbing second wave of the H1N1 influenza epidemic, also known as the Spanish flu.
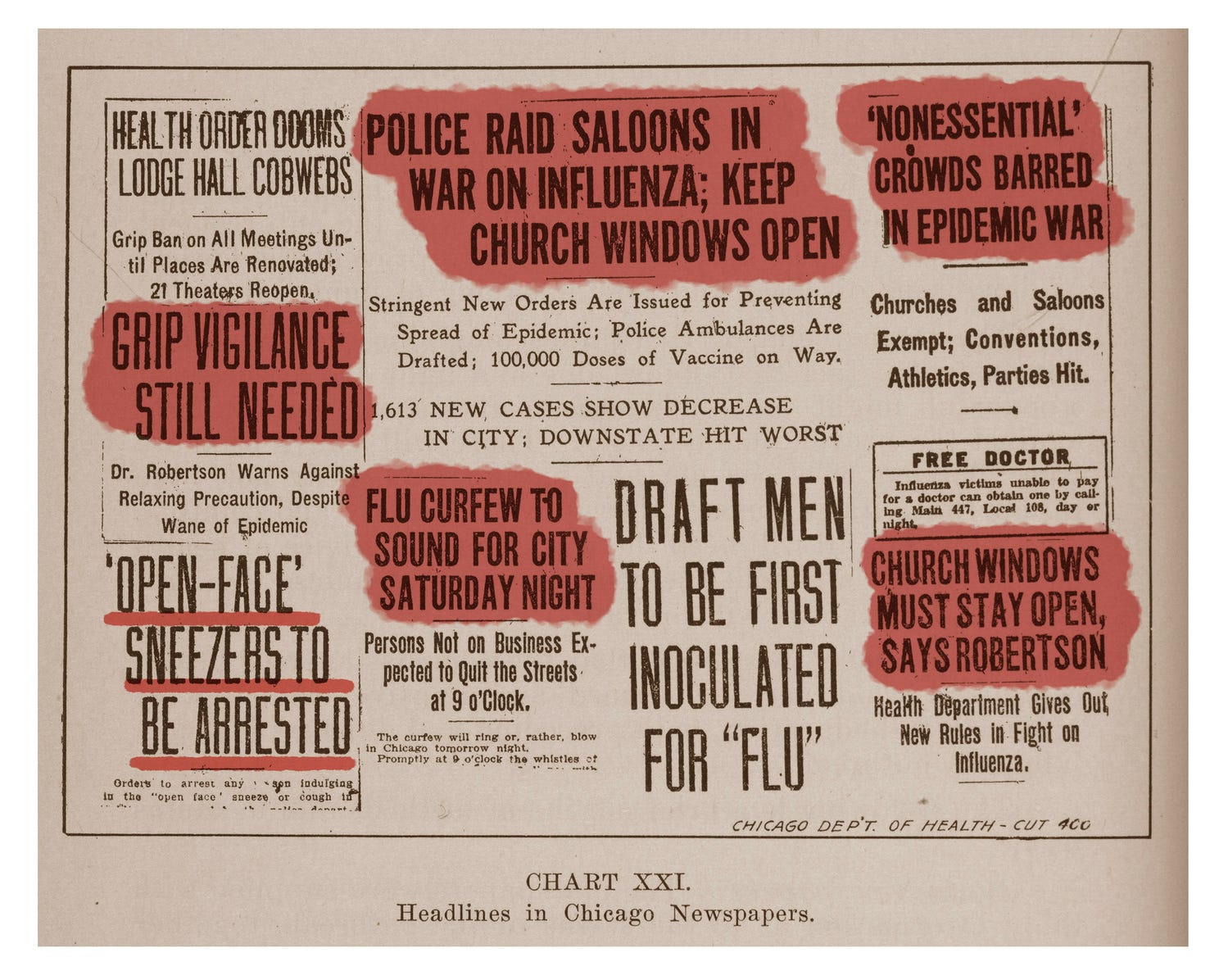
The first cases were detected in the USA in March of that year, growing exponentially by the fall. In October, the virus burned through the nation. Dozens of cities implemented face mask orders and curfews and locked down for two to three weeks, temporarily closing schools, libraries, theaters, movie houses, dance halls, churches, ice cream parlors and soda shops. The virus killed about 195,000 Americans during October alone.

