
New Ulm Medical Center struck a deal with a local payer willing to share the cost of a simple intervention. The arrangement has been paying dividends for seven years.
KEY TAKEAWAYS
The intervention slashed PMPM billing by 61% in three years for a small cohort of plan members.
What makes this program atypical is the way the hospital took a broad problem-solving approach while minimizing its expenses.
Patients who use the emergency department at least three times within four months at Allina Health’s New Ulm Medical Center in New Ulm, Minnesota, have their names added to a high-utilization list.
The keeper of that list is Jennifer Eckstein, a licensed social worker who follows up with each patient directly, looking to solve underlying problems that may be driving their frequent ED use. Whether the patients need a primary care physician, a mental healthcare provider, supportive housing, or another solution, Eckstein does her best to address their social determinants of health and steer them away from the ED for non-emergent care.
The intervention is a straightforward concept. Many other hospitals have similarly hired social workers to help meet the needs of these ED frequent flyers. The program at New Ulm Medical Center, in fact, was inspired in part by an earlier and narrower intervention that focused exclusively on mental health needs of ED patients at Allina’s Owatonna Hospital in Owatonna, Minnesota.
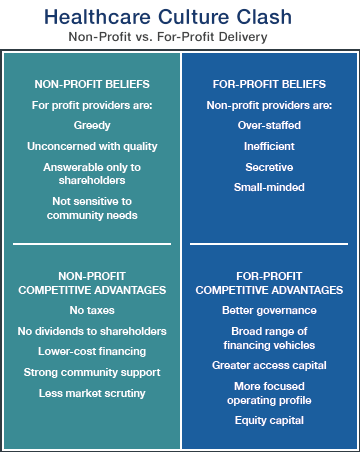
But what makes this program a bit different from others is the way New Ulm Medical Center took a broad problem-solving approach while minimizing its expenses. Rather than shouldering the full cost of employing a full-time ED social worker, the hospital partnered with local insurer South Country Health Alliance. They struck a deal and signed a contract agreeing to split the personnel expense 50/50, beginning in 2012.
Allina’s four hospitals in the Twin Cities metro area have regularly staffed social workers in their EDs, too, but none of them fund those positions through cost-sharing arrangements with health plans, according to a spokesperson for the nonprofit health system.
South Country Health Alliance CEO Leota Lind, who has been with the organization since its founding in 2000, says her organization didn’t need much convincing to sign the contract with New Ulm Medical Center. While unmet mental health needs are often a major factor contributing to ED overuse, they are far from the only factor, so the broader approach taken at New Ulm offered a chance to solve a wider range of the challenges that were leading plan members to an ED when they should be seeing a more cost-effective primary care physician instead, Lind says.
“We really just were looking at ways to influence and reduce emergency department visits,” Lind tells HealthLeaders. “By taking that broader scope, it gave us the opportunity to identify what other issues were contributing to that high utilization of the emergency department.”
FEWER DOLLARS, MORE SENSE
South Country Health Alliance and New Ulm Medical Center each contribute about $40,000 per year to cover Eckstein’s salary and benefits—which, at about $80,000 per year, are in line with what other hospital social workers earn in total compensation in the Midwest, says Carisa Buegler, MHA, director of operations for the hospital.
Both the hospital and payer say their shared investment has been paying off.
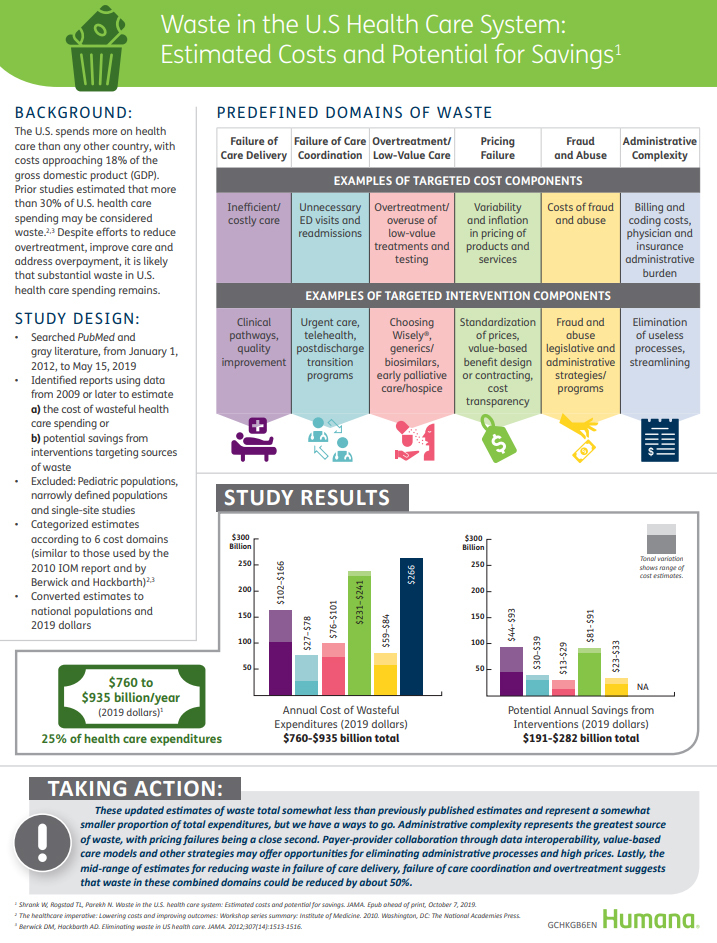
Before the social worker was introduced, a small cohort of 28 South Country Health Alliance plan members who received care in New Ulm Medical Center’s ED generated $731 per member per month (PMPM) in hospital bills, according to Buegler. A year after Eckstein began her work, in 2012, those bills fell to $416 PMPM, then they kept falling. By the end of the third year, in 2014, the 28-patient cohort generated $286 PMPM in bills, Buegler says.
