
Category Archives: Debt Collection
Senator has questions for Providence CEO on billing practices

U.S. Senator Patty Murray of Washington is seeking answers from Renton, Wash.-based Providence’s CEO following a Sept. 24 New York Times report detailing the system’s alleged debt collection practices.
“According to recent reports, over the past several years, Providence has increasingly extracted payments from low-income patients, even when patients qualified for free or discounted care,” Ms. Murray said in a Sept. 28 letter to CEO Rod Hochman. “The reports allege several disturbing practices, including high-pressure billing conversations at hospital beds when patients are vulnerable, the use of extraordinary collection actions by debt collectors, and patients eligible for free or discounted care being billed for outstanding balances. As a result, patients have gone without food or heat, have seen their credit scores plummet, and have been afraid to seek out further medical care due to the cost—all as a result of practices that potentially violate both state and federal laws.”
Ms. Murray said in the letter she is seeking answers on how many patients Providence has served in recent years who qualified for free or discounted care and how many it referred to debt collection services. She is also seeking information about the system’s billing and debt collection policies, and how much it paid consulting firm McKinsey & Co. for a program designed to increase its revenue. She is seeking answers by Oct. 12.
Washington state’s attorney general filed a lawsuit against Providence in February, alleging that 14 of its hospitals engaged in aggressive tactics to collect payment, failed to ensure discounts for eligible low-income patients, and steered poor patients to debt collectors.
A Providence spokesperson expressed discontent and disagreement with the attorney general’s charges in a statement shared with Becker’s.
“The Providence family of organizations is extremely disappointed that the Office of the Washington State Attorney General has chosen to file inaccurate and unfair charges against us regarding our charity care and financial assistance practices,” the spokesperson said. “Serving every person who comes to us, regardless of ability to pay, is a central tenet of our mission as a not-for-profit organization. We take this responsibility seriously.”
Why People Are Still Avoiding the Doctor (It’s Not the Virus)

At first, people delayed medical care for fear of catching Covid. But as the pandemic caused staggering unemployment, medical care has become unaffordable for many.
At first, Kristina Hartman put off getting medical care out of concern about the coronavirus. But then she lost her job as an administrator at a truck manufacturer in McKinney, Texas.
While she still has health insurance, she worries about whether she will have coverage beyond July, when her unemployment is expected to run out.
“It started out as a total fear of going to the doctor,” she said.
“I definitely am avoiding appointments.”
Ms. Hartman, who is 58, skipped a regular visit with her kidney doctor, and has delayed going to the endocrinologist to follow up on some abnormal lab results.
While hospitals and doctors across the country say many patients are still shunning their services out of fear of contagion — especially with new cases spiking — Americans who lost their jobs or have a significant drop in income during the pandemic are now citing costs as the overriding reason they do not seek the health care they need.
“We are seeing the financial pressure hit,” said Dr. Bijoy Telivala, a cancer specialist in Jacksonville, Fla. “This is a real worry,” he added, explaining that people are weighing putting food on the table against their need for care. “You don’t want a 5-year-old going hungry.”
Among those delaying care, he said, was a patient with metastatic cancer who was laid off while undergoing chemotherapy. He plans to stop treatments while he sorts out what to do when his health insurance coverage ends in a month.
The twin risks in this crisis — potential infection and the cost of medical care — have become daunting realities for the millions of workers who were furloughed, laid off or caught in the economic downturn. It echoes the scenarios that played out after the 2008 recession, when millions of Americans were unemployed and unable to afford even routine visits to the doctor for themselves or their children.
Almon Castor’s hours were cut at the steel distribution warehouse in Houston where he works about a month ago. Worried that a dentist might not take all the precautions necessary, he had been avoiding a root canal.
But the expense has become more pressing. He also works as a musician. “It’s not feasible to be able to pay for procedures with the lack of hours,” he said.
