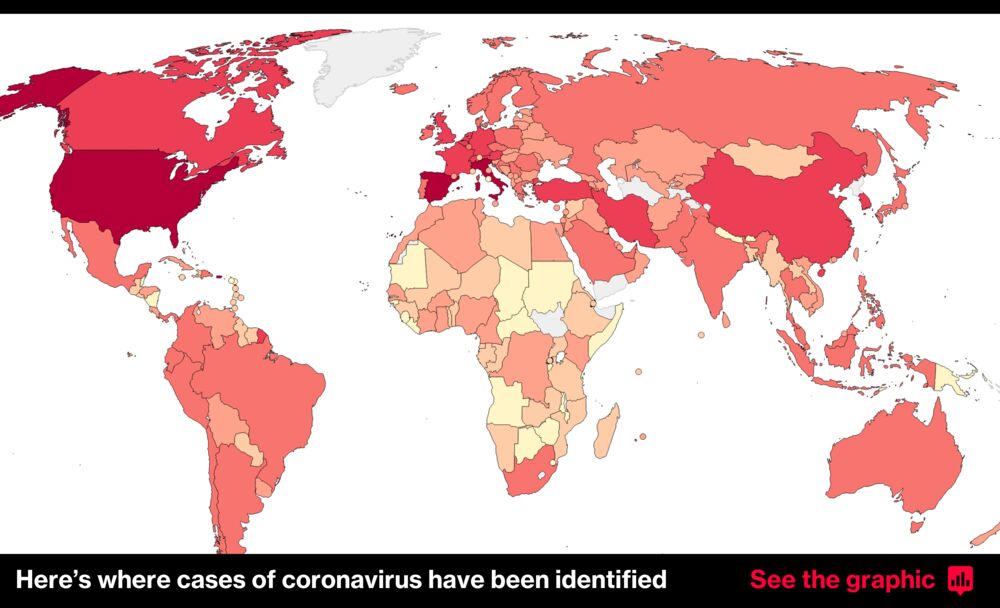
The coronavirus has killed nearly 4 million people since it first emerged in Wuhan, China, in 2019, according to data compiled by Johns Hopkins University.
New confirmed cases of covid-19, the disease caused by the virus, remain high, and the world struggles with unequal vaccine rollouts and new threats posed by fast-spreading variants.
“The pandemic is a long way far from over,” World Health Organization Director General Tedros Adhanom Ghebreyesus warned in May. “It will not be over anywhere until it’s over everywhere.”
Some countries have already found that the spread of the virus is outpacing their vaccination plans, especially in the face of proliferating variants. In India, new daily cases topped 400,000 in early May — a global record but probably an undercount.
China now leads the world in the number of vaccine doses given out, though some other nations have vaccinated far more of their population. The vaccines were developed and rolled out at record speed, and studies show most have impressive efficacy.
More than a billion doses have been administered around the world, far more than the number of confirmed cases of the coronavirus since the start of the pandemic — though a large number of cases were likely never recorded, experts caution.
But the vaccine rollout has been persistently unequal, with problems with global supply and pockets of opposition in many nations. Covax, a program to distribute vaccines fairly backed by the World Health Organization, only belatedly began distributing doses to low-income nations.
“I can’t say it’s surprising,” said Thomas J. Bollyky, a senior fellow at the Council on Foreign Relations. “In every previous pandemic where we have our global health crisis, where there has been limited supplies of medical intervention, wealthy nations have hoarded.”
The United States, which continues to have the highest cumulative number of confirmed cases and deaths globally. More than 590,000 deaths from covid-19 have been recorded across the country.
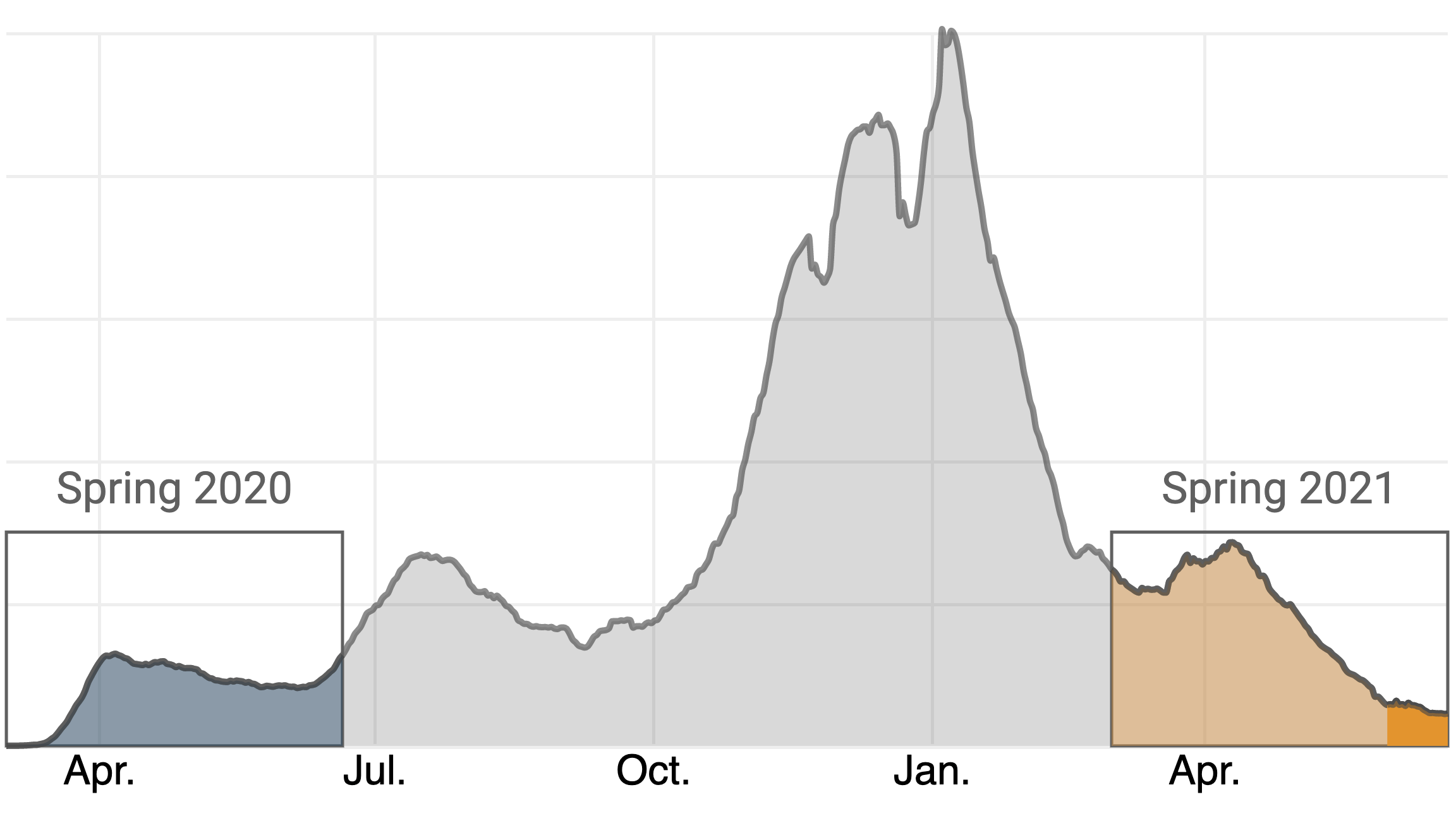
Though cases dipped after January, a new wave began only a few months later, prompting President Biden to urge governors to reinstate mask mandates and other virus-related restrictions. “This is deadly serious,” Biden said in March.
Behind the United States, India, Brazil, France and Turkey have the largest number of cases.
India’s record-setting surge this spring meant the country accounted for about 1 in 3 of all new confirmed cases. The spike, which has been blamed on complacency and the lifting of restrictions, along with the spread of variants, has seen the country’s health-care system overwhelmed amid widespread oxygen shortages.
Even after the spike in new cases subsided in mid-May, India still set records for the number of new daily deaths with more than 4,500 deaths from covid-19 reported in a single 24-hour period.
In India, as in Britain and Brazil before it, some of the spread of the virus has been blamed on fast-spreading variants rampant in the country.
The variant widespread in India, known by the name B.1.617.2, has spread far beyond its borders. In May, British officials warned that it would likely become dominant across Britain unless more was done to control its spread.
