
Cartoon – Drug Trial Results



Banks Pressure Health Care Firms to Raise Prices on Critical Drugs, Medical Supplies for Coronavirus

IN RECENT WEEKS, investment bankers have pressed health care companies on the front lines of fighting the novel coronavirus, including drug firms developing experimental treatments and medical supply firms, to consider ways that they can profit from the crisis.
The media has mostly focused on individuals who have taken advantage of the market for now-scarce medical and hygiene supplies to hoard masks and hand sanitizer and resell them at higher prices. But the largest voices in the health care industry stand to gain from billions of dollars in emergency spending on the pandemic, as do the bankers and investors who invest in health care companies.
Over the past few weeks, investment bankers have been candid on investor calls and during health care conferences about the opportunity to raise drug prices. In some cases, bankers received sharp rebukes from health care executives; in others, executives joked about using the attention on Covid-19 to dodge public pressure on the opioid crisis.
Gilead Sciences, the company producing remdesivir, the most promising drug to treat Covid-19 symptoms, is one such firm facing investor pressure.
Remdesivir is an antiviral that began development as a treatment for dengue, West Nile virus, and Zika, as well as MERS and SARS. The World Health Organization has said there is “only one drug right now that we think may have real efficacy in treating coronavirus symptoms” — namely, remdesivir.
The drug, though developed in partnership with the University of Alabama through a grant from the federal government’s National Institutes of Health, is patented by Gilead Sciences, a major pharmaceutical company based in California. The firm has faced sharp criticism in the past for its pricing practices. It previously charged $84,000 for a yearlong supply of its hepatitis C treatment, which was also developed with government research support. Remdesivir is estimated to produce a one-time revenue of $2.5 billion.
During an investor conference earlier this month, Phil Nadeau, managing director at investment bank Cowen & Co., quizzed Gilead Science executives over whether the firm had planned for a “commercial strategy for remdesivir” or could “create a business out of remdesivir.”
Johanna Mercier, executive vice president of Gilead, noted that the company is currently donating products and “manufacturing at risk and increasing our capacity” to do its best to find a solution to the pandemic. The company at the moment is focused, she said, primarily on “patient access” and “government access” for remdesivir.
“Commercial opportunity,” Mercier added, “might come if this becomes a seasonal disease or stockpiling comes into play, but that’s much later down the line.”
Steven Valiquette, a managing director at Barclays Investment Bank, last week peppered executives from Cardinal Health, a health care distributor of N95 masks, ventilators and pharmaceuticals, on whether the company would raise prices on a range of supplies.
Valiquette asked repeatedly about potential price increases on a variety of products. Could the company, he asked, “offset some of the risk of volume shortages” on the “pricing side”?
Michael Kaufmann, the chief executive of Cardinal Health, said that “so far, we’ve not seen any material price increases that I would say are related to the coronavirus yet.” Cardinal Health, Kaufman said, would weigh a variety of factors when making these decisions, and added that the company is “always going to fight aggressively to make sure that we’re getting after the lowest cost.”
“Are you able to raise the price on some of this to offset what could be some volume shortages such that it all kind of nets out to be fairly consistent as far as your overall profit matrix?” asked Valiquette.
Kaufman responded that price decisions would depend on contracts with providers, though the firm has greater flexibility over some drug sales. “As you have changes on the cost side, you’re able to make some adjustments,” he noted.
The discussion, over conference call, occurred during the Barclays Global Healthcare Conference on March 10. At one point, Valiquette joked that “one positive” about the coronavirus would be a “silver lining” that Cardinal Health may receive “less questions” about opioid-related lawsuits.
Cardinal Health is one of several firms accused of ignoring warnings and flooding pharmacies known as so-called pill mills with shipments of millions of highly addictive painkillers. Kaufmann noted that negotiations for a settlement are ongoing.
Owens & Minor, a health care logistics company that sources and manufactures surgical gowns, N95 masks, and other medical equipment, presented at the Barclays Global Healthcare Conference the following day.
