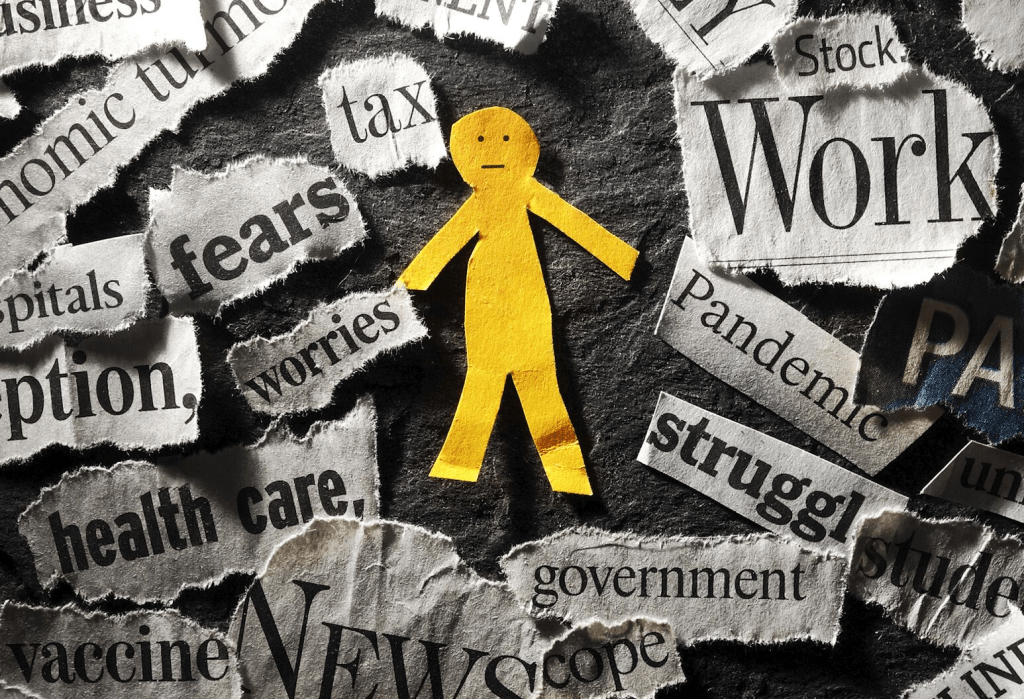
The U.S. bombing of Iran’s nuclear capability is unsettling: whether MAGA or not, hawk or dove, young or old, conservative or liberal, rich or poor—it matters.
Stability at home and abroad is utopian to some but desired by all. Pandemics, mass violence, natural disasters and even election results contribute to instability and lend to insecurity. Operation Midnight Hammer might contribute to the nation’s anxiety—time will tell.
The immediate aftermath of the bunker-bombings in Iran will involve two orchestrated campaigns by government officials:
- The Campaign to Contain Middle East Tension: military, diplomatic and economic levers will be put to the test to limit escalation of the bombing and limit its consequence to the region.
- The Campaign to Win Public Support: issues of consequence like military intervention ultimately depend on public opinion that support laws, funding and subsequent actions taken in response. History teaches and political leaders understand that ‘winning the hearts and minds’ of the public is necessary to success. Predictably, justification for Operation Midnight Hammer will be messaged loudly by supporters and challenged by critics.
For the moment, the news cycle will shift to foreign policy and away from tariffs, inflation, household prices and the “Big Beautiful Budget Bill” which the Senate Republicans hope to bring to the floor this week. News media will speculate about the after-effects of the Israeli-Iran bombing and what role the U.S. plays in an increasingly complicated geopolitical landscape marked by marked by armed conflicts Gaza, Ukraine, Myanmar, Yemen and 26 and other countries.
The attention these get in traditional media and social media channels will exacerbate public anxiety that’s already high: 19% U.S. adults and 40% of the country’s adolescents suffer from anxiety disorder: “a persistent, excessive fear or worry that interferes with daily life and functioning”. But, per the National Institute of Mental Health, fewer than a third suffering from severe anxiety receive professional treatment.
In the public health community, much is known about anxiety: it’s more prevalent among women than men, in minority populations, lower income populations and in the Southeast. It’s significant across all age groups, and at an alarming level among young working-class adults facing unique issues like affordability and job insecurity. And it is stigmatized in certain communities (i.e. certain fundamentalist religious sects, certain ethnic communities) lending to silent suffering and unattended consequences.
My take:
Operation Midnight Hammer came at a time of widespread public anxiety about the economy, tariffs, inflation, costs of living and political division. I will let pundits debate the advisability and timing of the bunker-bombing but I know one thing for sure: mental health issues—including anxiety, mood and substance abuse disorders– deserve more support from policymakers and more attention by the healthcare community.
- The former requires local, state and federal lawmakers to revisit and enforce mental health parity laws already on the books but rarely enforced.
- The latter requires the healthcare community to elevate behavioral health to a national priority alongside obesity, heart disease, cancer and aging to secure the public’s health and avoid unintended consequences of neglect.
Regrettably, the issue is not new. Employers, school systems, religious organizations and local public health agencies have been mental health default safety values to date; extreme have been temporarily shuffled to in hospital emergency rooms most ill-equipped to manage them. But systematic, community-wide, evidence-based help for those in need of mental health remains beyond their reach.
The Trump administration’s healthcare leaders under HHS’ Kennedy and CMS’ Oz espouse the U.S. healthcare system should prioritize chronic disease and preventive health. They believe its proficiency in specialty care is, in part, the result of lucrative incentives that reward providers and their financial backers handsomely in these areas.
In the President’s February 13 Executive Order establishing the Make America Healthy Again Commission, its goal was laid out:
“To fully address the growing health crisis in America, we must re-direct our national focus, in the public and private sectors, toward understanding and drastically lowering chronic disease rates and ending childhood chronic disease. This includes fresh thinking on nutrition, physical activity, healthy lifestyles, over-reliance on medication and treatments, the effects of new technological habits, environmental impacts, and food and drug quality and safety… We must ensure our healthcare system promotes health rather than just managing disease.”
Nothing could be more timely and necessary to the Commission’s work than addressing mass anxiety and mental health as a national priority. And nothing is more urgently needed in communities than mainstreaming anxiety and mental health into the systems of health that accept full risk for whole person health.
PS: Before Operation Midnight Hammer over the weekend, I had prepared today’s report focused on two government reports about the long-term solvency of the Medicaid and Medicare programs. Given the gravity of events in Israel and Iran and other hot spots, and after discussions with my family and friends this weekend, it became clear public anxiety is high.
I am concerned about the future and worry about the health system’s response. It’s composed of good people doing worthwhile work who are worried about the future. I recently spoke to a group on the theme (link below): ‘the future for healthcare is not a repeat of its past.’ That lends to anxiety unless accompanied by a vision for a better future. That’s what all hope for those in Iran, Gaza, Israel and beyond, and for all who serve in our industry.