Category Archives: Flexibility
Is there a silver lining for the systems who had the highest contract labor use?
https://mailchi.mp/d0e838f6648b/the-weekly-gist-september-8-2023?e=d1e747d2d8

Across the hospital industry, heavy reliance on contract labor in 2021 and 2022 caused a significant challenge for profitability.
However, a chief financial officer recently posited that his system’s large contract labor load has had unexpected benefits.
“Other hospitals [in our market] thought we were crazy to keep staffing with high contract rates until recently,” he shared. “But by keeping the agency nurses around a little longer, we were able to avert raising base salaries quite as much, and are in a better place today now that the labor market has softened.” It’s a story we’ve heard several times now.
While market rates for nursing and other clinical labor have undoubtedly been rebased, salary increases are sticky—it’s hard to adjust wages downward when the labor market loosens.
Systems who were able to avert large wage increases by increasing bonuses and other non-salary benefits, or forestalled permanent hiring at higher salaries by extending contract labor, now find themselves with more flexibility and potentially lower staffing costs in the long-term.
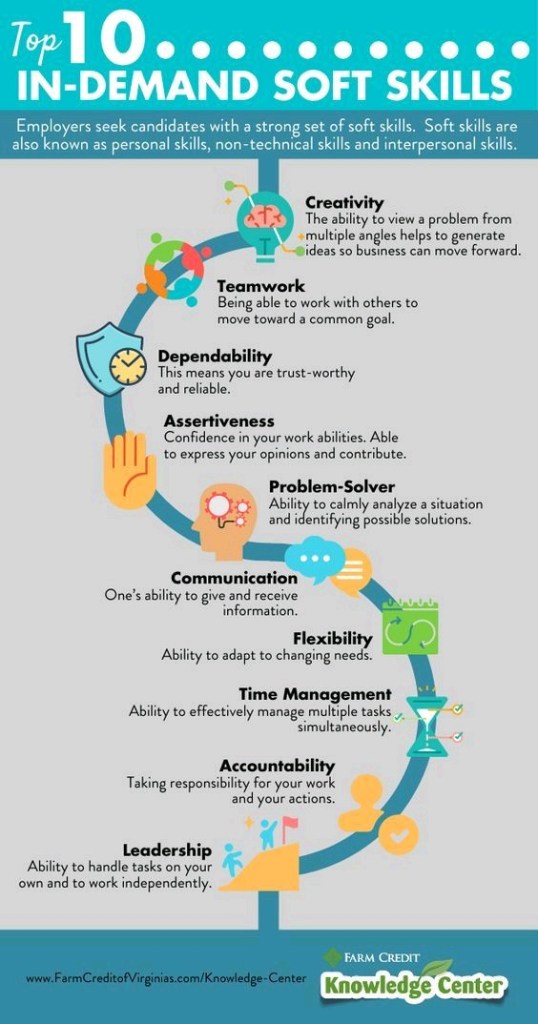
Top 10 In-Demand Soft Skills
Cartoon – New Year’s Resolutions
Cartoon – If We are to Succeed
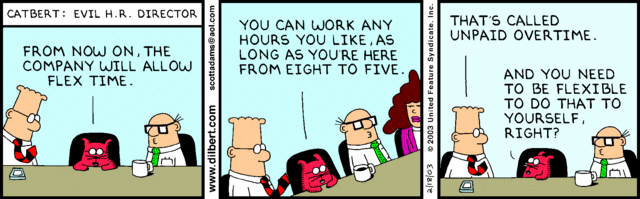
Cartoon – Flex Time
Cartoon – Lack of Flexibility Problem

UPMC CFO Edward Karlovich advises peers to ‘look beyond the challenges of today’

