Health systems are rightly concerned about Republican plans to cut Medicaid spending, end ACA subsidies and enact site neutral payments, says consultant Michael Abrams, managing partner of Numerof, a consulting firm.
“Health systems have reason to worry,” Abrams said shortly after President Donald Trump was inaugurated on Monday.
While Trump mentioned little about healthcare in his inauguration speech, the GOP trifecta means spending cuts outlined in a one-page document released by Politico and another 50-pager could get a majority vote for passage.
Of the insurers, pharmaceutical manufacturers and health systems that Abrams consults with, healthcare systems are the ones that are most concerned, Abrams said.
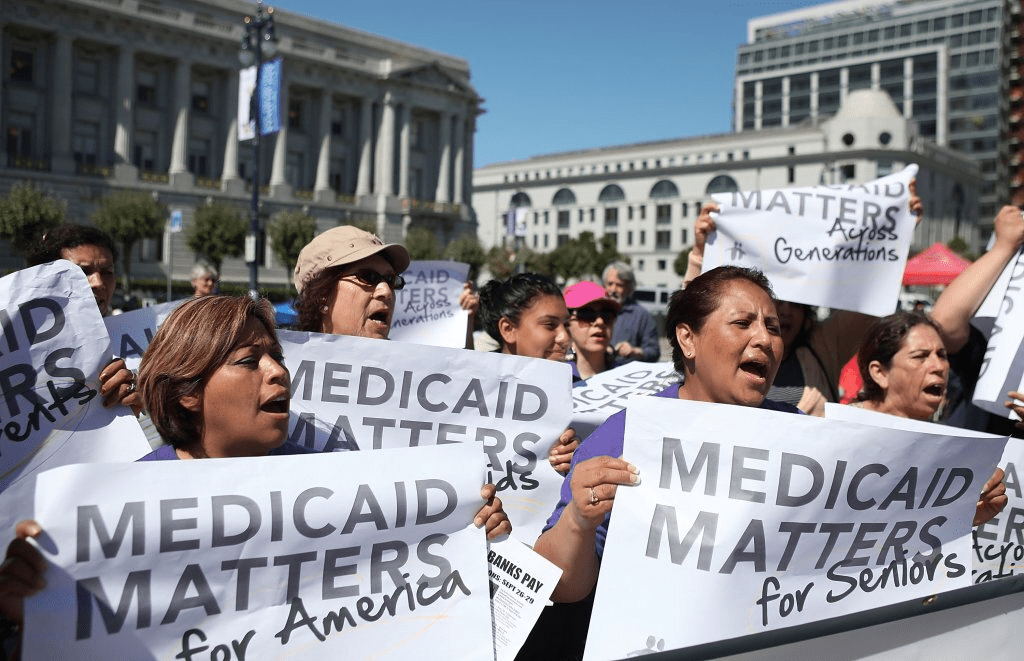
At the top of the Republican list targeting $4 trillion in healthcare spending is eliminating an estimated $2.5 billion from Medicaid.
“There’s no question Republicans will find savings in Medicaid,” Abrams said.
Medicaid has doubled its enrollment in the last couple of years due to extended benefits made possible by the Affordable Care Act, despite disenrolling 25 million people during the redetermination process at the end of the public health emergency, according to Abrams.
Upward of 44 million people, or 16.4% of the non-elderly U.S. population are covered by an Affordable Care Act initiative, including a record high of 24 million people in ACA health plans and another 21.3 million in Medicaid expansion enrollment, according to a KFF report. Medicaid expansion enrollment is 41% higher than in 2020.
The enhanced subsidies that expanded eligibility for Medicaid and doubled the number of enrollees are set to expire at the end of 2025 and Republicans are likely to let that happen, Abrams said. Eliminating enhanced federal payments to states that expanded Medicaid under the ACA are estimated to cut the program by $561 billion.
If enhanced subsidies end, the Congressional Budget Office has estimated that the number of people who will become uninsured will increase by 3.8 million each year between 2026 and 2034.
The enhanced tax subsidies for the ACA are set to expire at the end of 2025. This could result in another 2.2 million people losing coverage in 2026, and 3.7 million in 2027, according to the CBO.
WHY THIS MATTERS
For hospitals, loss of health insurance coverage means an increase in sicker, uninsured patients visiting the emergency department and more uncompensated care.
“Health systems are nervous about people coming to them who are uninsured,” Abrams said. “There will be people disenrolled.”
The federal government allowed more people to be added to the Medicaid rolls during the public health emergency to help those who lost their jobs during the COVID-19 pandemic, Numerof said. Medicaid became an open-ended liability which the government wants to end now that the unemployment rate is around 4.2% and jobs are available.
An idea floating around Congress is the idea of converting Medicaid to a per capita cap and providing these funds to the states as a block grant, Abrams said. The cost of those programs would be borne 70% by the federal government and 30% by states.
This fixed amount based on a per person amount would save money over the current system of letting states report what they spent.
Another potential change under the new administration includes site neutral Medicare payments to hospitals for outpatient services.
The HFMA reported the site neutral policy as a concern in a list it published Monday of preliminary federal program cuts totaling more than $5 trillion over 10 years. The 50-page federal list is essentially a menu of options, the HFMA said, not an indication that programs will actually be targeted leading up to the March 14 deadline to pass legislation before federal funding expires.
Other financial concerns for hospitals based on that list include: the elimination of the tax exemption for nonprofit hospitals, bringing in up to $260 billion in estimated 10-year savings; and phasing out Medicare payments for bad debt, resulting in savings of up to $42 billion over a decade.
Healthcare systems are the ones most concerned over GOP spending cuts, according to Abrams. Pharmacy benefit managers and pharmaceutical manufacturers also remain on edge as to what might be coming at them next.
THE LARGER TREND
President Donald Trump mentioned little about healthcare during his inauguration speech on Monday.
Trump said the public health system does not deliver in times of disaster, referring to the hurricanes in North Carolina and other areas and to the fires in Los Angeles.
Trump also mentioned giving back pay to service members who objected to getting the COVID-19 vaccine.
He also talked about ending the chronic disease epidemic, without giving specifics.
“He didn’t really talk about healthcare even in the campaign,” Abrams said.
However, in his consulting work, Abrams said, “The common thread is the environment is changing quickly,” and that healthcare organizations need to do the same “in order to survive.”