Nearly half of all Americans say they or someone they live with has delayed care since the onslaught of coronavirus, according to a survey last month from the Kaiser Family Foundation. While most of those individuals expected to receive care within the next three months, about a third said they planned to wait longer or not seek it at all.
While the survey didn’t ask people why they were putting off care, there is ample evidence that medical bills can be a powerful deterrent. “We know historically we have always seen large shares of people who have put off care for cost reasons,” said Liz Hamel, the director of public opinion and survey research at Kaiser.
And, just as the Great Recession led people to seek less hospital care, the current downturn is likely to have a significant impact, said Sara Collins, an executive at the Commonwealth Fund, who studies access to care. “This is a major economic recession,” she said. “It’s going to have an effect on people’s demand for health care.”
The inability to afford care is “going to be a bigger and bigger issue moving forward,” said Chas Roades, the co-founder of Gist Healthcare, which advises hospitals and doctors. Hospital executives say their patient volumes will remain at about 20 percent lower than before the pandemic.
“It’s going to be a jerky start back,” said Dr. Gary LeRoy, a physician in Dayton, Ohio, who is the president of the American Academy of Family Physicians. While some of his patients have returned, others are staying away.
But the consequences of these delays can be troubling. In a recent analysis of the sharp decline in emergency room visits during the pandemic, officials from the Centers for Disease Control and Prevention said there were worrisome signs that people who had heart attacks waited until their conditions worsened before going to the hospital.
Without income, many people feel they have no choice. Thomas Chapman stopped getting paid in March and ultimately lost his job as a director of sales. Even though he has high blood pressure and diabetes, Mr. Chapman, 64, didn’t refill any prescriptions for two months. “I stopped taking everything when I just couldn’t pay anymore,” he said.
After his legs began to swell, and he felt “very, very lethargic,” he contacted his doctor at Catalyst Health Network, a Texas group of primary care doctors, to ask about less expensive alternatives. A pharmacist helped, but Mr. Chapman no longer has insurance, and is not sure what he will do until he is eligible for Medicare later this year.
“We’re all having those conversations on a daily basis,” said Dr. Christopher Crow, the president of Catalyst, who said it was particularly tough in states, like Texas, that did not expand Medicaid. While some of those who are unemployed qualify for coverage under the Affordable Care Act, they may fall in the coverage gap where they do not receive subsidies to help them afford coverage.
Even those who are not concerned about losing their insurance are fearful of large medical bills, given how aggressively hospitals and doctors pursue people through debt collections, said Elisabeth Benjamin, a vice president at Community Service Society of New York, which works with people to get care.
“Americans are really very aware that their health care coverage is not as comprehensive as it should be, and it’s gotten worse over the past decade,” Ms. Benjamin said. After the last recession, they learned to forgo care rather than incur bills they can’t pay.
Geralyn Cerveny, who runs a day care in Kansas City, Mo., said she had Covid-19 in early April and is recovering. But her income has dropped as some families withdrew their children. Although her daughter is urging her to get some follow-up testing because she has some lingering symptoms from the virus, she is holding off because she does not want to end up with more medical bills if her health plan will not cover all of the care she needs. She said she would dread “a fight with the insurance company if you don’t meet their guidelines.”
Others are weighing what illness or condition merits the expense of a doctor or tests and other services. Eli Fels, a swim instructor and personal trainer who is pregnant, has been careful to stay up-to-date with her prenatal appointments in Cambridge, Mass. She and her doctor have relied on telemedicine appointments to reduce the risk of infection.
But Ms. Fels, who also lost her jobs but remains insured, has chosen not to receive care for her injured wrist in spite of concern over lasting damage. “I’ve put off medical care that doesn’t involve the baby,” she said, noting that her out-of-pocket cost for an M.R.I. to find out what was wrong “is not insubstantial.”
