https://www.yahoo.com/news/steep-plunge-virus-cases-every-120859155.html

The number of new coronavirus cases is increasing in every state, setting off a growing sense of concern from health officials who are warning that the pandemic in the United States is far from over, even though the national outlook is far better than during previous upticks.
The 160 million people across the country who are fully vaccinated are largely protected from the virus, including the highly contagious delta variant, scientists say. In the Upper Midwest, the Northeast and on the West Coast — including in Chicago, Boston and San Francisco — coronavirus infections remain relatively low.
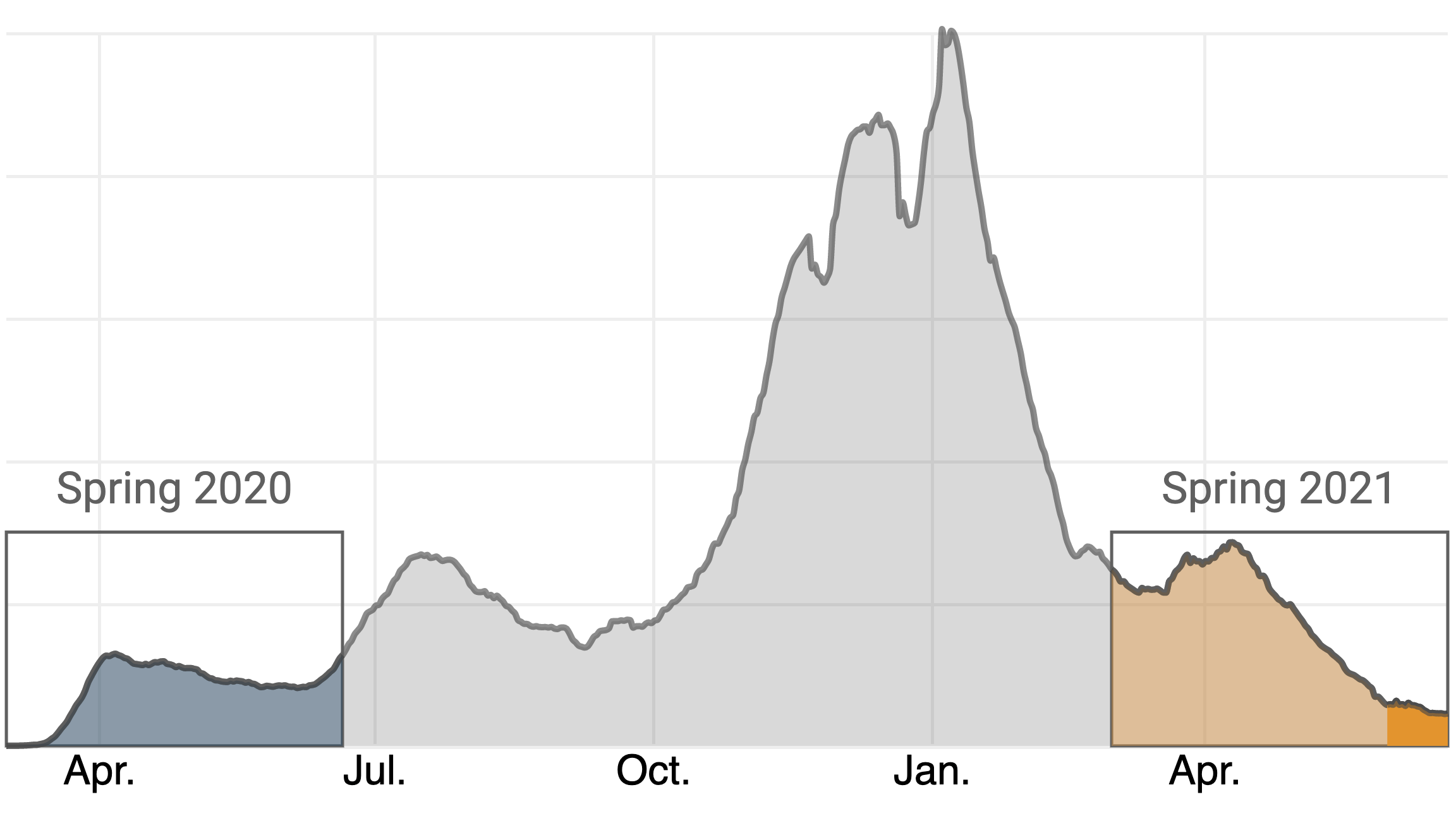
But the picture is different in pockets of the country where residents are vaccinated at lower rates. Hot spots have emerged in recent weeks in parts of Missouri, Arkansas and Nevada, among other states, leaving hospital workers strained as they care for an influx of coronavirus patients. Less than a month after reports of new cases nationally bottomed out at around 11,000 a day, virus cases overall are increasing again, with about 26,000 new cases a day, and hospitalizations are on the rise.