Valiquette, citing the Covid-19 crisis, asked the company whether it could “increase prices on some of the products where there’s greater demand.” Valiquette then chuckled, adding that doing so “is probably not politically all that great in the sort of dynamic,” but said he was “curious to get some thoughts” on whether the firm would consider hiking prices.
The inquiry was sharply rebuked by Owens & Minor chief executive Edward Pesicka. “I think in a crisis like this, our mission is really around serving the customer. And from an integrity standpoint, we have pricing agreements,” Pesicka said. “So we are not going to go out and leverage this and try to ‘jam up’ customers and raise prices to have short-term benefit.”
AmerisourceBergen, another health care distributor that supplies similar products to Cardinal Health, which is also a defendant in the multistate opioid litigation, faced similar questions from Valiquette at the Barclays event.
Steve Collis, president and chief executive of AmerisourceBergen, noted that his company has been actively involved in efforts to push back against political demands to limit the price of pharmaceutical products.
Collis said that he was recently at a dinner with other pharmaceutical firms involved with developing “vaccines for the coronavirus” and was reminded that the U.S. firms, operating under limited drug price intervention, were among the industry leaders — a claim that has been disputed by experts who note that lack of regulation in the drug industry has led to few investments in viral treatments, which are seen as less lucrative. Leading firms developing a vaccine for Covid-19 are based in Germany, China, and Japan, countries with high levels of government influence in the pharmaceutical industry.
AmerisourceBergen, Collis continued, has been “very active with key stakeholders in D.C., and our priority is to educate policymakers about the impact of policy changes,” with a focus on “rational and responsible discussion about drug pricing.”
Later in the conversation, Valiquette asked AmerisourceBergen about the opioid litigation. The lawsuits could cost as much as $150 billion among the various pharmaceutical and drug distributor defendants. Purdue Pharma, one of the firms targeted with the opioid litigation, has already pursued bankruptcy protection in response to the lawsuit threat.
“We can’t say too much,” Collis responded. But the executive hinted that his company is using its crucial role in responding to the pandemic crisis as leverage in the settlement negotiations. “I would say that this crisis, the coronavirus crisis, actually highlights a lot of what we’ve been saying, how important it is for us to be very strong financial companies and to have strong cash flow ability to invest in our business and to continue to grow our business and our relationship with our customers,” Collis said.
The hope that the coronavirus will benefit firms involved in the opioid crisis has already materialized in some ways. New York Attorney General Letitia James announced last week that her lawsuit against opioid firms and distributors, including Cardinal Health and AmerisourceBergen, set to begin on March 20, would be delayed over coronavirus concerns.
MARKET PRESSURE has encouraged large health care firms to spend billions of dollars on stock buybacks and lobbying, rather than research and development. Barclays declined to comment, and Cowen & Co. did not respond to a request for comment.
The fallout over the coronavirus could pose potential risks for for-profit health care operators. In Spain, the government seized control of private health care providers, including privately run hospitals, to manage the demand for treatment for patients with Covid-19.
But pharmaceutical interests in the U.S. have a large degree of political power. Health and Human Services Secretary Alex Azar previously served as president of the U.S. division of drug giant Eli Lilly and on the board of the Biotechnology Innovation Organization, a drug lobby group.
During a congressional hearing last month, Azar rejected the notion that any vaccine or treatment for Covid-19 should be set at an affordable price. “We would want to ensure that we work to make it affordable, but we can’t control that price because we need the private sector to invest,” said Azar. “The priority is to get vaccines and therapeutics. Price controls won’t get us there.”
The initial $8.3 billion coronavirus spending bill passed in early March to provide financial support for research into vaccines and other drug treatments contained a provision that prevents the government from delaying the introduction of any new pharmaceutical to address the crisis over affordability concerns. The legislative text was shaped, according to reports, by industry lobbyists.
As The Intercept previously reported, Joe Grogan, a key White House domestic policy adviser now serving on Donald Trump’s Coronavirus Task Force, previously served as a lobbyist for Gilead Sciences.
“Notwithstanding the pressure they may feel from the markets, corporate CEOs have large amounts of discretion and in this case, they should be very mindful of price gouging, they’re going to be facing a lot more than reputational hits,” said Robert Weissman, president of public interest watchdog Public Citizen, in an interview with The Intercept.
