https://www.beckershospitalreview.com/hospital-management-administration/decision-making-amid-covid-19-6-takeaways-from-health-system-ceos-and-cfos.html?utm_medium=email

Alignment between CEOs and CFOs has become even more essential during the pandemic.
Many health systems halted elective surgeries earlier this year at the height of the pandemic to conserve resources while caring for COVID-19 patients. Now, in many areas, those procedures are returning and hospitals are slowly resuming more normal operations. But damage has been done to the hospital’s bottom line. Moving forward, the relationship between top executives will be crucial to make the right decisions for patients and the overall health of their organizations.
During the Becker’s Healthcare CEO+CFO Virtual Forum on Aug. 11, CEOs and CFOs for top hospitals and health systems gathered virtually to share insights and strategies as well as discuss the biggest challenges ahead for their institutions. Click here to view the panels on-demand.
Here are six takeaways from the event:
1. The three keys to a strong CEO and CFO partnership are trust, transparency and communication.
2. It’s common for a health system CEO and CFO to have different priorities and different opinions about where investments should be made. To help come to an agreement, they should look at every decision as if it’s a decision being made by the organization as a whole and not an individual executive. For example, there are no decisions by the CFO. There are only decisions by the health system. The CFOs said it’s important to remember that the patient comes first and that health systems don’t exist to make money.
3. Technology has of course been paramount during the pandemic in terms of telehealth. But so are nontraditional partnerships with other health systems that have allowed providers to share research and education.
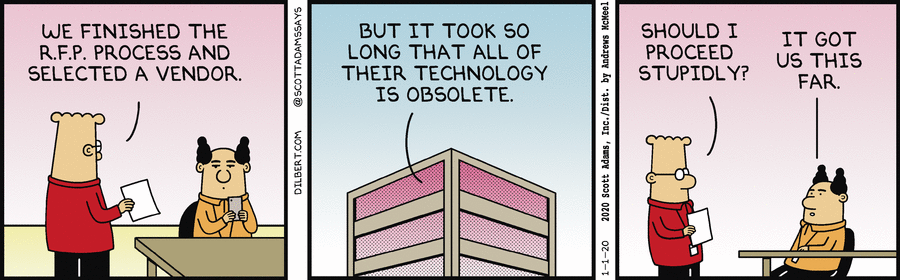
4. When it comes to evaluating technology, there’s a difference between being on the cutting edge versus the bleeding edge. Investing in new technology requires firm exit strategies. If warning signs show an investment is not going to give the return a health system hoped for, they need to let go of ideals and stick to the exit strategy.
5. Communication and transparency with staff and the public is key while making challenging decisions. Many hard decisions, including furloughs or personnel reductions, were made this spring to protect the financial viability of healthcare organizations. These decisions, which were not made lightly, were critiqued highly by the public. One of the best ways to ensure the message was not getting lost in translation and to help navigate the criticism included creating a communication plan and sharing that with employees, physicians and the public.
6. The pandemic required hospitals to think on their feet and innovate quickly. Many of the usual ways to solve a problem could not be used during that time. For example, large systems had to rethink how to acquire personal protective gear. Typically, in a large health system amid a disaster, when a supply item is running low, organizations can call up another hospital in the network and ask them to send some supplies. However, everyone in the pandemic was running low on the same items, which required innovation and problem-solving that is outside of the norm.