As Thanksgiving rolled around, some cities celebrated the relaxation of flu-related restrictions– partly due to opposition campaigns by retailers, theater owners, unions, mass transportation companies and other economically stressed stakeholders. Washington, Indianapolis and Oakland, California, had lifted restrictions days before, and San Francisco was on the brink of lifting its mask mandate.
San Francisco had one of the nation’s largest anti-masking campaigns, spearheaded by the Anti-Mask League of San Francisco, according to Howard Markel, a professor of the history of medicine at the University of Michigan and co-editor-in chief of The American Influenza Epidemic of 1918-1919. Many people refused to wear masks and were arrested, and when the “line into the courtroom was so long, they laid off arresting people because the system couldn’t enforce it,” Markel said.
On Nov. 13, the San Francisco Examiner reported that “Thanksgiving Day will be celebrated in San Francisco by the discarding of gauze masks, if the present rate of decrease in influenza continues.”
A week later, San Franciscans ceremoniously removed their masks as a whistle sounded across the city at noon. “San Francisco Joyously Discards Masks In Twinkling; Faces Beam As Gauze Covers Come Off At Time Fixed,” the San Francisco Chronicle wrote on its front page Nov. 22.

Resistance to public health measures was not as “vociferous or widespread as today,” but it was there, Markel said. “A lot of these rules and regulations were wrapped up in the patriotism of World War I, and most people followed them. But we don’t have that unifying situation right now. You would think the pandemic would be unifying.”
In some cities, Thanksgiving rituals brought a welcome sense of normalcy. Many Americans returned to religious services, performed charity work and went through with planned football games, parties and performances.
In Portland, a “grand reunion service” was planned for the Sunday after Thanksgiving, “in honor of the reassembling after being debarred from worship on account of the epidemic for the last five weeks.” Members of various congregations were “ready to greet each other after the long absence,” according to the Oregon Daily Journal on Nov. 16.
“The chimes of church bells will once more be heard on Sunday morning throughout the city, beckoning one and all to attend their chosen place of worship, where a double celebration will be held, first over the suppression of autocracy and, second, over the eradication of a frightful plague,” the paper wrote.
Rabbis, priests, pastors and more conveyed a unified message, Hutchinson said – one of “forgiveness and compassion.”
“People are urging to be considerate of one another, to care for one another,” Hutchinson said. “There are messages of putting the smallness of the individual into perspective with the vastness of humanity.”
Other cities were still trending in the opposite direction.
Lockdowns, quarantines on Thanksgiving
By the end of November, cases were rising in cities such as Atlanta, Denver, Louisville, Kentucky, Milwaukee, Omaha, Nebraska, Portland, Oregon, and Richmond, Virginia. Many health experts attributed the “renewal of the grip epidemic” to festivities Nov. 11 – later designated as Armistice Day – when thousands flooded the streets to celebrate the end of WWI.
“It is not the lifting of the closure ban that is the cause of spreading of the epidemic but the putting aside of all precautions and restrictions by the people of Denver when they celebrated on Victory Day,” City Manager of Health and Charity William H. Sharpley told the Denver Post in a story Nov. 21.

On Nov. 27, the day before Thanksgiving, St. Louis reported its highest new daily case count since the epidemic began, and Buffalo, New York, reported its largest jump in daily cases since the lifting of its pandemic ban weeks earlier. Both cities subsequently cracked down on public gatherings, limited the number of passengers on streetcars and ordered those cars to be ventilated and cleaned.
