Medicare Advantage is in an awkward place.
On the one hand, the alternative to traditional Medicare is still popular among consumers, who have been lured by the promises of lower out-of-pocket costs and increased supplemental benefits.
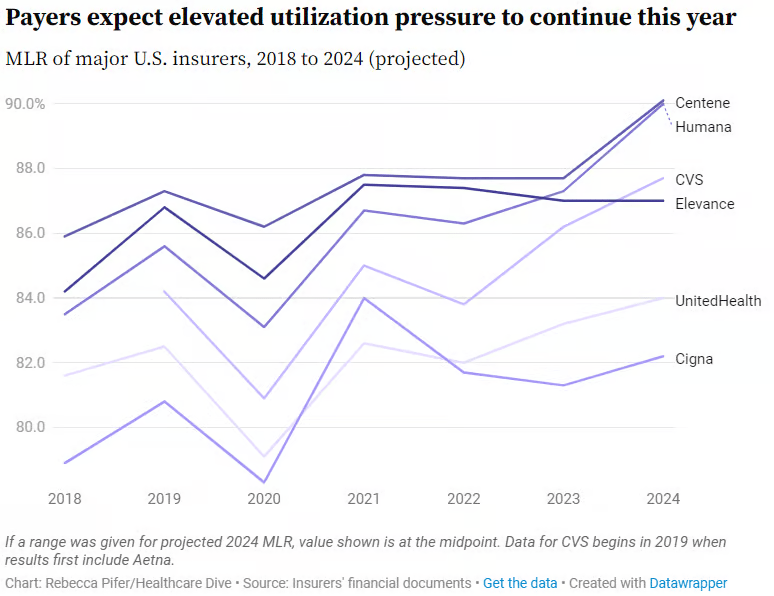
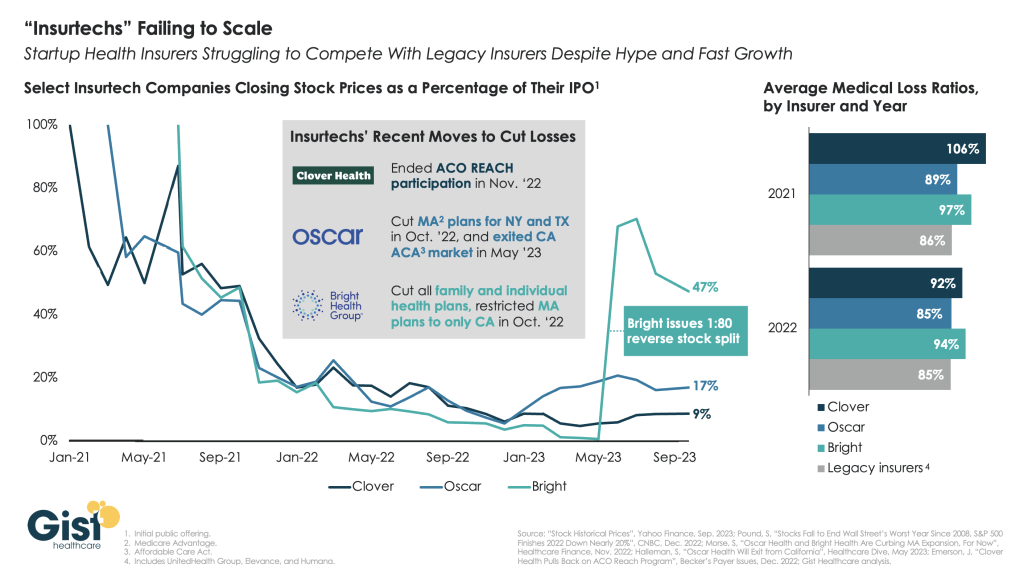
On the other hand, Medicare Advantage profitability is on the decline, as shown in recent quarterly reports from the large insurers. The headwinds, executives said during recent earnings calls, have been due to greater than expected utilization of benefits and lower than expected reimbursement from the government.
Adding to MA’s margin challenges are providers who are making the decision to cut their ties with MA plans rather than deal with delays in prior authorization and claims payments.
Moody’s Investors Service said this year, and an HFMA survey from March indicates 19% of health systems have discontinued at least one Medicare Advantage plan, while 61% are planning to or considering dropping Medicare Advantage payers.
Until recently, the story of Medicare Advantage was one of ascendancy. Just last year it hit a milestone: More than half of eligible Medicare beneficiaries are now in MA plans. So why is business taking a step back?
WHY THIS MATTERS
There are many factors at play, but a big one is the 3.7% rate increase for 2025 that Medicare Advantage plans will receive from the Centers for Medicare and Medicaid Services. The federal government is projected to pay between $500 and $600 billion in Medicare Advantage payments to private health plans, according to the 2025 Advance Notice for the Medicare Advantage and Medicare Part D Prescription Drug Programs released in April.
The payment rate was considered inadequate by insurers, who were also troubled over other key factors, including a 0.16% reduction in the Medicare Advantage benchmark rate for 2025, which represents a 0.2% decrease.
“AHIP has strong concerns that the estimated growth rate in the Advance Notice – an average of 2.44% – will lead to benchmark changes that are insufficient to cover the cost of caring for 33 million MA beneficiaries in 2025,” AHIP president and CEO Mike Tuffin said in April. “The estimate does not reflect higher utilization and cost trends in the healthcare market that are expected to continue into 2025.”