The country is at an inflection point, and experts said it was uncertain what would come next. While nationwide cases and hospitalization numbers remain relatively low, more local hot spots are appearing and the national trends are moving in the wrong direction. Many of the oldest, most vulnerable Americans are already inoculated, but the vaccine campaign has sputtered in recent weeks.
“This will definitely be a surge,” said Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota. “It won’t be as big as what happened in January. But we still have 100 million people in the United States who are susceptible to COVID-19.”
Intensive care beds in hospitals have become scarce in parts of Missouri, where officials in Springfield on Wednesday asked for an alternative care site. In Mississippi, where cases are up 70% over the past two weeks, health officials have urged older adults to avoid large indoor gatherings even if they have been vaccinated. And in Los Angeles County, officials said Thursday that masks would once again be required indoors, regardless of vaccination status, because of the spread of the delta variant.
The slowdown of the vaccination effort has amplified concerns. About 530,000 people are now receiving a vaccine each day, a sharp decrease from 3.3 million shots a day in April. Less than half of the United States population has been fully vaccinated.
Still, the country’s prognosis remains better than at previous points in the pandemic. The vaccines are widely available, cases and hospitalizations remain at a tiny fraction of their peaks and deaths are occurring at some of the lowest levels since the early days of the pandemic.
Yet daily case numbers have increased in all 50 states, including 19 states that are reporting at least twice as many new cases a day.
Mayor Quinton Lucas of Kansas City, Missouri, where cases are increasing but remain far below levels in other parts of the state, said he worried that the outbreak in southwestern Missouri would keep spreading, given low vaccination rates there. He said strong recommendations for mask wearing — or even new mandates — may become necessary if his city’s outlook continued to worsen.
“I think when you start to see Springfield-level hospitalizations here in the Kansas City metro, then we’ll have to very seriously consider whether it’s time to return to previous restrictions,” Lucas said.
In a string of news conferences this week, public health officials pleaded with people who have not gotten shots to change their minds, urging them to consider that coronavirus vaccines are safe, free and available to anyone ages 12 and older.
“To any who have been hesitating about being vaccinated, please, I implore you to hesitate no longer,” Dr. Kiran Joshi, the senior medical officer for the Cook County Department of Public Health, which serves suburban Chicago, said Thursday.
Even in places in the United States that have not yet seen a significant uptick in infections, governors and public health officials worried that their states were vulnerable to an outbreak.
“I hope and pray that it doesn’t come to West Virginia and just absolutely runs across our state like wild,” said Gov. Jim Justice, whose state has recorded relatively few cases recently but has a low vaccination rate. “But the odds are it will.”
Few places are more worrisome than in Missouri, where a surge among unvaccinated people has left hospitals scrambling to keep up.
Just two months ago, when there were only 15 active coronavirus cases in his southwestern Missouri county, Larry Bergner, the director of the Newton County Health Department, had hoped the end of the pandemic might be in sight.
That has not happened.
As the delta variant has spread across the country, it has sent case totals spiking in Newton County, where less than 20% of residents are fully vaccinated. Bergner’s county now has a higher rate of recent cases than any state.
“It does give, I guess, some depression to think that we thought we were coming out of it, now here we go again, how high are we going to get,” Bergner said.
In Milwaukee County, where 48% of residents are fully vaccinated, the health department has tried to push the number higher by setting up a vaccine site outside the Fiserv Forum, where the Milwaukee Bucks are playing in the NBA Finals. Fewer than two dozen people have received a vaccine each day the site was in place, said Dr. Ben Weston, the director of medical services for the Milwaukee County Office of Emergency Management.
“In March, people flooded to our vaccination sites — all we had to do was open a door,” Weston said. “Now we have to go out and find people.”
As case numbers slowly rise, a sense of worry has begun to creep in for some Americans, even those who are fully vaccinated.
Vince Palmieri, 89, who gets around Los Angeles on public transportation, said he worried when he saw fellow riders not wearing masks as required. Though per capita case rates remain relatively low in Los Angeles County, they have grown sharply in recent weeks. The county is averaging about 1,000 new cases a day, up from fewer than 200 a day in mid-June.
“Once you get on a bus or a train you’re in no man’s land,” said Palmieri, who continues to wear a mask. “Their sneeze could take somebody out, but I’m frightened to talk up about the disease because people get ugly.”
Debora Weems, 63, who lives in New York City, has been following the case numbers closely. Her anxiety about the virus has risen alongside cases. New York City, which averaged fewer than 200 new cases a day in late June and early July, is now averaging more than 400 a day, far below past peaks.
“I’m just afraid we’re going to have to shut down again,” Weems said. Both she and her mother, who is 85, are vaccinated, but now she worries that their protection is not enough.
When the case numbers were at their lowest, she moved through the city more freely, with less thought about whether people nearby were vaccinated. But now she is trying to avoid leaving her neighborhood, and recently put up a new sign on her apartment door with a request: She and her mother are not receiving visitors because of COVID-19.