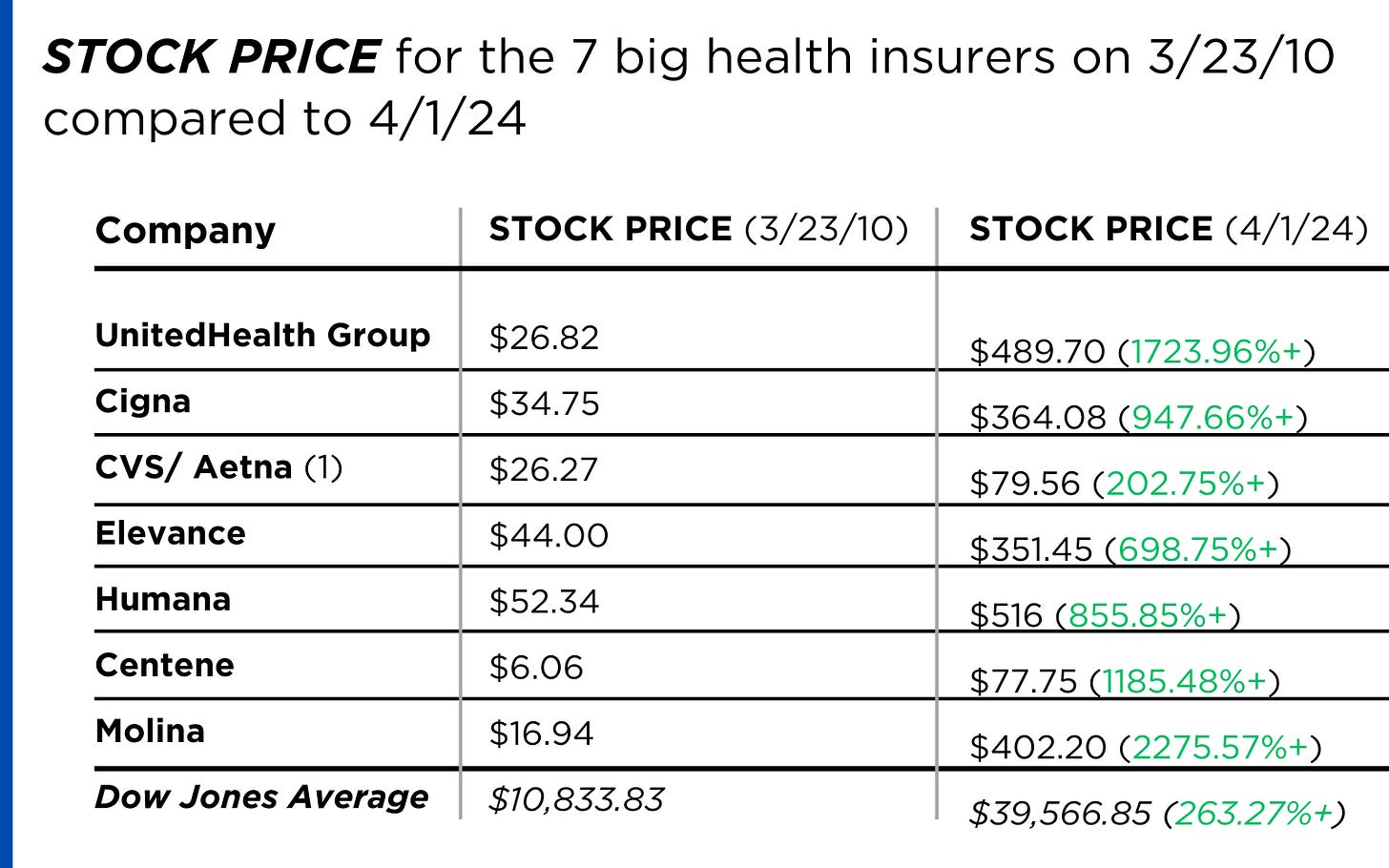
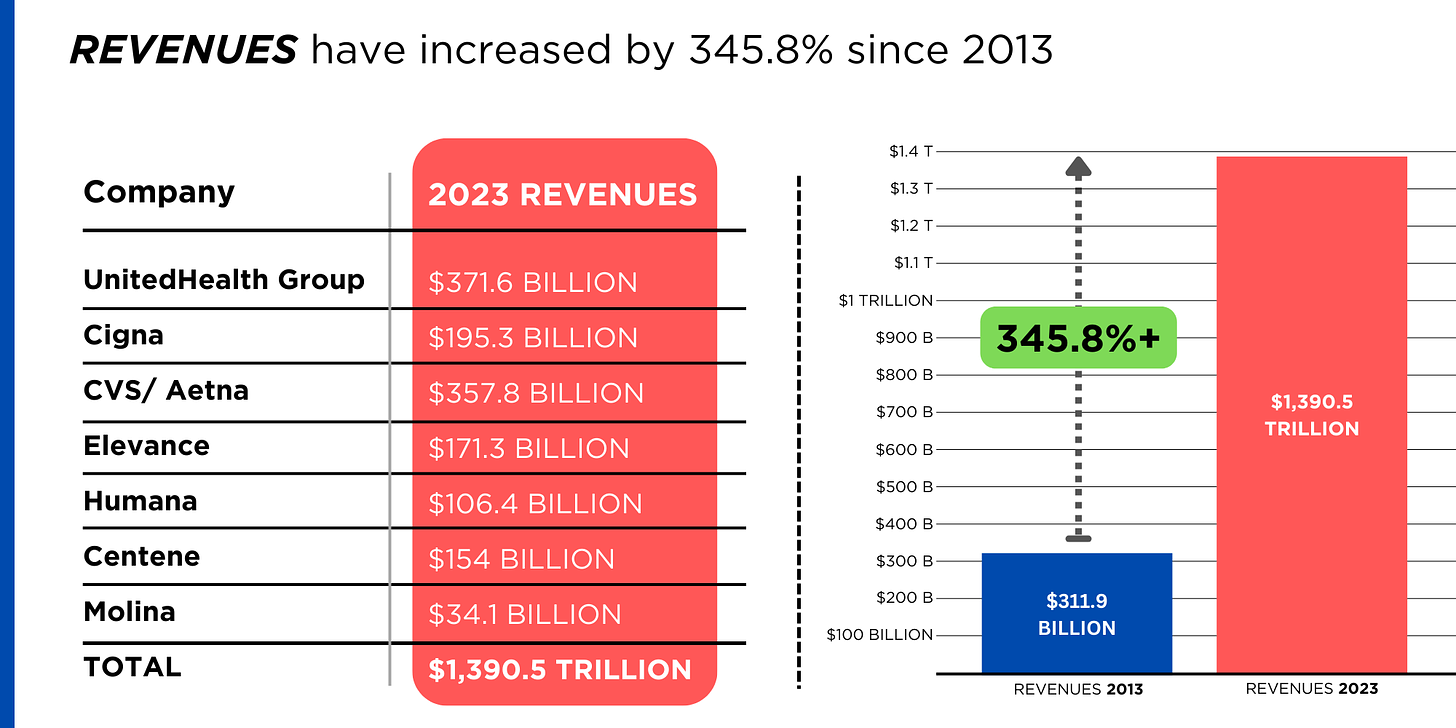
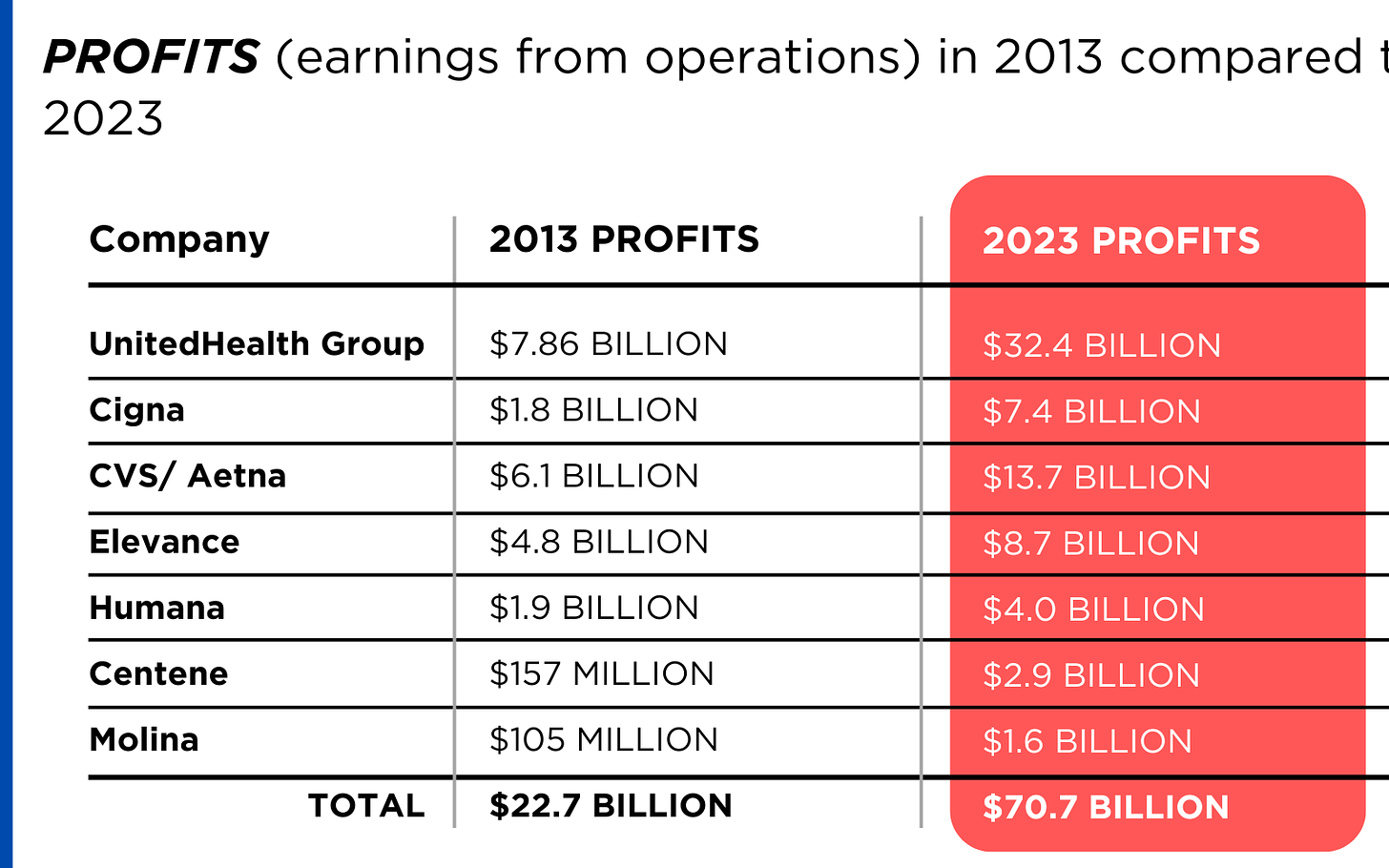
I wrote Monday about how the additional Medicare claims CVS/Aetna paid during the first three months of this year prompted a massive selloff of the company’s shares, sending the stock price to a 15-year low.