According to Karen Iapoce, vice president Government Programs at ZeOmega, the cost of running an MA business is increasing due to the burdens being placed on health plans.
“If you sit inside with a health plan, they’re asked to do a lot with not as much bandwidth as they had before,” said Iapoce. “For example, health equity requires plans to have new regulatory guidance they need to meet. There’s a host of measures around health equity. Our plans are not in the business of really understanding how to manage transportation, how to manage housing, so they’re working with other entities. This requires an expert to sit in with the health plan … and then track and report. On the business end, they want to show an ROI, but that could be six months or a year down the line.”
Because of that, she said, the benchmark rate is likely insufficient to cover the projected increase in administrative and other costs. Iapoce said the benchmark rates represent the maximum amount that will be paid to a person in a given county; this is used as a reference point for calculation. If a plan is higher than the benchmarks, the premiums end up going to the beneficiary. More commonly, the plans bid below the benchmark, and the difference represents the rebate plans will receive. But they also factor into risk adjustment.
“The plans are getting into these contract negotiations, so they have to know what goes into that benchmark,” said Iapoce. “I might not be a high utilizer, but you may be. If we’re bringing in a community of high utilizers, there’s no one offsetting that. There’s no balance.”
Richard Gundling, senior vice president, content and professional practice guidance at HFMA, said MA plans started running into these issues when the program crossed over the threshold of more than 50% of beneficiaries.
“When a Medicare Advantage plan comes in, then all the extra administrative burdens come into play,” said Gundling. “So you have prior authorizations, all the issues around lack of payment and denials. Patients get caught in the middle, and in particular elderly patients think they’re still on traditional Medicare.
“It used to be that healthier beneficiaries went into Medicare Advantage,” he added. “Sicker beneficiaries tended to stay in traditional Medicare. That’s not the case anymore, and so there’s a higher spend.”
Gundling said beneficiaries are likely flocking to MA with visions of lower costs and increased benefits such as eyeglasses and hearing aids, and many don’t realize the tradeoffs, such as prior authorizations and network restrictions.
MA remains popular with seniors, but studies show the plans cost the government more money than original Medicare.
A 2023 Milliman report showed annual estimated healthcare costs per beneficiary are $3,138, compared to $5,000 for traditional fee-for-service Medicare, and over $5,700 if a traditional Medicare beneficiary also buys a Medigap plan.
MA membership has grown nationally at an annual rate of 8% to approximately 32 million, while traditional Medicare has declined at an average annual rate of 1%. As that has happened the percentage of people choosing MA has grown to 49% from 28%, data shows.
Yet Medicare Advantage profitability is on the decline, Moody’s found in February. That’s largely because of a significant spike in utilization for most of the companies, which Moody’s expects will result in lower full-year MA earnings for insurers. Adding to that is lower reimbursement rates for the first time in years that are likely to remain weaker in 2025 and 2026, which is credit negative.
Moody’s analysts contend that MA may have “lost its luster,” citing as evidence Cigna’s efforts to sell its MA business, even after a failed merger with Humana. Cigna this past winter announced it had entered into a definitive agreement to sell its Medicare Advantage, Supplemental Benefits, Medicare Part D and CareAllies businesses to Health Care Service Corporation (HCSC) for about $3.7 billion.
Iapoce said Medicare Advantage may be a victim of its own success.
“Because of all this great promotion about what a Medicare Advantage plan can do for you, you’re seeing an increase in enrollment, or more people moving over, and the demographics are starting to change,” she said.
For many consumers, the appeal of an MA plan is the same as that of an online retailer like Amazon, said Iapoce. Such retailers offer one-stop shopping for a variety of goods, and the perception is that MA essentially offers one-stop shopping for a variety of healthcare services and benefits.
But while this massive shift is happening, it puts providers in an awkward position, said Iapoce.
“Their reimbursement is almost being dictated, in essence, by a health plan,” she said. “It almost feels like the payer has the upper hand over the provider. Think: I’m a provider. It’s my job to get this female with this particular age and condition a mammogram, and the health plan has told me to get her a mammogram. But you, as the health plan, get the money for it. I, as the provider … what am I getting? What’s it doing for me? It becomes this very tense situation, and the provider is probably the entity that is running on the thinnest of staff.”
Gundling expects that despite some “growing pains,” MA will remain viable and continue to grow.
“Nobody’s going to stay still,” said Gundling. CMS has to consider, ‘Are we paying the health plans appropriately for the types of patients they have?’ And then health plans will need to look at their medical utilization rules – ‘Are we overdoing pre-authorization or denying things appropriately?’ And providers need to say, ‘This is a market we need to continue to grow.’
“There’s still going to be a role for it,” he said. “It’s just that we’ve introduced a larger population into it, and I think that’s where a lot of the surprises come in.”
THE LARGER TREND
CVS reported earlier this month that healthcare-benefits medical costs, primarily due to higher-than-expected Medicare Advantage utilization, came in approximately $900 million above expectations.
Last month, Humana said it expected membership may take a hit from future Medicare Advantage pricing resulting from the CMS payment rate notice. Humana is actively evaluating plan level pricing decisions and the expected impact to membership, president and COO James Rechtin said on the call.
Elevance Health, formerly Anthem, reported a 12.2% earnings increase for Q1, but company margins have not been as affected as those insurers that are heavily invested in the MA market. Fewer of its members are in MA plans compared to other large insurers Humana, CVS Health or UnitedHealth Group, executives said.