“There will be a backlash that will both prevent their profiteering, but also may push to more structural limitations on their monopolies and authority moving forward,” Weissman said.
Weissman’s group supports an effort led by Rep. Andy Levin, D-Mich., who has called on the government to invoke the Defense Production Act to scale up domestic manufacturing of health care supplies.
There are other steps the government can take, Weissman added, to prevent price gouging.
“The Gilead product is patent-protected and monopoly-protected, but the government has a big claim over that product because of the investment it’s made,” said Weissman.
“The government has special authority to have generic competition for products it helped fund and prevent nonexclusive licensing for products it helped fund,” Weissman continued. “Even for products that have no connection to government funding, the government has the ability to force licensing for generic competition for its own acquisition and purchases.”
Drug companies often eschew vaccine development because of the limited profit potential for a one-time treatment. Testing kit companies and other medical supply firms have few market incentives for domestic production, especially scaling up an entire factory for short-term use. Instead, Levin and Weissman have argued, the government should take direct control of producing the necessary medical supplies and generic drug production.
Last Friday, Levin circulated a letter signed by other House Democrats that called for the government to take charge in producing ventilators, N95 respirators, and other critical supplies facing shortages.
The once inconceivable policy was endorsed on Wednesday when Trump unveiled a plan to invoke the Defense Production Act to compel private firms to produce needed supplies during the crisis. The law, notably, allows the president to set a price ceiling for critical goods used in an emergency.

The distinction may sound academic. But understanding it is actually vital to designing the policies that should follow.
In an economic crisis, you could imagine a situation in which people lose their jobs and are unable to spend money. That’s called a demand shock, which is what happened during the global financial crisis of 2008. Or producers could raise prices (for various reasons), making it harder to buy their goods. That’s a supply shock, and it describes the oil crises of 1973 and 1979. But what is happening now cannot be addressed primarily by economic responses, because we are witnessing the suspension of economics itself.
Today, even if you have money, increasingly you cannot go into a shop, restaurant, theater, sports arena or mall because those places are closed. If you own a factory that hasn’t already closed for health reasons, you may still have to shut it down because you can’t get key components from suppliers or you can’t find enough stores open to sell your goods.
In these conditions, cash to consumers cannot jump-start consumption. Relief to producers will not jump-start production. This problem is on a level different and far greater than the recession of 2008 or the aftermath of 9/11. If it were to go on for months, it could look worse than the Great Depression.
This is not an argument against any of the economic measures being proposed. People need to be able to eat, buy medicine and pay their bills. New York Times columnist Andrew Ross Sorkin has canvassed experts and concluded that the best approach would be a zero-interest “bridge loan” to all businesses and self-employed people as long as they keep most of their workers on staff. It is probably the right course of action, massively expensive but cheaper than a full-blown Great Depression.
But even that might not work if we do not recognize that first and foremost the United States faces a health crisis. And that crisis is not being solved. China is now reporting no new domestic infections. South Korea, Taiwan and Singapore have also made progress in “flattening the curve” — the phrase of the year — because they have prioritized dealing with the health-care crisis over enacting a grand economic stimulus.
The United States is still dangerously behind the curve. A headline in Thursday’s Wall Street Journal is, “Coronavirus Testing Chaos Across America.” The article details how the country still has “a chaotic patchwork of testing sites,” with testing proceeding “far slower than experts say is necessary, in part due to a slow federal response.” The U.S. testing rate remains shockingly low, well behind the rates of most other rich countries and far behind those of the Asian countries that are handling this crisis best. Across the United States, hospitals are warning of a dire shortage of beds, medical equipment and supplies. And the worst is yet to come. With infections doubling every two to three days, the U.S. health-care system will face what New York Gov. Andrew Cuomo correctly described as a “tsunami.”
The Trump administration is still acting slowly and fitfully. Experts predicted weeks ago that cities would need thousands more hospital beds, and yet the Navy is still performing maintenance on two hospital ships and figuring out staffing. The president says he will invoke “defense production” powers only if necessary. What is he waiting for? He should direct firms to start production of all key medical equipment in short supply. The armed forces should be deployed immediately to set up field testing and hospital sites. Hotels and convention centers should be turned into hospitals. The federal government should announce a Manhattan Project-style public-private partnership to find and produce a vaccine. After decades of attacks on government, federal agencies are understaffed, underfunded and ill-equipped to handle a crisis of this magnitude. They need help, and fast.