During CVS’s May 1 call with investors, CEO Karen Lynch and CFO Thomas Cowhey assured them the company had already begun taking action to avoid paying more for care in the future than Wall Street found acceptable.
Among the solutions they mentioned:
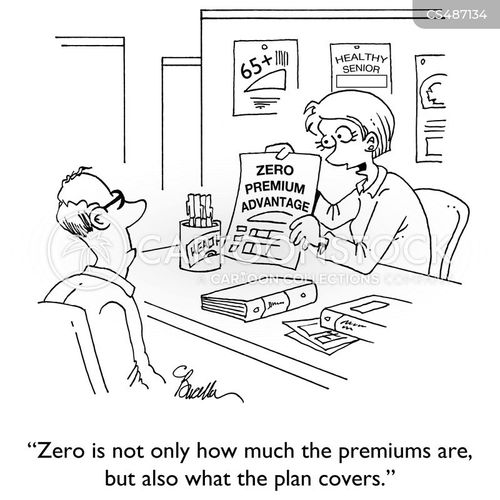
Ratcheting up the process called prior authorization that results in delays and denials of coverage requests from physicians and hospitals; kicking doctors and hospitals out of its provider networks; hiking premiums; slashing benefits; and abandoning neighborhoods where the company can’t make as much money as investors demand.
