https://www.healthcaredive.com/news/beyond-the-aca-healthcare-legal-fights-to-watch-in-2020/569793/

All eyes were on the legal drama over the Affordable Care Act as 2019 drew to a close — and while that case remains a focus for this year — a lot more is also at stake.
Payers and providers are fiercely contesting a price transparency push from the Trump administration that would force privately negotiated rates out into the open. The administration is also being challenged over regulations regarding risk corridor payments to payers and the expansion of association health plans.
Antitrust concerns are also front and center, as payers clash over exclusive broker policies in Florida.
As policy debates rage on this year through presidential debates and on Capitol Hill, courthouses will also be a key battleground for the industry in 2020. Below are the big cases to watch.
ACA and the high court
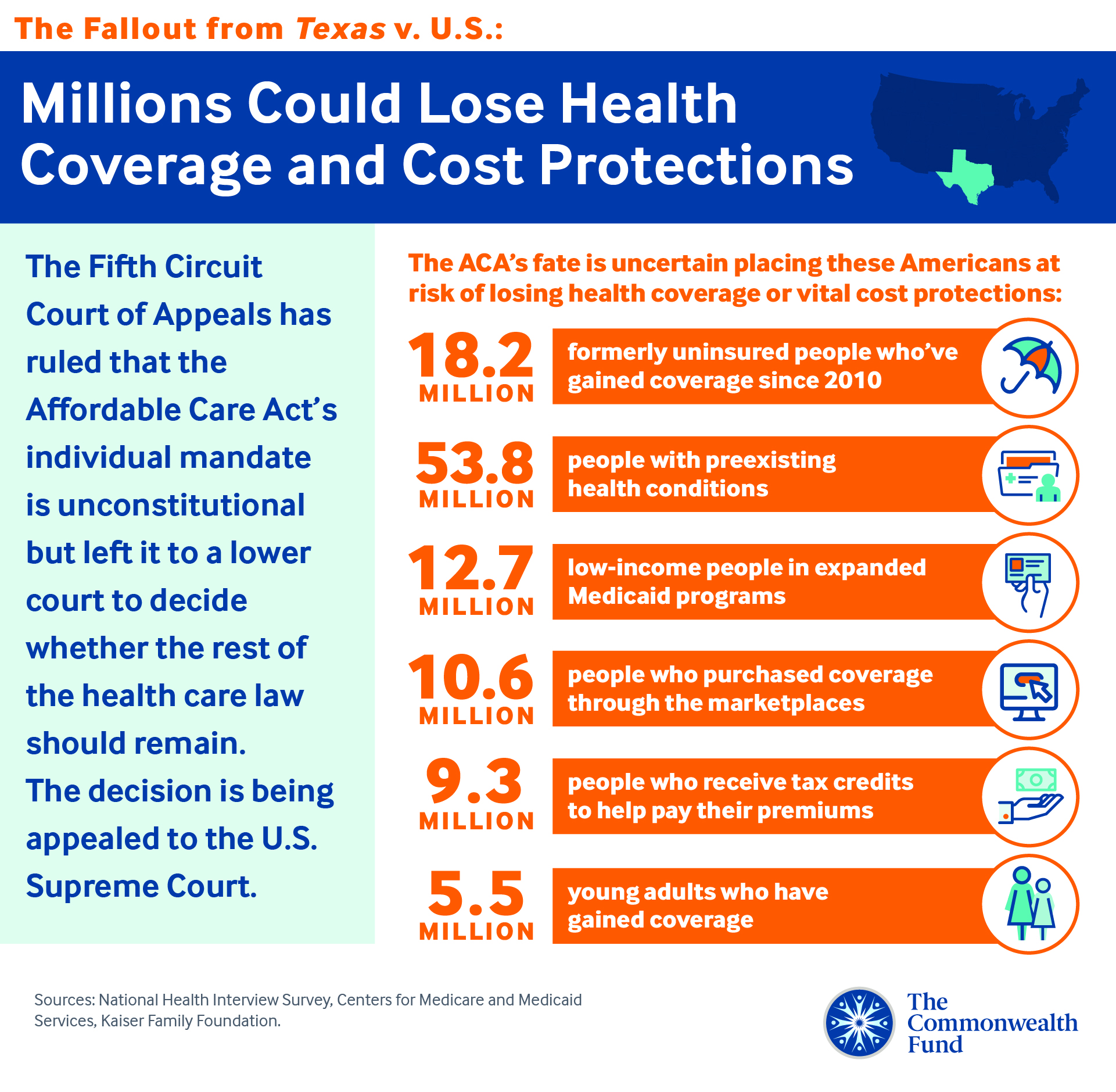
The most consequential case still making its way through the court system is the challenge to the Affordable Care Act. At the end of last year, an appeals court notched a win for the red states fighting the law by declaring the individual mandate was no longer constitutional after the penalty was zeroed out by a Republican-controlled Congress.
The three-judge panel, however, stopped short of declaring the entire ACA void, instead asking the lower court that made the argument that the rest of the law is not severable from the individual mandate to revisit and clarify its ruling.
Supporters of the ACA are trying to speed up what is almost certainly the next major step for the court case by petitioning the Supreme Court on Friday to hear the case before the November presidential election.
“States, health insurers, and millions of Americans rely on those provisions when making important — indeed, life-changing — decisions. The remand proceedings contemplated by the panel majority would only prolong and exacerbate the uncertainty already caused by this litigation,” according to the Jan. 3 petition filed by California Attorney General Xavier Becerra and a coalition of 19 other states and D.C.