And here’s another idea: President Trump could forge an international effort to unite the world against this common threat. If the United States, China and the European Union worked together, prospects for success — on a vaccine, for example — would be greater. China in particular produces most of the supplies and medical ingredients the world needs. Trump should remove all of his self-defeating tariffs so that American consumers don’t have to pay more for these goods and China can ramp up production. This is a war, and in a war you try to find allies rather than create enemies.

AS THE NEW CORONAVIRUS spreads illness, death, and catastrophe around the world, virtually no economic sector has been spared from harm. Yet amid the mayhem from the global pandemic, one industry is not only surviving, it is profiting handsomely.
“Pharmaceutical companies view Covid-19 as a once-in-a-lifetime business opportunity,” said Gerald Posner, author of “Pharma: Greed, Lies, and the Poisoning of America.” The world needs pharmaceutical products, of course. For the new coronavirus outbreak, in particular, we need treatments and vaccines and, in the U.S., tests. Dozens of companies are now vying to make them.
“They’re all in that race,” said Posner, who described the potential payoffs for winning the race as huge. The global crisis “will potentially be a blockbuster for the industry in terms of sales and profits,” he said, adding that “the worse the pandemic gets, the higher their eventual profit.”
The ability to make money off of pharmaceuticals is already uniquely large in the U.S., which lacks the basic price controls other countries have, giving drug companies more freedom over setting prices for their products than anywhere else in the world. During the current crisis, pharmaceutical makers may have even more leeway than usual because of language industry lobbyists inserted into an $8.3 billion coronavirus spending package, passed last week, to maximize their profits from the pandemic.
Initially, some lawmakers had tried to ensure that the federal government would limit how much pharmaceutical companies could reap from vaccines and treatments for the new coronavirus that they developed with the use of public funding. In February, Rep. Jan Schakowsky, D-Ill., and other House members wrote to Trump pleading that he “ensure that any vaccine or treatment developed with U.S. taxpayer dollars be accessible, available and affordable,” a goal they said couldn’t be met “if pharmaceutical corporations are given authority to set prices and determine distribution, putting profit-making interests ahead of health priorities.”
When the coronavirus funding was being negotiated, Schakowsky tried again, writing to Health and Human Services Secretary Alex Azar on March 2 that it would be “unacceptable if the rights to produce and market that vaccine were subsequently handed over to a pharmaceutical manufacturer through an exclusive license with no conditions on pricing or access, allowing the company to charge whatever it would like and essentially selling the vaccine back to the public who paid for its development.”
But many Republicans opposed adding language to the bill that would restrict the industry’s ability to profit, arguing that it would stifle research and innovation. And although Azar, who served as the top lobbyist and head of U.S. operations for the pharmaceutical giant Eli Lilly before joining the Trump administration, assured Schakowsky that he shared her concerns, the bill went on to enshrine drug companies’ ability to set potentially exorbitant prices for vaccines and drugs they develop with taxpayer dollars.
The final aid package not only omitted language that would have limited drug makers’ intellectual property rights, it specifically prohibited the federal government from taking any action if it has concerns that the treatments or vaccines developed with public funds are priced too high.
“Those lobbyists deserve a medal from their pharma clients because they killed that intellectual property provision,” said Posner, who added that the language prohibiting the government from responding to price gouging was even worse. “To allow them to have this power during a pandemic is outrageous.”
The truth is that profiting off public investment is also business as usual for the pharmaceutical industry. Since the 1930s, the National Institutes of Health has put some $900 billion into research that drug companies then used to patent brand-name medications, according to Posner’s calculations. Every single drug approved by the Food and Drug Administration between 2010 and 2016 involved science funded with tax dollars through the NIH, according to the advocacy group Patients for Affordable Drugs. Taxpayers spent more than $100 billion on that research.