On Tuesday at the Bank of America Securities Healthcare Conference, Cowhey doubled down on that commitment to shareholders and provided a little more color about what those actions would look like and how many human beings would be affected. As Modern Healthcare reported:
Headed into next year, Aetna may adjust benefits, tighten its prior authorization policies, reassess its provider networks and exit markets, CVS Chief Financial Officer Tom Cowhey told investors. It will also reevaluate vision, dental, flexible spending cards, fitness and transportation benefits, he said. Aetna is also working with its employer Medicare Advantage customers on how to appropriately price their business, he said.
Could we lose up to 10% of our existing Medicare members next year? That’s entirely possible, and that’s OK because we need to get this business back on track,” Cowhey said.
Insurers use the word “members” to refer to people enrolled in their health plans. You can apply for “membership” and pay your dues (premiums), but insurers ultimately decide whether you can stay in their clubs. If they think you’re making too many trips to the club’s buffet or selecting the most expensive items, your membership can–and will–be revoked.
That mention of “employer Medicare Advantage customers” stood out to me and should be of concern to people like New York Mayor Eric Adams, who was sold on the promise that the city could save millions by forcing municipal retirees out of traditional Medicare and into an Aetna Medicare Advantage plan. A significant percentage of Aetna’s Medicare Advantage “membership” includes people who retired from employers that cut a deal with Aetna and other insurers to provide retirees with access to care. Despite ongoing protests from thousands of city retirees, Adams has pressed ahead with the forced migration of retirees to Aetna’s club. He and the city’s taxpayers will find out soon that Aetna will insist on renegotiating the deal.
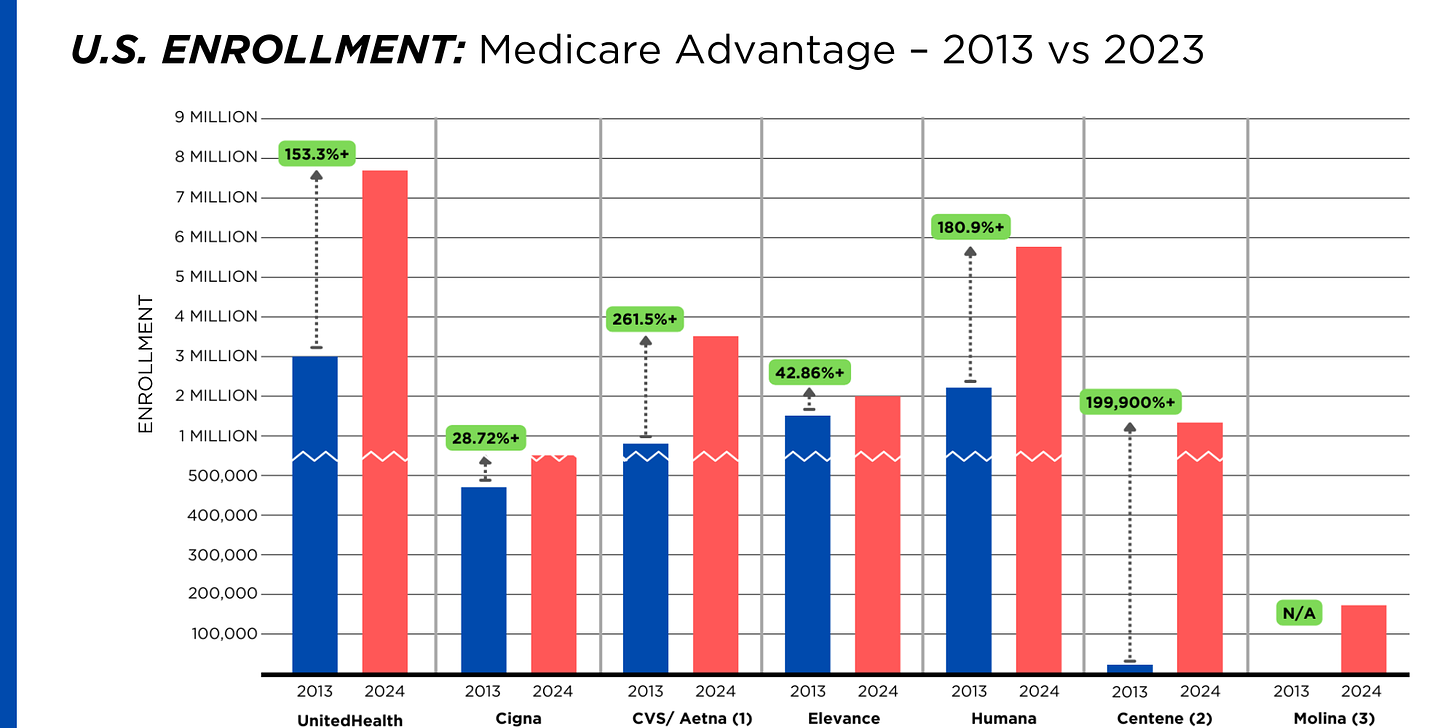
Back to that 10%. Aetna now has about 4.2 million Medicare Advantage “members,” but it has decided that around 420,000 of those human beings must be cut loose. Keep in mind that those humans are not among the most Internet-savvy and knowledgeable of the bewildering world of health insurance. Many of them have physical and mental impairments. They will be cast to the other wolves in the Medicare Advantage business.