Edward Karlovich serves as the executive vice president and CFO for UPMC, a $23 billion provider and insurer based in Pittsburgh.
Since joining UPMC in 1990, Mr. Karlovich has served in several financial leadership roles. Most recently, he was vice president, CFO and chief of staff for UPMC’s Health Services Division. He became CFO of the entire integrated system with 40 hospitals in October 2020, after serving on an interim basis for about a year.
Here, Mr. Karlovich shares with Becker’s the skills he thinks CFOs need to succeed today, some key capital projects in the works at UPMC and his organization’s top financial priorities.
Editor’s note: Responses were lightly edited for length and clarity.
Question: What is the most pressing issue facing hospital CFOs due to COVID-19?
Edward Karlovich: I would say the most pressing issue for me is disruption. COVID-19 has done many things to disrupt the way we think about our organization and business. Some disruptions we faced in the last year include staffing and supply chain challenges. UPMC did a great job weathering through the supply disruptions and labor challenges. We always had adequate personal protective equipment for our folks here. We also really made a conscientious decision last year to keep our workforce intact; we didn’t lay off workers, and we took care of people who needed time off because of COVID-19. We also made sure employees knew they had the support of our executive leadership team. In summary, COVID-19 has created a disruption, and we must think about how things are different now coming out of the disruption.
Q: What are some things you are doing to work through the change/disruption?
EK: From an organizational perspective, we embarked on what we call the “UPMC experience” a few years ago. We looked at the way we are doing things to understand the experience of our employees and patients. This prepared us to be more creative in our thinking as to how we address challenges and disruption. We also learned through this the importance of interdependencies. Our business, both provider and insurance side, discussed a need to tackle the disruptions in an integrated way and discussed a need to communicate changes effectively. This year, we provided about 40 news conferences to get the standard message out across all of our regions. We also have a 90,000-plus employee organization which allows you to move around resources to deal with some challenges and disruptions.
Q: What are UPMC’s top financial priorities for 2022?
EK: From a financial perspective, we want to maintain a positive margin to support our capital investments and employees. To do this, we are focused on a few things. First, supporting our operating employees to ensure they can perform to the best of their ability. They are the ones who make the difference each and every day. Second, we want to make sure we, as a finance team, can provide the things that the organization needs to be successful. This includes, but is not limited to, making sure supply chain folks can get all needed supplies and ensuring we have the cash collections needed to fund our organization. Another priority is making sure we provide the advice and guidance needed to invest our dollars effectively so we can prepare for the next challenge.
Q: What are a few key capital projects UPMC has in the works?
EK: UPMC is a premier provider in our community, and we operate a number of specialty hospitals in the area. We are the primary pediatric, psychiatric, women’s health and oncology provider in the region. Over the past couple of years, we’ve embarked on a journey to provide new facilities in western Pennsylvania for these major programs. We are also investing heavily in a vision and rehabilitation institute, which is a $500 million project that will put our clinicians, researchers and other providers together to drive breakthroughs in vision care and rehabilitation.
We also are going to embark on a new tower for UPMC Presbyterian Oakland Campus [in Pittsburgh]. It is going to be the largest capital project we’ve embarked on since I’ve been here. This project will be more than $1 billion and is so important to the community.
The third thing we are looking at is enhancing our oncology services and product at UPMC Shadyside [in Pittsburgh]. What we’ve recognized is that we are the provider and insurer of choice in western Pennsylvania, and we have to invest in this community for the next 50 to 100 years.
Q: What skills are essential for hospital and health system CFOs to thrive in today’s healthcare landscape?
EK: The technical skills are given as CFO. To get in that leadership position, you have to be able to perform the necessary tasks. However, to make your organization better, I could boil it down to four things. First, you have to be a partner to your other senior leaders. Finance doesn’t exist in a vacuum. You have to be in the room with those folks, helping them manage and drive the business. The second thing is flexibility. If you think about what we experienced as an industry over the last two years, if you weren’t flexible, you were going to be seriously challenged. Flexibility is such an important attribute because the pace of change is going to accelerate in our industry. Third, I’d say talent recognition is a key skill. It is important to be able to find talent as well as mentor and develop them as employees who can provide a great service to the organization. Fourth, you have to embody integrity. There is no doubt in my mind that integrity is a core value that is essential to everything you do as a finance leader. You have to maintain your integrity at all times. Those are essential skills. If you’re going to be a successful CFO now, you have to have those skills outside of the technical.
Q: What is one piece of advice you would offer to another healthcare CFO, and why?
EK: I’d say, look beyond the challenges of today. It’s not just about what you can actually see and envision in front of you. Try to look at the implications that are not necessarily top of mind. What the future holds is uncertain for all of us in healthcare now. You need to be thinking about what things might be coming down the road that will change our business and commitment to our communities dramatically. Try to brainstorm around that. Trying to think forward and speculate about what might happen is very valuable.
Consolidation as a force for good—at least during COVID
https://mailchi.mp/b0535f4b12b6/the-weekly-gist-march-12-2021?e=d1e747d2d8

| When Jeff Goldsmith and Ian Morrison talk, people listen (apologies to E.F. Hutton…Goldsmith and Morrison are old enough to get that reference, anyway). These two lions of health policy and strategy came together recently to pen an editorial in Health Affairs examining the impact of large integrated health systems on the nation’s response to COVID-19. Morrison and Goldsmith admit to often finding themselves on opposite sides of consolidation issue, but looking back over the past year, both agree the scale systems have built over decades has been foundational to their effective and rapid response to the pandemic, which they rate as “better than just about any other element of our society”. Larger health systems were able to mobilize the resources to secure protective gear as supplies dwindled. They responded at a speed many would have thought impossible, doubling ICU capacity in a matter of days, and shifting care to telemedicine, implementing their five-year digital strategies during the last two weeks of March. This kind of innovation would have been impossible without the investments in IT and electronic records enabled by scale—but systems also exhibited an impressive degree of “systemness”, making important decisions quickly, and mobilizing across regional footprints. Given the financial stresses experienced by smaller providers, consolidation is sure to increase. And the Biden healthcare team will likely bring more scrutiny to health system mergers. Morrison and Goldsmith urge regulators to reconsider the role of health systems. The government should continue to pursue truly anticompetitive behavior that raises employer and consumer prices. But lawmakers should focus less on the sheer size of health systems and rather on their behavior, considering the potential societal impact a combined system might deliver—and creating policy that takes into account the role health systems have played in bolstering our public health infrastructure. |
Cartoon – Importance of Flexibility