https://www.axios.com/europe-lessons-reopening-schools-b713801e-26d6-4ba1-bb9e-c0b0b5809a11.html

American parents and policymakers hoping for a safe return to schools in the fall have been looking to Europe, where several countries reopened as early as April without a subsequent spike in cases.
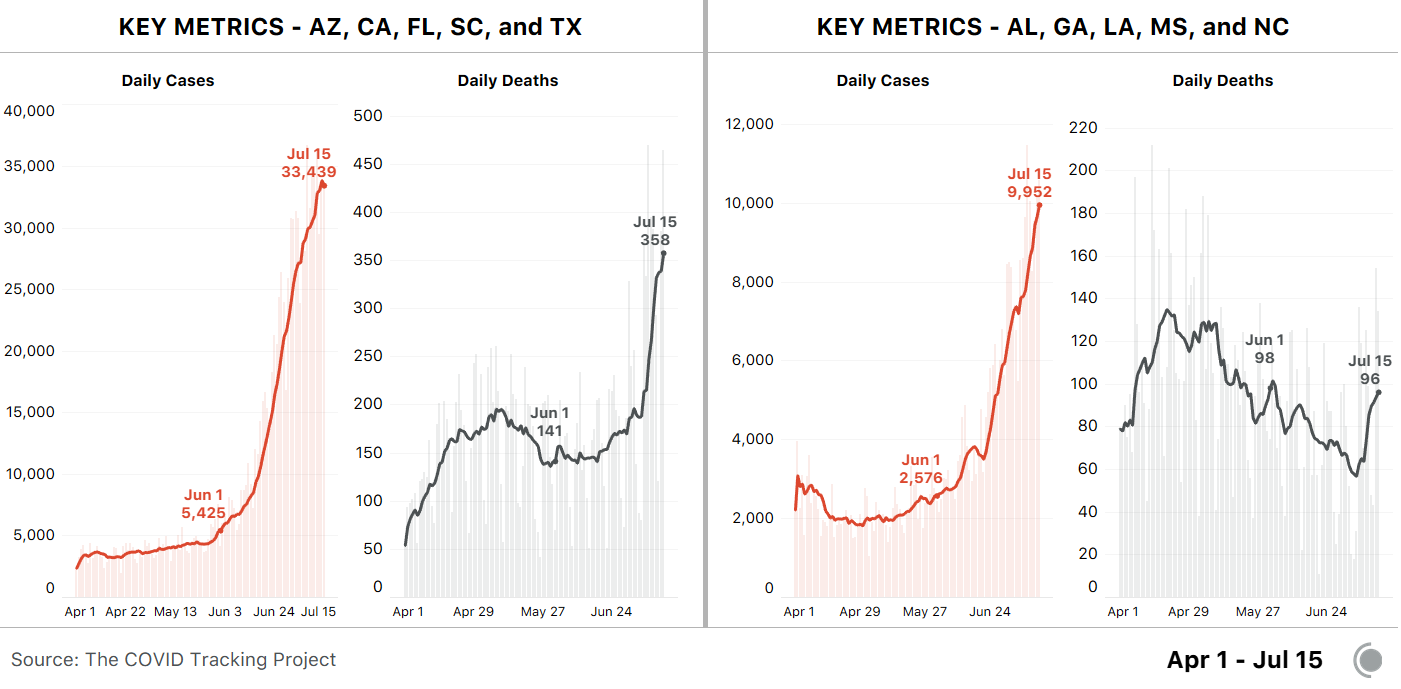
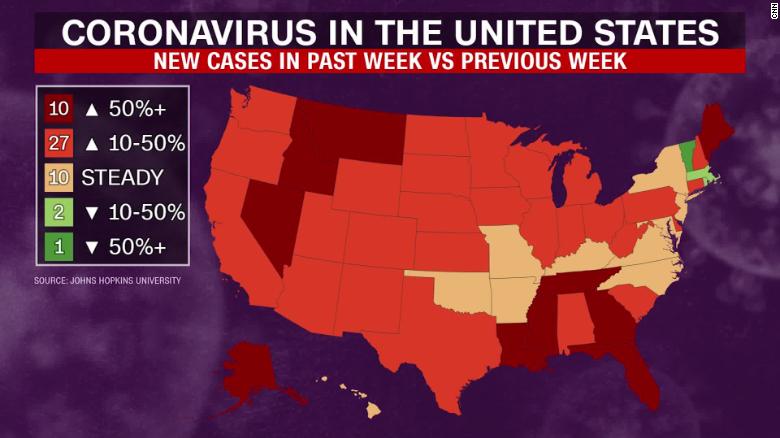
Why it matters: There’s a growing body of evidence suggesting that schools can operate safely, at least under certain circumstances. But no country that closed schools has attempted to reopen them with outbreaks still raging as they are across much of America.
- The first countries to bring students back, as Denmark did in April, didn’t detect much spread in schools — but the virus was also under control in the broader communities.
- Harder-hit countries, like France or Belgium, contained the spread through lockdowns before bringing students back — something the U.S. has largely failed to do.
- America’s unenviable position as a global epicenter complicates matters, but the challenge is similar: adapting schools to our pandemic reality.
Social distancing: Danish class sizes were initially limited to around 12, and arrival times were staggered to avoid crowding.
- As they plan for the fall, though, countries like Belgium are dropping distancing mandates for younger students, while France is trimming its spacing requirements from 4 meters (about 12 feet) to 1 (3 feet), per the Washington Post.
- That’s due to space limitations and the difficulties of keeping children apart, as well as indications that young students are unlikely to spread the virus to one another.
Masks: Similarly, countries including Austria initially required masks but loosened those restrictions over time.
- Masks are optional for both students and teachers in Denmark, Norway, the U.K. and Sweden, per Science. Some German schools force students to wear them in the hallway, but not in class.
- Masks are required for both students and teachers in several Asian countries, including China. Some experts argue that mask requirements would make reopening safer, particularly for teachers and older students.
“Bubbles”: When the U.K. fully reopens schools in September, smaller subsets of students will spend classes, lunch and recess together — an approach several other countries have experimented with.
- If a student gets the virus, the logic goes, there are only so many people they could give it to, or who would need to self-isolate.
- Italy is asking schools to open on Saturdays to allow for lower daily attendance, and schools are encouraged to hold classes outdoors or in larger venues like cinemas, per The Local. Funding has been allocated to update schools and hire more teachers.
Hybrid learning: Several countries have resumed in-person schooling on a more limited basis, supplemented by online education. School districts across the U.S. are designing such approaches now.
- Belgian students over 12 will attend school four days a week in the fall, with an additional half-day online. If cases increase, so will the proportion of online education.
What to watch: It remains unclear how susceptible children are to the virus, though findings from a hard-hit town in France — which are consistent with other evidence — suggest it spreads significantly less easily among teens than adults, and hardly at all among young children.
The bottom line: The risks to schools remain uncertain, but will almost certainly depend on what’s happening outside their walls.



.png)