Welcome to a world in which Wall Street increasingly calls the shots and decides which health insurance clubs you can apply to and whether those clubs will allow you to get the tests, treatments and medications you need to see another sunrise.
As Modern Healthcare noted, Aetna is not alone in tightening the screws on its Medicare Advantage members and setting many of them adrift. Humana, which has also greatly disappointed Wall Street because of higher-than-expected health care “utilization,” told investors it would be taking the same actions as Aetna.
But Aetna in particular has a history of ruthlessly cutting ties with humans who become a drain on profits. As I wrote in Deadly Spin in 2010:
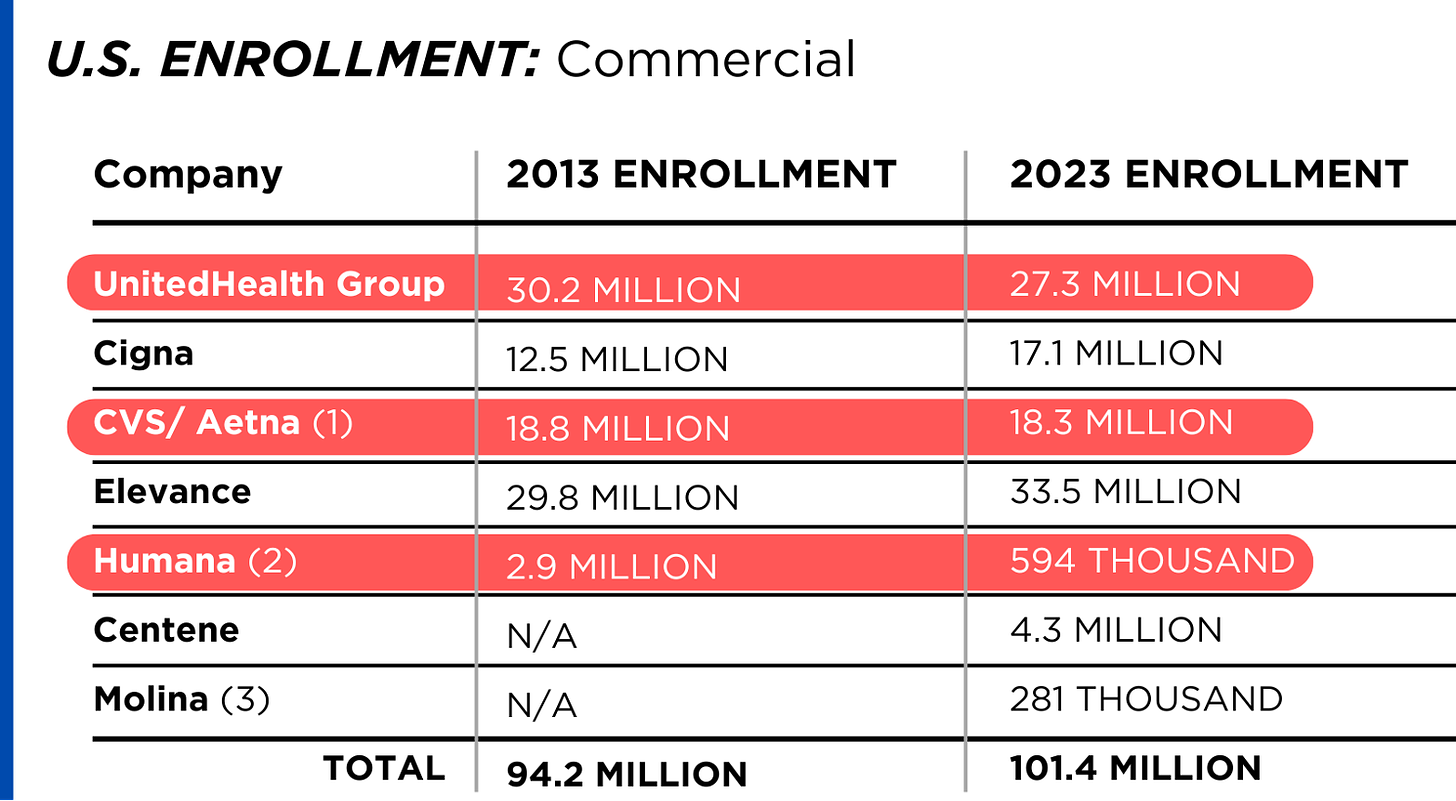
Aetna was so aggressive in getting rid of accounts it no longer wanted after a string of acquisitions in the 1990s that it shed 8 million (yes, 8 million) enrollees over the course of a few years. The Wall Street Journal reported in 2004 that Aetna had spent more than $20 million to install new technology that enabled it “to identify and dump unprofitable corporate accounts.” Aetna’s investors rewarded the company by running up the stock price.
I added this later in the book:
One of my responsibilities at Cigna was to handle the communication of financial updates to the media, so I knew just how important it was for insurers not to disappoint investors with a rising MLR [medical loss ratio, the ratio of paid claims to revenues]. Even very profitable insurers can see sharp declines in their stock prices after admitting that they had failed to trim medical expenses as much as investors expected. Aetna’s stock price once fell more than 20% in a single day after executives disclosed that the company had spent slightly more on medical claims during the most recent quarter than in a previous period. The “sell alarm” was sounded when the company’s first quarter MLR increased to 79.4% from 77.9% the previous year.
I could always tell how busy my day was going to be when Cigna announced earnings by looking at the MLR numbers. If shareholders were disappointed, the stock price would almost certainly drop, and my phone would ring constantly with financial reporters wanting to know what went wrong.
May 1 was a deja-vu-all-over-again day for Aetna. You can be certain the company’s flacks had a terrible day–but not as terrible as the day coming soon for Aetna’s members when they try to use their membership cards.