At Maimonides Medical Center in Brooklyn, doctors have already seen the impact of delaying care. During the height of the pandemic, people who had heart attacks and serious fractures avoided the emergency room. “It was as if they disappeared, but they didn’t disappear,” said Dr. Jack Choueka, the chair of orthopedics. “People were dying in home; they just weren’t coming into the hospital.”
In recent weeks, people have begun to return, but with conditions worsened because of the time they had avoided care. A baby with a club foot will now need a more complicated treatment because it was not addressed immediately after birth.
Another child who did not have imaging promptly was found to have a tumor. “That tumor may have been growing for months unchecked,” Dr. Choueka said.
It’s Not Just Hospitals That Are Quick To Sue Patients Who Can’t Pay
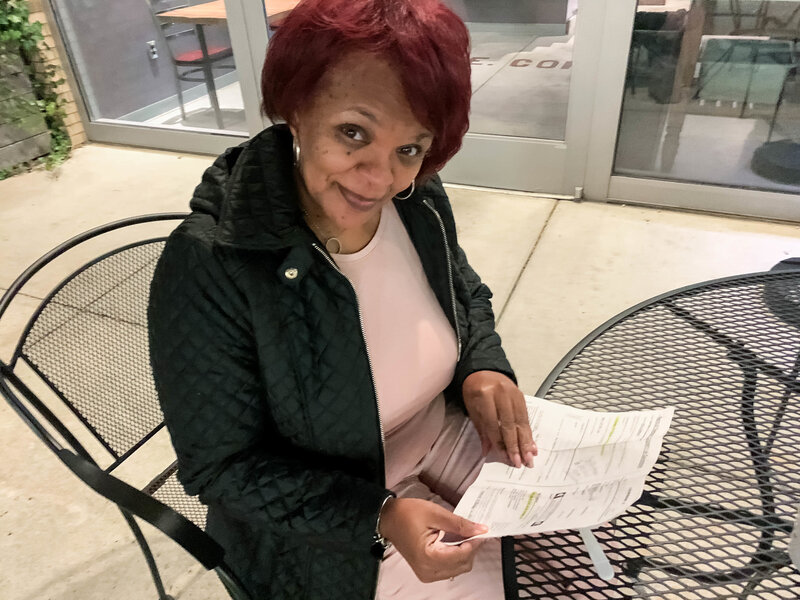
Social worker Sonya Johnson received a civil warrant to appear in court when the company that runs Nashville General Hospital’s emergency room threatened to sue her over a $2,700 ER bill — long after she’d already negotiated a reduced payment schedule for the rest of her hospital stay.
Nashville General Hospital is a safety net facility funded by the city. For a patient without insurance, this is supposed to be the best place to go in a city with many hospitals. But for those who are uninsured, it may have been the worst choice in 2019.
Its emergency room was taking more patients to court for unpaid medical bills than any other hospital or practice in town. A WPLN investigation finds the physician-staffing firm that runs the ER sued 700 patients in Davidson County during 2019.
They include patients such as Sonya Johnson, a 52-year-old social worker and single mother.
By juggling her care between a nonprofit clinic and Nashville General, Johnson had figured out how to manage her health problems, even though she was, until recently, uninsured. In 2018, she went in to see her doctor, who charges patients on a sliding scale. Her tongue was swollen and she was feeling weak. The diagnosis? She was severely anemic.
“He called me back that Halloween day and said, ‘I need you to get to the emergency [room], stat — and they’re waiting on you when you get there,’ ” she recalls.
Nashville General kept her overnight and gave her a blood transfusion. They wanted to keep her a second night — but she was worried about the mounting cost, so asked to be sent home.
Staying overnight even the one night meant she was admitted to the hospital itself, and the bill for that part of her care wasn’t so bad, Johnson says. The institution’s financial counselors offered a 75% discount, because of her strained finances and because her job didn’t offer health insurance at the time.
But emergency rooms are often run by an entirely separate entity. In Nashville General’s case, the proprietor was a company called Southeastern Emergency Physicians. And that’s the name on a bill that showed up in Johnson’s mailbox months later for $2,700.