Five justices are needed to approve the suggested expedited timeline while four are needed to agree to hear the case at all. More will be clear in the next couple of months as justices make their decisions. The ultimate decision — whether it comes in months or years — will have huge ramifications across the healthcare landscape.
Price transparency pushback
The legal clash between hospitals and the administration over forcing providers to reveal negotiated rates is set to heat up quickly in the new year.
The federal judge overseeing the case recently released a timeline for how it is expected to proceed in the coming months. Hospitals are seeking a swift ruling and summary judgment. HHS faces a Feb. 4 deadline to file its opposition motion to the summary judgment, while deadlines for motions extend through March 10.
“That is an extremely accelerated schedule,” James Burns, a partner at Akerman, told Healthcare Dive. “My strong suspicion is that we’ll get a ruling from the judge late spring or earlier summer at the latest, which is obviously all before the election.”
Hospital groups including the American Hospital Association and health systems have alleged that the administration’s push to force negotiated rates out into the open exceeds the government’s authority and violates the First Amendment because it compels hospitals to reveal confidential and proprietary information. Legal experts say the principal argument will center around whether the government exceeded its authority, not the First Amendment.
Risk corridor payments
On last month’s Supreme Court docket was a case regarding an ACA risk adjustment program. At issue are $12 billion in payments insurers say they are owed from losses on state exchanges.
Early participants in the marketplaces were hit hard in some cases as they attempted to adjust to people gaining coverage under the ACA. A few nonprofit co-ops were driven to close when CMS declared the program had to be budget neutral and therefore only about one-eighth of the expected risk corridor amount could be paid out.
A number of justices seemed to lean toward ruling in favor of the insurers during arguments in front of the high court, Tim Jost, health law expert and professor emeritus at Washington and Lee University School of Law, told Healthcare Dive. “Only a couple of the justices that spoke seemed inclined to support the government, but we’ll see what happens there,” he said.
If the payers do prevail, there’s still the question of exactly how much they are owed and how the money will be distributed. It could ultimately affect medical loss ratio rebates or premiums down the road, he said.
CSR fight in court this week
The legal fight over canceled payments to insurers under the ACA drags on as oral arguments begin this week in a federal appeals court.
A number of insurers including Maine Community Health Options and Sanford Health claim they’re owed millions in cost-sharing reduction payments that the government failed to pay out after the Trump administration said Congress failed to appropriate the funds. The payments were intended to repay insurers for lowering the cost of care to make coverage affordable for those with low incomes.
Health Options and Sanford both won in the lower courts after judges ruled they were entitled to the unpaid CSR payments. The cases have been consolidated within the appeals court and oral arguments start Thursday.
A ruling in favor of insurers in the risk corridor case could be a good sign for their fight to be reimbursed for CSRs as well, Jost said.
Oscar antitrust argument
Health insurer Oscar has alleged that Blue Cross Blue Shield of Florida is enforcing a broker policy that is impeding Oscar’s ability to sell individual exchange plans and undermines competition in Florida.
The key question in this case is whether Florida Blue, a dominant insurer in the sunshine state, can lawfully bar independent brokers from working with other carriers like Oscar by threatening to cut off their ability to sell all other Florida Blue plans if they sell Oscar’s individual plans.
A lower court ruled against Oscar and found that such arrangements are shielded from antitrust scrutiny. A federal law excludes the “business of insurance” from antitrust scrutiny in some cases, legal experts say this case shouldn’t be exempt from antitrust enforcement.
A group of 10 antitrust scholars called the ruling “dangerous” and “plainly incorrect,” in an amicus brief Dec. 23 to the U.S. Court of Appeals for the 11th District.
“The practice at issue here — forming exclusive deals with industry gatekeepers to box out potential entry by competitors — is a quotidian business strategy that appears across many industries and raises well-recognized antitrust concerns,” according to the amicus brief.
Oscar alleges that consumers are harmed if brokers are barred from discussing other plan options outside Florida Blue.
The Department of Justice also intends to file an amicus brief, according to a recent filing in the appeals case.
Association, short-term health plans
The federal court of appeals in D.C. heard arguments late last year to review a judge’s decision in March 2019 declaring association health plans an “end-run” around the ACA. AHPs are offered by business or professional associations and aren’t bound by ACA requirements protecting pre-existing conditions and mandating essential benefits.
U.S. District Judge John Bates had strong language in March for the Trump administration, which is being challenged for loosening restrictions on what groups can offer AHPs — and therefore expanding their presence in the marketplace.
The D.C. appeals court is expected to rule on the case in the coming months. Jost’s take from the oral arguments is that the court seem inclined to reverse Bates’ decision, though he warned the outcome is not certain. “It’s a technical case that really has more to do with interpreting ERISA than the Affordable Care Act, though both are relevant,” he said.
A similar challenge has risen on short-term health plans, which were originally meant as stopgap coverage but have been expanded by the Trump administration to offer up to three years worth of coverage.
U.S. District Judge Richard Leon ruled in favor of the administration in July, saying the plans did not undermine the ACA. The plaintiffs, including the Association for Community Affiliated Plans, the National Alliance on Mental Illness and AIDS United, quickly appealed to the U.S. Court of Appeals in D.C.
Briefs are due this month and argument is likely in the spring, Jost said.
If AHPs and short-term plans are allowed to continue as the Trump administration has pushed for, it presents a concern for the viability of ACA risk pools. Consumer warnings against short-term plans, however, may be working, he said.
“There’s been a lot of publicity about how risky these plans are and I think they probably have not been achieving the same market strength they were hoping for,” he said.