In Salt Lake City, residents were under “quarantine” on Thanksgiving, shops were prohibited from holding sales and celebrations were postponed until Christmas Day. Placards indicating households infected with influenza were placed on the front and rear entrances of 2,000 homes.
“Owing to the influenza quarantine, the day’s festivities … had to be postponed till Christmas day. But Thanksgiving services of some sort are being held in nearly every home,” an article on the front page of the Desert Evening News said. “Because the influenza quarantine prevents public gatherings, the day in Utah is being observed quietly and without any spectacular features.”
Officials in Los Angeles promoted a “Stay at Home Week” over Thanksgiving. The Los Angeles Times issued a call on its front page to “REMEMBER AFFLICTED THANKSGIVING DAY; Influenza Ban Is Felt,” saying, “Thanksgiving Day held many attractions, although in a modified sense.”
“The salvation Army served fifty pounds of turkeys to fifty old men, but dispensed with its usual big dinner to the outcasts at the headquarters, because of the influenza ban,” the Times wrote.
Denver, which was under a face mask order, had just opened three emergency hospitals and issued an urgent call for nurses. Churches were expected to hold Thanksgiving services, but “extra precautions will be taken to guard against spread of epidemic,” the Rocky Mountain News reported the day before.
“Special pains have been taken to provide all the ventilation necessary and to make attendance at the services safe in spite of the influenza epidemic. In a number of churches electric fans have been placed in the auditoriums so as to change the air every few minutes,” the article said.
In many cities, traditional Thanksgiving Day pageants were held outside. In Cincinnati, which saw a surge in cases among children and firemen, Thanksgiving “exercises” at school were held in auditoriums instead of classrooms to “avoid crowding,” the Cincinnati Enquirer wrote Nov. 28.
A handful of cities began to see a surge in cases on Thanksgiving.
Cities see cases rise on Thanksgiving
Cincinnati health officials “requested parents to forego children’s parties and gatherings during the Thanksgiving vacation,” but the number of hospitalized patients rose on the holiday. Schools added an extra day of vacation to the Thanksgiving holiday break to promote “a beneficial result in the influenza situation.”
“We are not in a happy frame of mind tonight,” Dr. Walter List, superintendent of the city’s General Hospital, told the Cincinnati Enquirer on Thanksgiving. “An institution such as this can stand the strain of an epidemic for five or six weeks, but when it continues for such a long period the situation is complicated.”
Kansas City saw a similar trend. The week of Thanksgiving, the number of flu cases at the city’s General Hospital doubled, and on Thanksgiving Day, city health officials reinstituted home quarantine for influenza victims and their families. Schools on break for Thanksgiving were closed until further notice.
Public dance halls and restaurants were closed on Thanksgiving in Spokane, Washington, and private parties were prohibited. The next day, the city’s emergency hospital received more applications for admission than on any other day during the entire epidemic. On Thanksgiving, “the hospital was filled and death a frequent visitor,” the Spokesman-Review wrote.

Jefferson, Iowa, physician C.W. Blake spent much of his Thanksgiving evening making house calls on people ill from influenza, author Thomas Morain wrote in his 1998 book, “Prairie Grass Roots.” Blake was attending a Thanksgiving dinner at a farm outside town and let the local phone operator know he would be available later in the day. When he received the call about patients in the early evening, the operator had a list of 54 patients who had come down with the flu that day.
“At one farm north of Jefferson a family of four was too sick even to make themselves the most simple meal,” Morain wrote. “While Blake checked each one, (his assistant) made a soup from ingredients on hand and left it for the family.”
Hopes of a vaccine on Thanksgiving
By the fall of 1918, scientists were working on an influenza vaccine, and many were developed and used over the course of the pandemic. Researchers in New York, Boston, Pittsburgh, New Orleans and Seattle developed vaccines, and thousands of people in those cities and many others were inoculated.
