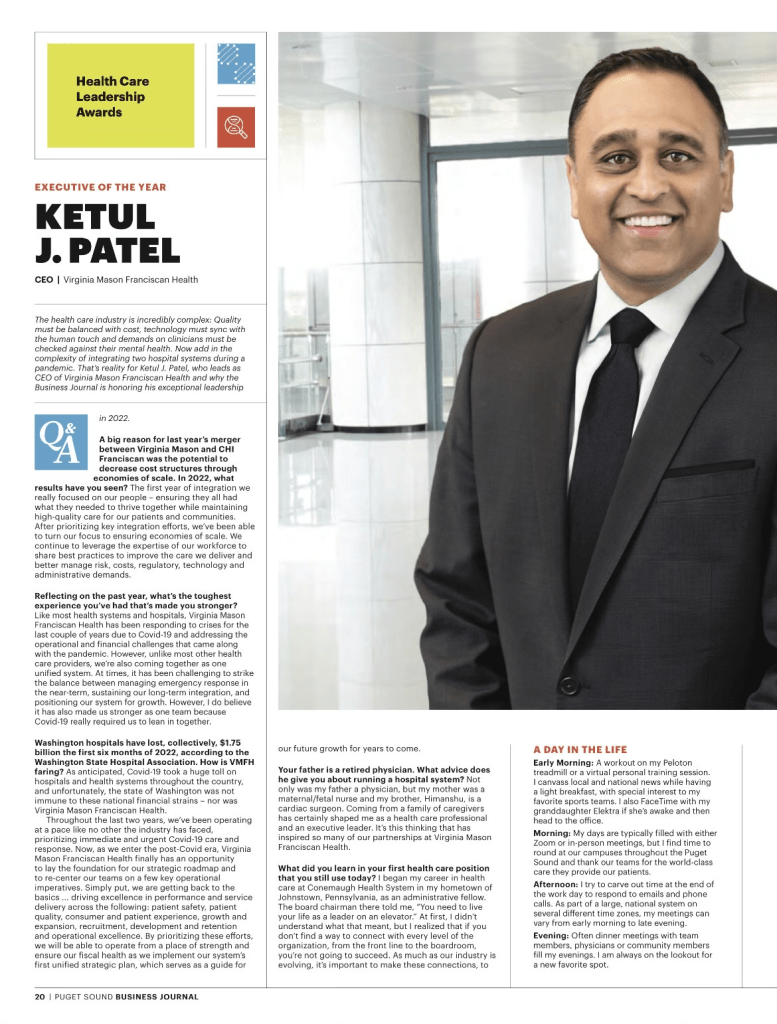
Regular readers know I’ve long been curious about the forces driving one essential question in healthcare today:
Why is it so hard to run a hospital now? One area worth exploring is the interplay between the healthcare system and our nation’s changing demographics.
Baby Boomers have been displaced as the largest generation of adults in America. Millennials now hold that position, and Gen Z will likely outnumber Baby Boomers in the workplace sometime this year. Our nation is rapidly diversifying, as more than two-fifths of Americans identify as people of color.
It’s not just a matter of who we are as a nation that’s changing; how we live is evolving, too. The number of 40-year-olds who’ve never been married reached record highs in 2022, according to the Pew Research Center, dovetailing with a steadily growing trend since 1970 toward single living.
The U.S. Census published a report earlier this year showing that nearly 29% of American households include only one person. Further, the U.S. fertility rate is at an all-time low — and, according to a Pew survey, may not recover, given that 47% of those under 50 said they were unlikely to have children. That’s an increase of 10 percentage points since 2018.
The effects of this are starting to shape our broader culture. Solo living has been cited as a contributing factor to the housing crisis, and we’re starting to hear more about how people are grappling with the practical implications of retiring while living alone. This column in The New York Times is just one example.
As for the potential health effects of living alone, in 2023, U.S. Surgeon General Vivek Murthy raised an alarm with a report documenting the negative effects of social isolation on individual and public health. Murthy outlined a host of risks, including cardiovascular disease, hypertension, diabetes and increased susceptibility to infectious disease. Mental health is a major concern. A 2024 study published in National Health Statistics Reports found that people who live alone were more likely to be depressed, particularly if they lacked social or emotional support.
All of this adds up to an increasing burden on the U.S. healthcare system.
As providers who care for the socially isolated already know, it’s impossible to operate as usual if a patient lacks family support. Hospitals and the traditional American family structure are fundamentally intertwined. When family support is not available for a medical emergency, then the entire hospital episode becomes more fragile. Patient discharge procedures assume someone is available at home to help with care, assist in transporting patients for follow-up visits, and engage with the business office around billing and insurance.
Without this family safety net, the potential for readmission rises, harming patient outcomes, increasing costs and putting quality ratings at risk. The rise in younger people living alone also raises further financial implications, given that about 45% of Americans access health insurance through employer-sponsored programs. If someone living alone becomes too sick to work, patients may be less able to pay for care when they need it most.
This is just another in a long list of challenging hospital operational dilemmas. How best to respond to such profound change in the American demographic landscape? The right strategy may be to re-think consumer segmentation.
Consumer segmentation has become very popular at the clinical product level, but perhaps the next level of service segmentation is not among disease types but based on demographic characteristics.
As an increasing portion of the American population has less family support to navigate a hospital stay or chronic illness, it will become more important to identify these patients and determine which new and enhanced services need to be provided to them by the hospital. Social work programs will need to be more robust, and health systems should invest in community partnerships to help bridge the resource gap. But the wide-ranging nature of patients’ practical needs will likely require healthcare leaders to think creatively.
Consider the scope:
- Care coordinators: Particularly for patients with complex conditions, it may be beneficial to designate a care coordinator to oversee healthcare planning.
- Home health care: Without family members to help with day-to-day care, more nurses and aides will be needed to provide healthcare at home as well as help with day-to-day living. For patients with less demanding healthcare needs, adult day care may be useful.
- Medication management: Patients need to understand how to take their medications, watch for potential side effects and interactions, and develop a system to make sure they take them on time. Further, they may need help navigating the pharmacy, either in getting prescriptions filled or with financial assistance programs.
- Meal delivery: Nutrition is vital to a patient’s recovery, and ensuring patients have access to healthy options can help to reduce the likelihood of readmission.
- Personal emergency response systems: Patients may need devices to call for help during an emergency as well as medical bracelets or other methods for communicating important information to first responders.
- Housekeeping assistance: Hospitals may need to help connect patients with resources to maintain clean, safe homes.
- Volunteer companions: While volunteer companions usually help elderly patients with social interaction and basic needs, it may be necessary to develop programs that target a wider range of ages.
- Transportation services: Patients need help getting to and from follow-up visits.
- Telehealth: Remote care will become increasingly important. Clinical services should consider whether care plans could be adjusted to reduce the number of in-person visits.
Beyond targeting resources, consumer segmentation also offers an opportunity to communicate with patients in a more effective and personalized way. This sort of engagement fosters trust and increases loyalty that’s particularly important, given the intimate nature of healthcare.
It’s long been true that the stronger the family system, the better off hospitals are. But as the concept of the American family shifts, and in this case, unwinds, healthcare leaders need to be attuned to new demands—and nimble enough to meet them. This requires making the most of the information you have today to plan for tomorrow.