Among the drugs that were developed with some public funding and went on to be huge earners for private companies are the HIV drug AZT and the cancer treatment Kymriah, which Novartis now sells for $475,000.
In his book “Pharma,” Posner points to another example of private companies making exorbitant profits from drugs produced with public funding. The antiviral drug sofosbuvir, which is used to treat hepatitis C, stemmed from key research funded by the National Institutes of Health. That drug is now owned by Gilead Sciences, which charges $1,000 per pill — more than many people with hepatitis C can afford; Gilead earned $44 billion from the drug during its first three years on the market.
“Wouldn’t it be great to have some of the profits from those drugs go back into public research at the NIH?” asked Posner.
Instead, the profits have funded huge bonuses for drug company executives and aggressive marketing of drugs to consumers. They have also been used to further boost the profitability of the pharmaceutical sector. According to calculations by Axios, drug companies make 63 percent of total health care profits in the U.S. That’s in part because of the success of their lobbying efforts. In 2019, the pharmaceutical industry spent $295 million on lobbying, far more than any other sector in the U.S. That’s almost twice as much as the next biggest spender — the electronics, manufacturing, and equipment sector — and well more than double what oil and gas companies spent on lobbying. The industry also spends lavishly on campaign contributions to both Democratic and Republican lawmakers. Throughout the Democratic primary, Joe Biden has led the pack among recipients of contributions from the health care and pharmaceutical industries.
Big Pharma’s spending has positioned the industry well for the current pandemic. While stock markets have plummeted in reaction to the Trump administration’s bungling of the crisis, more than 20 companies working on a vaccine and other products related to the new SARS-CoV-2 virus have largely been spared. Stock prices for the biotech company Moderna, which began recruiting participants for a clinical trial of its new candidate for a coronavirus vaccine two weeks ago, have shot up during that time.
On Thursday, a day of general carnage in the stock markets, Eli Lilly’s stock also enjoyed a boost after the company announced that it, too, is joining the effort to come up with a therapy for the new coronavirus. And Gilead Sciences, which is at work on a potential treatment as well, is also thriving. Gilead’s stock price was already up since news that its antiviral drug remdesivir, which was created to treat Ebola, was being given to Covid-19 patients. Today, after Wall Street Journal reported that the drug had a positive effect on a small number of infected cruise ship passengers, the price went up further.
Several companies, including Johnson & Johnson, DiaSorin Molecular, and QIAGEN have made it clear that they are receiving funding from the Department of Health and Human Services for efforts related to the pandemic, but it is unclear whether Eli Lilly and Gilead Sciences are using government money for their work on the virus. To date, HHS has not issued a list of grant recipients. And according to Reuters, the Trump administration has told top health officials to treat their coronavirus discussions as classified and excluded staffers without security clearances from discussions about the virus.
Former top lobbyists of both Eli Lilly and Gilead now serve on the White House Coronavirus Task Force. Azar served as director of U.S. operations for Eli Lilly and lobbied for the company, while Joe Grogan, now serving as director of the Domestic Policy Council, was the top lobbyist for Gilead Sciences.


Pharmaceutical companies spending on R&D and buybacks.
In 2018, the year the Republican tax law went into full effect, 12 of the largest pharmaceutical companies spent more money buying back their stock than they spent on drug research and development, Axios’ Bob Herman reports.
The big picture: When billions of dollars became available to the biggest drug companies, their main priority was to juice earnings, along with the paydays of their executives and investors — not investments in new treatments or relief for patients who can’t afford their drugs.
By the numbers: Axios analyzed the stock buybacks and R&D expenses of the 12 largest American pharmaceutical companies, by revenue, between 2016 and 2019.
What they’re saying: Amgen said in a statement that it repurchased large quantities of stock because the tax law allowed the company to bring home cash that was parked overseas. Biogen submitted a statement saying it has a “deep commitment to R&D,” but did not address questions about its stock buybacks.