Days before Thanksgiving, health officers in Rochester, New York, encouraged people to obtain the vaccine available at a health bureau. In Salt Lake City, the emergency hospital gave more than 100 vaccinations Nov. 30. By early December, free inoculation clinics were established across the city, and thousands of residents lined up for their vaccinations.

The problem? Researchers didn’t know influenza was a virus.
“The vaccine that was made was a vaccine against (a bacteria), which they thought was the cause of influenza,” Markel said. “So not only were vaccines of this era crude and not all that effective, the vaccine that they did produce was for the wrong organism.”
Vaccine science was nowhere near the scientifically advanced level of 2020, said Markel, whose mother died from COVID-19 this year. The study of virology was in its infancy, and researchers didn’t have the tools to see viruses. Though bacteria are much larger and can be viewed under a light microscope, viruses require an electron microscope, which had not been invented in 1918, Markel said.
The vaccines that researchers developed did not stop an impending third wave of the flu.
Third wave of influenza surges after the holidays
Just as cases rose after Armistice Day celebrations, they rose again after Thanksgiving. Dallas, Minneapolis, San Antonio, San Francisco and Seattle saw surges. Omaha relaunched a public health campaign. Parts of Cleveland and its suburbs closed schools and enacted influenza bans in early December.
On Dec. 6, the St. Paul Daily News announced that more than 40 Minneapolis schools were closed because of the flu, below the headline “SANTA CLAUS IS DOWN WITH THE FLU.” Health officials asked “moving picture show” managers to exclude children, closed Sunday schools and ordered department stores to dispense with “Santa Claus programs.”
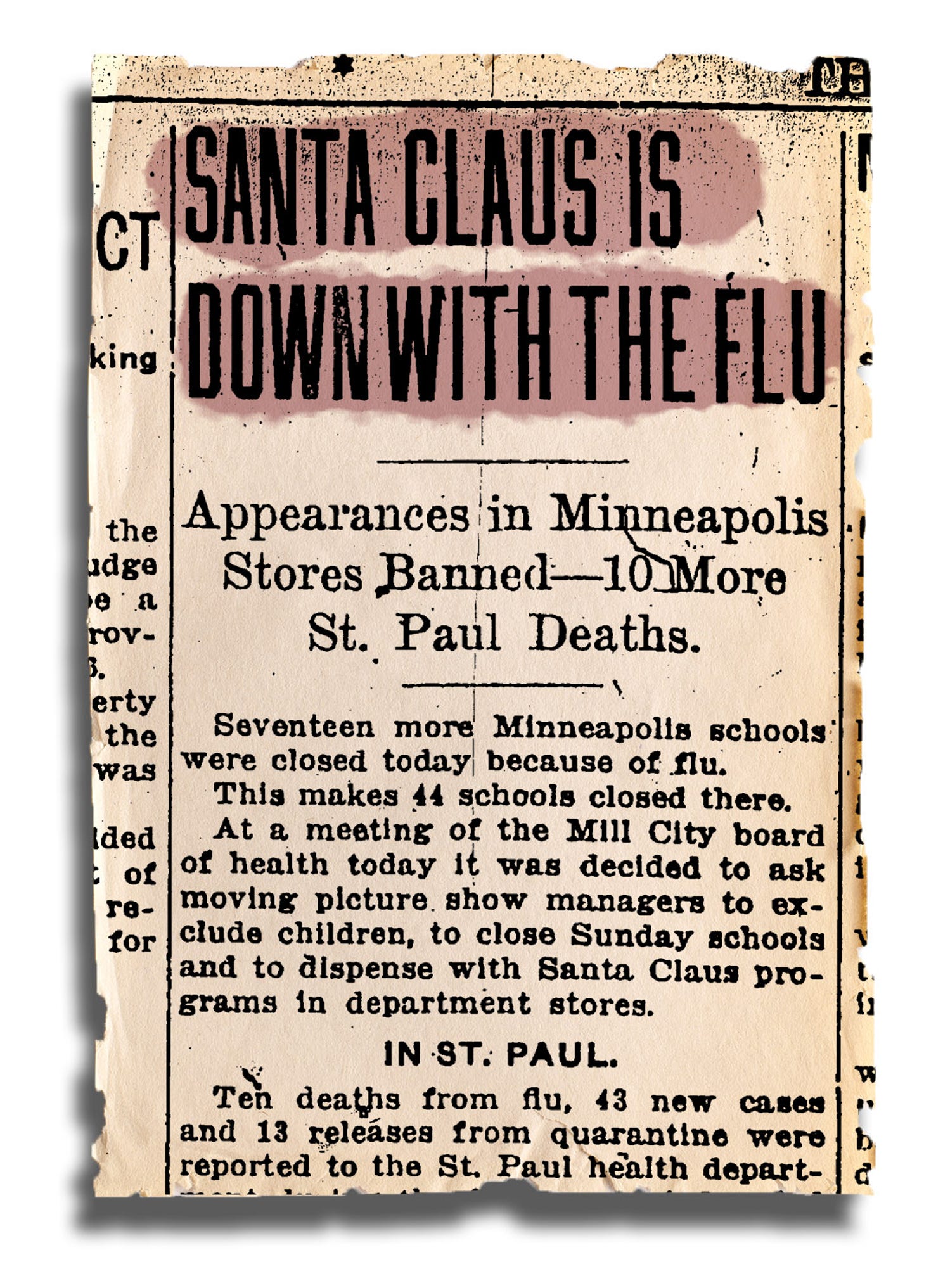
On Christmas Eve, health officials in Nebraska made influenza a mandatory quarantine disease, and fines ranged from $15 to $100 for violations. Approximately 1,000 homes in Omaha were placarded, meaning their occupants were unable to leave for at least four days after the fever had subsided.
