Healthcare costs are expected to jump 6.0% next year. CFOs must prepare accordingly, advises WTW’s Tim Stawicki.
CFOs need to be prepared for a “higher tail” of medical inflation — even if general inflation eases in the near future, Tim Stawicki, chief actuary, North America health & benefits of Willis Towers Watson (WTW) told CFO Dive.
With the Consumer Price Index (CPI) rising to 8.5% in July and the recent rise in the core Producer Price Index (PPI), the Federal Reserve will probably look to hike interest rates even farther.
“CFOS need to be prepared for the case that if general inflation eases, there may be two or three more years where they need to think about how they are managing the costs of health care plans,” he said in an interview.
Inflation, which can more immediately impact consumer prices, works somewhat differently when it comes to costs of medical care. “Employers are paying healthcare costs based on contracts that their insurer has with providers, which are multiple years in length. So if a deal with the hospital or contract does not come up until 2023, then that provider has the opportunity to renegotiate higher prices for three years,” said Stawicki.
The recent Best Practices in Healthcare Survey by WTW consisting of 455 U.S. employers found that employers project their healthcare costs will jump 6.0% next year compared with an average 5.0% increase expected by the end of this year.
Further, employers see little relief in sight — seven in 10 (71%) expect moderate to significant increases in costs over the next three years. Additionally, over half of respondents (54%) expect their costs will be over budget this year.
Balancing talent retention and healthcare costs
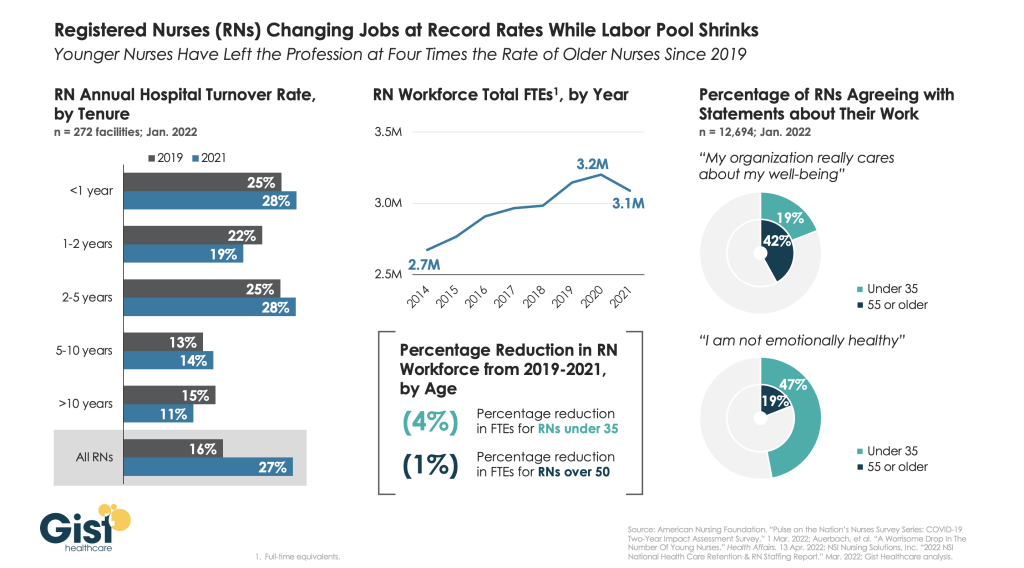
Talent retention has also remained an entrenched challenge for CFOs over recent months and continues to be top of mind.
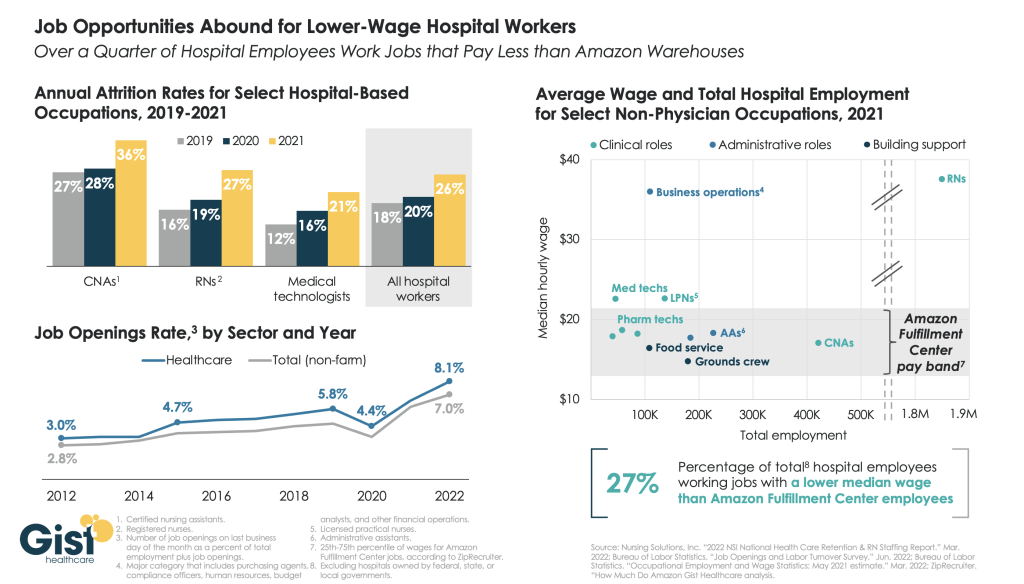
Given inflationary pressures and a potential looming recession, employers are having trouble finding the workers they need to run their businesses. A rise in healthcare benefit costs will make this all the more challenging, said Stawicki. “Employers are looking around and saying ‘I need to find talent to help me run my business and I can’t do that if I have an ineffective program in healthcare benefits,’” he said.
There is a direct link between business outcomes and in particular employee productivity and employees’ ability to manage their health and financial environment, according to WTW’s Global Benefits Attitude Survey. “Losing the ability to offer programs and benefits that meet employee needs is impacting business,” said Stawicki.
It comes down to finding the balance between cost management in an environment where talent is hard to come by, he said. In order for CFOs to be successful in financing benefit programs they need to look at finding ways to partner with their counterparts in human resources, said Stawicki.
Sixty-seven percent of employers said that managing company costs was a top priority in the company’s August Best Practices in Healthcare Survey, versus the 42% who said that achieving affordability for employees was a top priority. In the near future, CFOs need to establish a relationship with HR counterparts that can facilitate “ways to manage company costs without shifting it to employees,” said Stawicki.
Ultimately, company costs remain paramount for employers but running a successful business will also require keeping employee affordability top of mind.