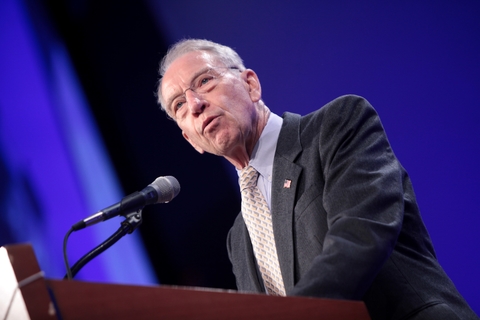
Sen. Chuck Grassley, R-Iowa, and Ron Wyden, D-Ore., are demanding Optum and Express Scripts turn over documents on how they determine insulin prices.
Leaders of the Senate Finance Committee demanded Cigna and Optum produce critical documents over the pricing of insulin, with a subpoena threat looming.
Cigna failed to produce any documents related to the committee’s request back in April 2019 and Optum didn’t produce essential documents, according to letters to both companies sent earlier this week by committee leaders. The documents would relate to the actions of pharmacy benefit managers such as Cigna’s Express Scripts on the rising costs of insulin.
“Cigna’s unwillingness to provide the documents we requested fits an industry-wide pattern of fighting efforts to shed light on PBMs’ practices,” the letter (PDF) to the insurer read.
Sens. Chuck Grassley, R-Iowa, and Ron Wyden, D-Ore., the committee’s chairman and ranking member respectively, wrote that Cigna’s failure to comply has “reached an endpoint.” The insurer has until March 10 to provide more information or face a subpoena.
UnitedHealth Group’s Optum did produce thousands of pages for the committee, but a majority of them were irrelevant, already publicly available or duplicative.
“For example, Optum has produced more than 4,000 pages of publicly available formulary information guides and internal formulary drug lists that contain virtually no information related to the insulin therapeutic class,” the senators’ letter (PDF) to Optum said.
The original request for documentation had called for internal communications that would help the committee understand how Optum made decisions on “the out-of-pocket price patients pay for their insulin,” the letter said.
Grassley and Wyden launched the investigation last February into the price of insulin, which has increased up to 500%. The senators sent letters to leading insulin manufacturers Eli Lilly, Novo Nordisk and Sanofi regarding the spike.
The senators also wanted to learn the process used for negotiations and agreements between PBMs and large plans on patient cost-sharing.
Cigna-Express Scripts said that it takes the committee’s inquiry “very seriously and have been engaged with them on this request. We are committed to being cooperative.”
Optum said that it share’s the committee’s concens regarding the high prices for insulin set by manufacturers.
“We have provided thousands of pages of documents in response to the committee’s request, and will continue to work with them on this important issue,” the company said.
https://theconversation.com/high-priced-specialty-drugs-exposing-the-flaws-in-the-system-129598

My husband, Andy, has Parkinson’s disease. A year ago, his neurologist recommended a new pill that he was to take at bedtime. We quickly learned that the medication would cost US$1,300 for a one-month supply of 30 pills. In addition, Andy could obtain the drug from only one specialty pharmacy and would have to use mail order.
This was our introduction to specialty drugs.
These medications are becoming increasingly common, though many Americans are unfamiliar with the term. In 2018, the Food and Drug Administration approved 59 new medications, of which 39 are considered specialty drugs.
Specialty drugs are generally high-cost drugs requiring special handling such as refrigeration or injection, though Andy’s did not. They treat complex conditions such as cancer and multiple sclerosis.
Specialty drugs are often available only through specialty pharmacies. In addition to filling prescriptions, these outlets provide educational and support services to patients. For example, they provide refill reminders and help patients learn how to inject their drugs.
In a forthcoming article, professor Isaac Buck and I argue that specialty drugs raise significant legal and ethical questions. These merit attention from the public and policymakers.
First, the term “specialty drug” is somewhat elusive and has no clear definition. In addition, government authorities and medical experts are not the ones who decide whether a medication is designated a specialty drug. Rather, the decision is entirely up to pharmacy benefit managers, or PBMs.
PBMs administer health plans’ drug benefit programs and thereby serve insurers. PBMs have been criticized for driving up health care costs. Drugs that are specialty drugs under one insurance policy are sometimes classified differently in other policies. Furthermore, some specialty drugs are simple pills that do not involve complicated instructions, and thus, it is unclear why they are categorized as specialty drugs.
