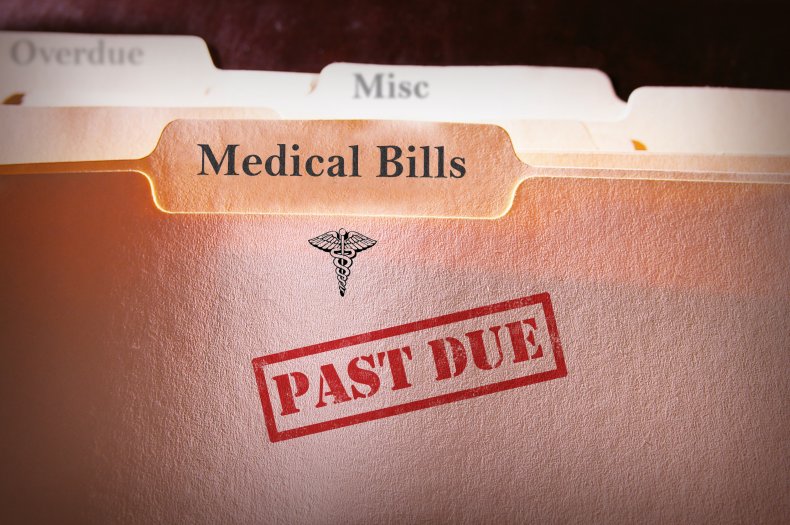
About 73% of health insurance markets are highly concentrated, and in 46% of markets, one insurer had a share of 50% or more, a new report from the American Medical Association shows. The report comes a few months after President Joe Biden directed federal agencies to ramp up oversight of healthcare consolidation.
The majority of health insurance markets in the U.S. are highly concentrated, curbing competition, according to a report released by the American Medical Association.
For the report, researchers reviewed market share and market concentration data for the 50 states and District of Columbia, and each of the 384 metropolitan statistical areas in the country.
They found that 73% of the metropolitan statistical area-level payer markets were highly concentrated in 2020. In 91% of markets, at least one insurer had a market share of 30%, and in 46% of markets, one insurer had a share of 50% or more.
Further, the share of markets that are highly concentrated rose from 71% in 2014 to 73% last year. Of those markets that were not highly concentrated in 2014, 26% experienced an increase large enough to enter the category by 2020.
In terms of national-level market shares of the 10 largest U.S. health insurers, UnitedHealth Group comes out on top with the largest market share in both 2014 and 2020, reporting 16% and 15% market share, respectively. Anthem comes in second with shares of 13% in 2014 and 12% in 2020.
But the picture looks different when it comes to the market share of health insurers participating in the Affordable Care Act individual exchanges. In 2014, Anthem held the largest market share among the top 10 insurers on the exchanges, with a share of 14%. By 2020, Centene had taken the top spot, with a share of 18%, while Anthem had slipped to fifth place, with a share of just 4%.
Another key entrant into the top 10 list in 2020 was insurance technology company Oscar Health, with 3% of the market share in the exchanges at the national level.
“These [concentrated] markets are ripe for the exercise of health insurer market power, which harms consumers and providers of care,” the report authors wrote. “Our findings should prompt federal and state antitrust authorities to vigorously examine the competitive effects of proposed mergers involving health insurers.”
The payer industry hit back. In a statement provided to MedCity News, America’s Health Insurance Plans, a national payer association, said that Americans have many affordable choices for their coverage, pointing to the fact that CMS announced average premiums for Medicare Advantage plans will drop to $19 per month in 2022 from $21.22 this year.
“Health insurance providers are an advocate for Americans, fighting for lower prices and more choices for them,” said Kristine Grow, senior vice president of communications at America’s Health Insurance Plans, in an email. “We negotiate lower prices with doctors, hospitals and drug companies, and consumers benefit from lower premiums as a result.”
Further, the report does not mention the provider consolidation that also contributes to higher healthcare prices. Mergers and acquisitions among hospitals and health systems have continued steadily over the past decade, remaining relatively impervious to even the Covid-19 pandemic.
Scrutiny around consolidation in the healthcare industry may grow. In July, President Joe Biden issued an executive order urging federal agencies to review and revise their merger guidelines through the lens of preventing patient harm.
The Federal Trade Commission has already said that healthcare businesses will be one of its priority targets for antitrust enforcement actions.