The Trump administration has made a flurry of recent moves aimed at lowering the cost of prescription drugs, including cutting deals with some of America’s top drugmakers and launching a new website to help consumers shop for the best available prices. We recently asked 10 experts — including health economists, drug policy scholars and industry insiders — to evaluate the likely impact of those maneuvers. Their verdict: Most are unlikely to deliver substantive savings, at least based on what we know today.
So, we followed up: If those moves won’t work, what could the administration do that would make a meaningful dent in America’s drug spending?
Here are three key ideas from the experts:
1. Expand Medicare’s new power to directly negotiate prices with drugmakers.
Compared to Trump’s recent ad hoc approach to cutting confidential deals with individual drug companies, some experts say building on Medicare’s new power to negotiate could offer a more sweeping, and potentially lasting, path to savings.
For example, Trump’s team could use the price negotiations to seek steeper discounts than the Biden administration did. Federal officials could also establish a more transparent and predictable formula for future negotiations — similar to the approaches used by other nations — and publish that framework so private insurance plans could use it to drive better deals with drugmakers, too.
Finally, the White House could urge lawmakers to loosen some of the limits Democrats in Congress placed on this power when they passed the law back in 2022. Medicare can currently only negotiate the price of drugs that have been on the market for at least several years — often after the medicines have already made drug companies billions of dollars.
Ideally, said Vanderbilt professor Stacie Dusetzina, “you would negotiate a value-based price at the time a product arrives on the market” — that’s what nations like France and England do.
2. Identify and fix policies that encourage wasteful spending on medicines.
“There are policies within everything — from the tax code to Medicare and Medicaid to health insurance regulations — that are driving up drug prices in this country,” said Michael Cannon, who directs health policy studies at the Cato Institute.
One example Cannon sees as wasteful: the formula that Medicare uses to pay for drugs administered by doctors, such as chemotherapy infusions. Those doctors typically get paid 106% of the price of whichever medicine they prescribe, creating a potential incentive to choose those that are most expensive — even in cases where cheaper alternatives might be available.
And that, according to Cannon, is just the tip of the “policy failure” iceberg.
The Trump administration is taking early steps to reform at least one federal drug-pricing policy, known as 340B, which lets some hospitals and clinics purchase drugs at a discount. More than $60 billion a year now flow through this program, whose growth has exploded in recent years. But researchers, auditors and lawmakers like Republican Sen. Bill Cassidy have questioned where all of that money is going and whether it’s making medicines affordable for as many patients as it should.
3. Speed up access to cheaper generic drugs.
Generic drugs — cheaper, copycat versions of brand-name medicines — can slash costs for patients and insurers by as much as 80% once they come to market. But this price-plunging competition often takes more than a decade to arrive.
That’s, in part, because drug companies have found a host of ways to game the U.S. patent system to protect and prolong their monopolies. Law professor Rachel Sachs at Washington University in St. Louis suggested Trump not only close those loopholes, but also make its own creative use of patents.
Federal officials could, for example, invoke an obscure law known as Section 1498, she said. That provision allows the U.S. government to effectively infringe on a patent to buy or make on the cheap certain medicines that meet an extraordinary need of the country. Sachs suggested that the drug semaglutide — the active ingredient in Ozempic, Wegovy and several other weight-loss medicines — might make for an ideal target.
“The statutory authority is already there for them to do it,” Sachs said. “It’s not clear to me why they haven’t.”
Semaglutide, which earned drugmakers more than $20 billion last year alone, will otherwise remain under patent in the U.S. until early next decade.
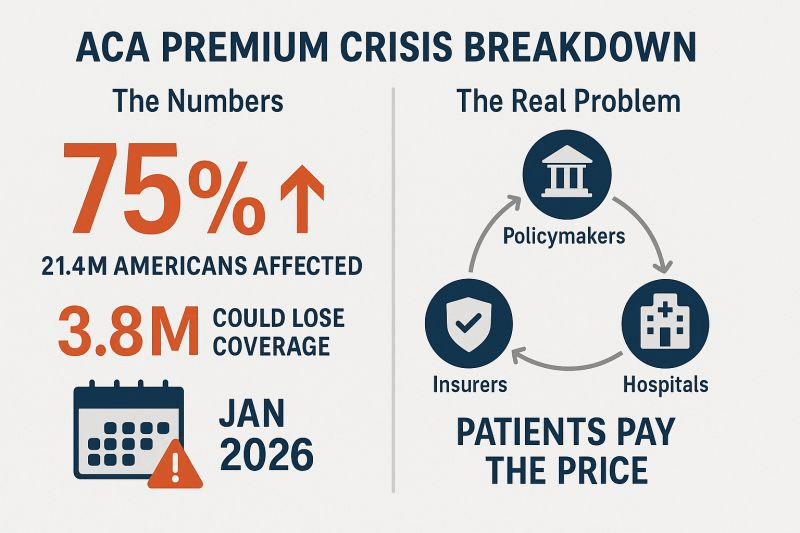
The Trump administration issued an executive order back in April signaling at least a high level of interest in some of these ideas — and a host of others, too. On the other hand, Trump and Congressional Republicans have made moves this year that have weakened some of these potential cost-cutting tools, such as Medicare’s power to negotiate drug prices. A key provision of July’s ‘Big Beautiful Bill,’ for example, shielded more medicines from those negotiations, eroding the government’s potential savings by nearly $9 billion over the next decade.
We should all get a better read soon on just how interested this administration is in cutting prices: Federal officials are expected to announce the results of their latest round of Medicare negotiations by the end of November.