The second problem is the very high cost of specialty drugs. The average price tag of the more than 300 medications that are considered specialty drugs is approximately $79,000 per year. Almost half of the dollars that Americans pay for medications are spent on specialty drugs. In fact, Medicare spent $32.8 billion on specialty drugs in 2015.
Because of these exorbitant costs, some insurers have created what they call a “specialty tier” in their health plans. In this tier, patients’ cost-sharing responsibilities are higher than they are for medications in other tiers. If your drug is placed in a specialty tier, your coinsurance payment, or the percentage of cost that you pay, may be 25% to 33% of the drug’s price.
This leads to a situation in which you may have the least generous insurance coverage for your most expensive drugs. Under some plans you might pay $10 per month for generic drugs but hundreds of dollars per month for specialty drugs. This can translate into many thousands of dollars in annual out-of-pocket costs, even for consumers with good health insurance. There are no federal regulations in the U.S. that limit drug prices or insurers’ tiering practices.
A third problem is conflict of interest. PBMs own or co-own the top four specialty pharmacies in the U.S., which are responsible for two-thirds of nationwide specialty drug prescription revenues.
PBMs frequently require patients to purchase their medications from the specific specialty pharmacy that they own. Thus, PBMs have much to gain from designating medications as specialty drugs. Doing so may lead to significant revenues in the form of purchases at PBM-owned specialty pharmacies.
A related problem is the limiting of patient choice. Many specialty pharmacies fill prescriptions only through mail order. Consequently, patients may be restricted to using just one pharmacy and be forced to rely on the mail for delivery.
Some patients enjoy the convenience of home delivery. Others, however, prefer the traditional approach of visiting a drugstore in person. They may worry that the mail will be late, their package will be stolen, or they will be out of town when the drugs arrive. Yet, such patients do not have the option of a brick and mortar pharmacy.
Both political parties have stated that health care costs are a priority for them. However, they have shown a limited appetite for tackling this herculean problem.
The House recently passed a bill that would enable the federal government to negotiate prices with drug manufacturers. Such negotiations could well lower specialty drug prices. The Senate, however, is unlikely to approve the bill, and Congress is unlikely to pass sweeping legislation in a divisive election year.
There has been more success at the federal level in promoting consumer choice. Medicare rules establish that Medicare plans may not force participants to use mail-order pharmacies.
In the meantime, individual states offer useful solutions. For example, some have provided patients with relief in the form of capping out-of-pocket costs. California limits consumers’ expenditures to $250 or $500 for a 30-day supply, depending on the drug type.
At least 15 states also have pharmacy choice statutes. Several ban PBM mandates that prevent patients from freely selecting their preferred qualified pharmacy. Many ban mail-order only requirements.
Some states have recognized that PBMs should not be entirely free to designate medications as specialty drugs. Because such designations can significantly disadvantage patients and may increase patients’ costs, such states have statutory definitions for the term “specialty drug.”
They generally mandate that the drug require special administration, delivery, storage or oversight. Such requirements may justify purchase from a specialty pharmacy. However, drugs without complicated instructions should not be deemed specialty drugs.
One more option that some insurers have already adopted is allowing patients to obtain just a few pills or doses for an initial trial period. Sometimes individuals quickly learn that they cannot tolerate a medication or that it is ineffective. Such “partial fill” programs can spare patients the exorbitant cost of a full 30-day specialty drug supply.
Specialty drugs contribute significantly to the American health care cost crisis. Additional state, or better yet, federal laws should be enacted to constrain PBMs’ authority over specialty drugs. We need further regulation concerning drug classification, pricing, conflicts of interest and patient choice.

As the new coronavirus, called 2019-nCoV, spreads rapidly around the globe, the international community is scrambling to keep up. Scientists rush to develop a vaccine, policymakers debate the most effective containment methods, and health care systems strain to accommodate the growing number of sick and dying. Though it may sound like a scene from the 2011 movie “Contagion,” it is actually an unfolding reality.
In the midst of all of this, a potential crisis simmers in the shadows: The global dependence on China for the production of pharmaceuticals and medical equipment.
