https://www.kaufmanhall.com/insights/blog/financial-literacy-leadership-prerequisite

In last month’s blog, we discussed the importance of financial planning, both for internal audiences—including the leadership team and the board of trustees—and for external audiences—including prospective students and their families, rating agencies, alumni and other stakeholders. This month, in the first of a series of blogs focused on key finance-related issues, we’re turning our attention to a broader and deeper internal audience, asking the question, “What is your institution’s financial literacy?”
The terms described in this blog will be very familiar to members of college and university finance teams and to many institutional leaders as well.
The point is that these terms should be familiar to as many individuals as possible throughout the institution: they form the foundation of a basic financial literacy that every college and university should foster across its faculty and staff.
What is financial literacy?
Financial literacy is the ability to understand where an institution stands at any given time with respect to key elements of its balance sheet and income statement. To state it simply, financial literacy means an understanding of the vital signs that describe the financial health of the institution. In medicine, the basic vital signs are body temperature, pulse rate, respiration rate, and blood pressure. In finance, the vital signs include measures of unrestricted cash, revenue, expenses, debt, and risk.
In medicine, there are professionals whose job is to dig deeper if any of the body’s vital signs are deteriorating. Similarly in finance, it is the job of the CFO and finance team to monitor the vital signs of the institution’s financial health and to seek causes and solutions of current troubles or to use changes in the vital signs to address potential future issues. For most of us—in medicine or finance—the goal should be a basic understanding of what the vital signs measure and whether they point to good health.
There are some key considerations for each financial vital sign:
- Unrestricted Cash. The critical question related to unrestricted cash (also termed liquidity) is whether the institution has enough accessible liquidity to meet its daily expenses if its cash flow was unexpectedly interrupted. Days cash on hand is a balance sheet metric that is typically used to assess this issue: days cash on hand literally measures how long unrestricted cash reserves could cover the institution’s operating costs if its cash flow suddenly stopped.
The emphasis on “accessible liquidity” is an important element of this financial vital sign: it speaks to the ability to distinguish between institutional wealth versus liquidity. In higher education, an endowment can be an important source of the institution’s wealth, but many of the funds within an endowment cannot be easily accessed—they are, by and large, not liquid funds or are highly restricted as to their use. Readily available, unrestricted cash reserves are what an institution must rely on to meet its day-to-day expenses should cash flow be interrupted or reduced.
- Revenue. Because an institution needs to maintain or grow its cash reserves and allocate them sparingly, the amount of revenue coming in—from tuition and fees and from other sources of additional income (see below)—is also an important vital sign. An institution should obviously be taking in enough revenue to cover its expenses without drawing on its cash reserves.
Additionally, however, given continued growth in expenses, revenue growth (through enrollment growth, student mix, and/or program mix) is a significant measure of ongoing vitality.
Financial health is also enhanced if an institution does not rely too heavily on a single revenue source. For schools with an endowment, for example, the amount of income the endowment can generate to support operations is an important source of additional income. More generally, additional income can come from such auxiliary revenue sources as residential fees, fundraising, special events, concessions, and a host of other sources. These additional revenue sources, while potentially small on an individual basis, can be material on a cumulative basis.
- Expenses. How much does it cost to produce the education that a college or university provides to its students? If that cost is approaching—or worse, surpassing—the net tuition revenue and additional income that the institution brings in, what is being done—or could be done—to reduce those costs? Expenses are perhaps most similar to body temperature in medical vital signs; if they get too high, they must be brought down before the health of the institution begins to decline. And the measure of expenses should be viewed overall for the institution as well as on a per student basis to communicate the “value” of different student types to the organization.
- Debt. Debt is an essential component of the funding of significant capital projects that colleges and universities must undertake to maintain updated and competitive facilities. Just as most people need to take out a mortgage to afford a home purchase—spreading the cost of the home over a multiyear payment period—so too do institutions often need debt to finance large capital expenditures. But the amount of debt (also termed “leverage”) can also be an indicator of the institution’s financial health. That health begins to decline if the amount of debt relative to an institution’s assets or annual income grows too large, or if the amount required to pay for the debt (i.e., to meet the scheduled principal and interest payments—the debt service) puts too much of a burden on the cash flow generated from the institution’s day-to-day operations. If the debt service becomes too high relative to cash flow, the institution may face onerous legal requirements, or even default, which may severely constrain its ability to provide the range of programs desired and expected by its student population.
- Risk. Risk is an indicator that identifies potential weaknesses in any of the preceding indicators that could jeopardize the institution’s financial health. For basic financial literacy, only the most significant risks need to be identified: over-reliance on tuition revenue in a market with declining enrollments, for example, or over-reliance on endowment income in the event of market instability. Once an institution consistently measures its risks, it can begin to determine what level of risk is appropriate and address strategies to manage that risk.
Why does financial literacy matter?
Promoting financial literacy throughout an institution cultivates a common understanding of financial health that provides context for leadership’s decisions and a common language to address issues. If tuition revenue is declining, for example, financially literate faculty members should better understand the need to prioritize academic programs that not only meet the academic needs of their students, but also can draw more students or produce healthier margins. If cost-cutting measures are required to reduce expenses, financially literate staff should understand the genesis of the need for reductions and why the institution cannot simply draw on its endowment to close the gap. Furthermore, acknowledging and describing the most significant risks an institution faces using a common language makes clear the need for action if one or more of those risks begins to materialize.
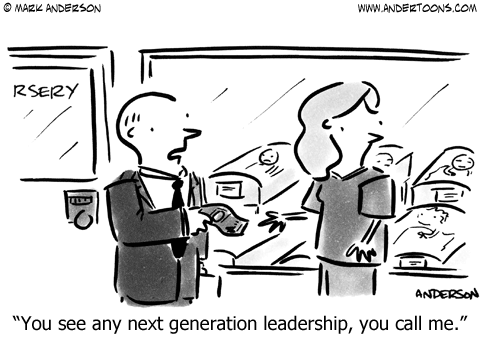
Financial literacy is also an important tool for cultivating the next generation of faculty leaders. When faculty members rise to leadership positions, it is essential that they understand that academic growth and strategic initiatives cannot succeed without sufficient resources to support them, or if they cannot generate the revenue needed to cover—or exceed—their costs.
By promoting financial literacy across the institution, the institution can help ensure that future leaders are acquiring the foundation needed for them to grow into informed decision-makers who understand the need to maintain the institution’s financial health.