Speaking of Lynch, one of the people commenting on the piece I wrote Monday suggested I might have been a bit too tough on Lynch, who I know and liked as a human being when we both worked at Cigna. The commenter wrote that:
After finishing Karen S. Lynch’s book, “Taking Up Space,” I came to the conclusion that she indeed has a very strong conscience and sense of responsibility, not totally to shareholders, but more importantly to the insured people under Aetna and the customers of CVS.”
I don’t doubt Karen Lynch is a good person, and I know she is someone whose rise to become arguably the business world’s most powerful woman was anything but easy, as the magazine for alumni of Boston College, her alma mater, noted in a profile of her last year. Quoting from a speech she delivered to CVS employees a few years earlier, Daniel McGinn wrote:
Lynch began with a story to illustrate why she was so passionate about health care. She described how she’d grown up on Cape Cod as the third of four children. Her parents’ relationship broke up when she was very young and her father disappeared, leaving her mom, Irene, a nurse who struggled with depression, as a single parent. In 1975, when Lynch was 12, Irene took her own life, leaving the four children effectively orphaned.
During her speech, several thousand employees listened in stunned silence as Lynch explained how her mom’s life might have turned out differently if she’d had access to better medical treatment, or if there’d been less stigma and shame about getting help for depression. She then talked about how an insurance company like Aetna could play a role in reducing that stigma, increasing access to care, and helping people live with mental illness.
I’m sure when she goes home at night these days, Lynch worries about what will happen to those 420,000 other humans who will soon be scrambling to get the care they need or to find another club that will take them. Their lives most definitely will turn out differently to appease the rich people who control her and the rest of us.
But she is stuck in a job whose real bosses–investors and Wall Street financial analysts–care far more about the MLR, earnings per share and profit margins than the fate of human beings less fortunate than they are.