We represent an interdisciplinary group of scientists and policymakers at the Scowcroft Institute’s Pandemic and Biosecurity Policy Program based at the Bush School of Government at Texas A&M University who have been holding annual summits addressing pandemic-related issues for the past five years. One of our goals is to promote dialogue on potential risks related to pandemics and U.S. security, in this case the disruption of supply chains and availability of medical supplies and drugs.
Today, about 80% of pharmaceuticals sold in the U.S. are produced in China. This number, while concerning, hides an even greater problem: China is the largest and sometimes only global supplier for the active ingredient of some vital medications. The active ingredients for medicines that treat breast cancer and lung cancer and the antibiotic Vancomycin, which is a last resort antibiotic for some types of antimicrobial resistant infections, are made almost exclusively in China. Additionally, China controls such a large market portion of heparin, a blood thinner used in open-heart surgery, kidney dialysis and blood transfusions that the U.S. government was left with no choice but to continue buying from China even after a contamination scandal in 2007.
China is not only the dominant global supplier of pharmaceuticals, but it is also the largest supplier of medical devices in the U.S. These include things like MRI equipment, surgical gowns, and equipment that measures oxygen levels in the blood. Supplies of these essential products have not yet been severely disrupted by the coronavirus, but if China is no longer will or able to supply them to the U.S., thousands of Americans could die.
More concerning still are the limited options available to the U.S. and the rest of the globe to make up the shortfall. It could take years to develop the necessary infrastructure to reestablish U.S. manufacturing capacities and obtain Food and Drug Administration licensure to overcome the loss of the Chinese supply.
When a disease reaches epidemic levels, the first obligation for leaders in any country is to protect their own people. As this current crisis progresses, there may come a point when political leaders in China will face decisions on whether to prohibit the export of pharmaceuticals, medical devices and other vital medical components in order to treat or protect their own people. Such acts would be the logical outcome of an escalating situation. For the 2009 H1N1 pandemic response, for example, the U.S. was pushed to the back of the queue for vaccine deliveries even though we had existing contracts with a major vaccine manufacturer located in another country. Those vaccine deliveries were delayed.
While a total loss of active ingredient imports from China might seem far-fetched, we believe the increasing scale of the outbreak moves it closer to the realm of possibility.
About six weeks into international recognition of the epidemic in China, there are already shortages of vital personal protective equipment in both China and the U.S. UPS has transported more than 2 million masks and 11,000 gowns to Wuhan to help alleviate the shortage. But what happens when everyone runs out of protective equipment?
Wuhan is a significant player in the biotechnology and pharmaceutical industry, with multiple pharmaceutical companies located in the city. How many of these factories have closed as a result of the pandemic, and when will those that have closed open back up? Global supply chains could reach a crisis point if they are compromised because Hubei province, where Wuhan is located, is in quarantine and factories are shut down.
Additionally, Wuhan is the location of China’s first Biosafety Level (BSL) 4 laboratory, which was opened in 2017 to research SARS and other emerging diseases. It is the only lab in China that can safely handle the world’s most dangerous pathogens that pose a significant risk of transmission. Infection, death and quarantine in Wuhan and the surrounding Hubei province is restricting the ability of all types of commerce in the region. Meanwhile, the virus is already creating a significant supply chain imbalance within China. That means those medical supply companies will be under pressure to keep any products produced within the country for protection of their own health care workers, laboratory personnel and the general public.
The regulatory apparatus to insure that the Chinese manufactured pharmaceuticals being exported meet the highest standards of safety and quality control are weak or nonexistent, according to a congressional report last year. The pressure placed on supply chains by the outbreak could further exacerbate existing quality control challenges. In doing so, the virus has highlighted our reliance on China as a U.S. national security issue due to outsourcing our manufacturing capabilities and inability to ensure quality control.
As with all pandemics, the complexity of this outbreak demands international collaboration and transparency. At the same time, U.S. public health officials must acknowledge the country’s vulnerability due to our dependence on Chinese production of pharmaceuticals and medical equipment. The U.S. must develop a response plan for the inevitable shortages in the near-term and take necessary actions to reclaim control of our medical supply chain. Continuing to overlook this long-known vulnerability will only lead to catastrophe.