Sharon Peacock, director of the U.K.’s Covid-19 Genomics Consortium, told reporters that a fast-spreading variant such as B.1.617.2 had “a biological passport for international travel and global spread” — making its spread difficult, if not impossible, to fully contain.
Some countries have seen success at controlling the virus.
In New Zealand, which closed its borders and ordered people to stay home as a first wave hit in the spring of 2020, confirmed infections went down to zero for a time. Taiwan and Singapore have kept their outbreaks far smaller than those in other parts of the world, which some experts attribute to their early responses and sophisticated tracking and tracing.
China, the early epicenter of the crisis, has seen much of daily life return to normal. In the early months of the outbreak, it reported more cases than any other country. Its tally of new infections peaked in mid-February of 2020 and approached zero by mid-March, although questions surround the accuracy of its data.
Wuhan, the virus’s initial epicenter, ground to a standstill in January 2020 as the coronavirus spiraled out of control. But after months without a confirmed case of domestic transmission, about 1.4 million children in the city returned to classrooms at the start of September, and crowded events have resumed.
Countries that have successfully rolled out vaccines are also seeing important gains. Britain, one of the hardest-hit countries in terms of cases and deaths, has excelled in the distribution of coronavirus vaccines. It was the first country to roll out a fully tested vaccine to the general public in December, when it began distributing the vaccine developed by Pfizer and Moderna.
Data released by Public Health England in March suggested that vaccinations had saved over 6,000 lives among people over 70, if not more.
Israel, which has seen several waves of the virus, had raced ahead of other nations and given the first doses of Pfizer’s two-dose vaccine to more than a third of its population by the end of January. Data from Israel indicated that the Pfizer vaccine was around 94 percent effective at stopping asymptomatic infection.
Early signs from the country suggest that the large scale of vaccinations has had an impact on the spread of the virus.
But global health experts have cautioned that despite the success of vaccines, the virus remains a potent threat and returning to normal life too early could ultimately extend the length of the pandemic and lead to fresh new cases.
Though wealthy countries have taken some steps to ensure vaccines are shared around the world, such as by donating through Covax or supporting waivers on intellectual property such as the Biden administration has done, experts say they are worried by the ongoing level of spread.
“Sadly, unless we act now, we face a situation in which rich countries vaccinate the majority of their people and open their economies, while the virus continues to cause deep suffering by circling and mutating in the poorest countries,” United Nations Secretary General António Guterres said at a meeting of the World Health Assembly on May 24.