In Denver, the Salvation Army canceled its annual Christmas parties for children, and the Women’s Press Club canceled its New Year’s Eve ball. School Christmas assemblies were canceled in Fall River, Massachusetts, and families with an influenza patient in their homes were warned not to entertain guests and barred from borrowing books from the library.
By January, the USA was fully engulfed in its third wave of influenza. The virus spread throughout the winter and spring, killing thousands more. It infected one-third of the world’s population and killed approximately 675,000 Americans before subsiding in the summer of 1919.
“What did they do wrong? That’s hard to say, but all of these measures are like Swiss cheese. They have holes, so you try to use as many layers as possible,” Markel said. “To me, those surges just represented whether there was social distancing or not. Flu didn’t stop circulating, the question was when did people go out and get exposed to it? And that’s what’s going on now.”
A warning for 2020: ‘Stay home and stay safe’
A century later, the nation has recorded more than 12 million cases of COVID-19, and more than 255,000 people in the USA have died. Dozens of states reimplemented coronavirus-related restrictions, and health officials echo the stay-at-home guidance issued decades ago.
“The risk of not traveling is less than the risk of traveling,” Anthony Fauci, the nation’s leading infectious disease expert, told USA TODAY Wednesday. “During this interesting period of a lot of infection going on, colder weather, indoors: Do you want to travel and go to a Thanksgiving meal where there may be 12, 15, 20 people?”
Fauci said his three adult daughters won’t come home for Thanksgiving this year. Hutchinson, the Chicago-based curator who had COVID-19 in April, said she plans to celebrate Thanksgiving at home with her dog and Facetime family members. Markel, in Ann Arbor, said he plans to eat Thanksgiving dinner alone, downsize from a full turkey to a sliced turkey breast and Zoom with family.
If history tells us anything, Markel said, it’s that “the risk of contracting the virus or spreading the virus by congregating in groups or even traditional holiday parties is right now too great.”
“It is disappointing, but let’s get through this, so we can celebrate many, many more Thanksgivings,” he said. “The better part of valor is to stay home and stay safe.”