That 61% reduction means the hospital billed the payer nearly $150,000 less in 2014—just for those 28 patients—than it had before the social worker was introduced. By the end of the third year, the cohort’s overall ED utilization was cut in half, and its inpatient admissions fell 89%, Buegler says.
That’s only part of the impact Eckstein’s labor has produced, since she doesn’t work exclusively with South Country plan members. Eckstein, who was hired into the position when it was created, says she helps roughly 150–200 patients per year, regardless of who’s paying for their care. Some needs are easier to meet than others, so she’s built a sense of rapport with some returning patients over the years.
“The good thing is they utilize me now instead of the ER, so when they get into a pickle or if they’re having trouble with something, they call me,” she says.
Across all payers, the intervention has likely been saving $500,000 or more, Buegler says.
The intervention is about more than just money, of course. It aims also to improve clinical care and patients’ quality of life.
“I don’t think the driver was necessarily just cost but appropriate care at the right place, at the right time, with the right kind of provider,” says South Country Health Alliance Chief Medical Officer Brad Johnson, MD.
But the financial implications of this intervention are especially interesting considering the fact that New Ulm Medical Center is spending $40,000 per year on a program that delivers cost-savings to payers while reducing the hospital’s revenue. The immediate financial benefit goes to the payer, not the provider.
The hospital has seen a 20% reduction in its overall ED volumes in the past five years, and that’s likely the direction in which most hospitals’ EDs are headed, which is generally good news, Buegler says. The situation presents a challenge, though, since value-based payment arrangements haven’t matured and proliferated to a point where they can compensate adequately for the trend, she says.
Why, then, would the hospital keep investing in this intervention?
“It’s the right thing to do,” Buegler says. “It’s providing the best level of care to our patients who are coming in the emergency department seeking help and then providing another level of service to those individuals to help them improve their social conditions, that will then help them to improve their health. … It’s really looking at the patient as a whole person.”
There’s also a longer-term business case to be made for the hospital’s continued investment, Buegler says.
“From a financial perspective, we’re preparing for more value-based payment contracts,” she says.
Although risk-based contracts have been arriving more slowly than many industry stakeholders had expected, leaders remain confident that more value-based models are on the way, so it makes sense for hospitals like New Ulm Medical Center to invest in the future it anticipates, Buegler says.
PLUGGED INTO SUPPORT NETWORK
Eckstein is the sole social worker stationed in the ED, but she’s not running a one-woman show.
New Ulm Medical Center has a social worker assigned to its clinic, too, and South Country Health Alliance employs a physician as a community care connector in each of the 11 counties it serves—so Eckstein has multiple partners just outside the ED’s walls.
“By having that hospital social worker work in partnership with the community care connector at the county, they’re able to effectively make referrals and access some of those other types of community supports that have also helped address the issues that individuals may be experiencing as barriers to managing their healthcare,” Lind says.
This idea of bridging the gap between traditional medical care and broader social services has been central to South Country Health Alliance’s mission since it was founded, Lind says.
“We recognized way back then that those other aspects, those other social, environmental aspects of an individual’s life, impact their ability to manage and maintain their healthcare,” she adds. “That’s been a part of our program since the beginning.”
Johnson says this care coordination is a vital component of the local safety net.
“In rural Minnesota,” he says, “there’s lots of opportunities for people that are not savvy users of the healthcare system to fall through the cracks.”
“THE GOOD THING IS THEY UTILIZE ME NOW INSTEAD OF THE ER, SO WHEN THEY GET INTO A PICKLE OR IF THEY’RE HAVING TROUBLE WITH SOMETHING, THEY CALL ME.”
JENNIFER ECKSTEIN, LICENSED SOCIAL WORKER












:format(webp)/cdn.vox-cdn.com/uploads/chorus_image/image/65358995/843175548.jpg.0.jpg)