“How in the world can I pay this company, when I couldn’t even pay for health care [insurance]?” Johnson asks.
Johnson didn’t recognize the name of the physician practice. A Google search doesn’t help much. There’s no particular website, though a list of Web pages that do turn up in such a search suggest the company staffs a number of emergency departments in the region.
Johnson says she tried calling the number listed on her bill to see if she could get the same charity-care discount the hospital gave her, but she could only leave messages.
And then came a knock at her apartment door over the summer. It was a Davidson County sheriff’s deputy with a summons requiring Johnson to appear in court.
“It’s very scary,” she says. “I mean, [I’m] thinking, what have I done? And for a medical bill?”
Nashville General Hospital was no longer suing patients
Being sued over medical debt can be a big deal because it means the business can get a court-ordered judgment to garnish the patient’s wages, taking money directly from their paycheck. The strategy is meant to make sure patients don’t blow off their medical debts. But this is not good for the health of people who are uninsured, says Bruce Naremore, the chief financial officer at Nashville General.
“When patients owe money, and they feel like they’re being dunned all the time, they don’t come back to the hospital to get what they might need,” he says.
Under Naremore’s direction in the past few years, Nashville General had stopped suing patients for hospital fees. He says it was rarely worth the court costs.
But Southeastern Emergency Physicians — which, since 2016, has been contracted by the hospital to run and staff its emergency department — went the other way, filing more lawsuits against patients than ever in 2019.
Naremore says the decision on whether to sue over emergency care falls to the company that staffs the ER, not Nashville General Hospital.
“It’s a private entity that runs the emergency room, and it’s the cost of doing business,” he says. “If I restrict them from collecting dollars, then my cost is going to very likely go up, or I’m going to have to find another provider to do it.”
This is a common refrain, says Robert Goff. He’s a retired hospital executive and board member of RIP Medical Debt. The nonprofit helps patients who are trapped under a mountain of medical bills, which are the No. 1 cause of personal bankruptcy.
“So the hospital sits there and says, ‘Not my problem.’ That’s irresponsible in every sense of the word,” Goff says.
The practice of suing patients isn’t new for Southeastern Emergency Physicians or its parent company, Knoxville-based TeamHealth. But such lawsuits have picked up in recent years, even as the company has stopped its practice of balance billing patients.
TeamHealth is one of the two dominant ER staffing firms in the nation, running nearly 1 in 10 emergency departments in the United States. And its strategy of taking patients to court ramped up after it was purchased by the private equity giant Blackstone, according to an investigation by the journalism project MLK50 in Memphis.
Under pressure from journalists, TeamHealth ultimately pledged to stop suing patients and to offer generous discounts to uninsured patients.
Officials from TeamHealth declined WPLN’s request for an interview to answer questions about how widespread its practice of suing patients for ER doctors’ services and fees has been.
“We will work with patients on a case by case basis to reach a resolution,” TeamHealth said in an email.
According to court records obtained by WPLN, the firm filed about 700 lawsuits against patients in Nashville in 2019. That’s up from 120 in 2018 and just seven in 2017. Its only contract in the city is with Nashville General’s ER, and the patients reached by WPLN say they were uninsured when they were sued.
What’s surprising to Mandy Pellegrin, who has been researching medical billing in Tennessee at the nonpartisan Sycamore Institute, is that it was all happening at Nashville General — where treating uninsured patients is part of the hospital’s mission.
“It is curious that a company that works for a hospital like that might resort to those sorts of actions,” Pellegrin says.
TeamHealth halts suits, pledges to drop cases
As for Sonya Johnson — she eventually went to court and worked out a payment plan of $70 a month over three years.
And now TeamHealth tells WPLN that its intent is to drop pending cases.
“We will not file additional cases naming patients as defendants and will not seek further judgments,” a TeamHealth spokesperson says in an emailed statement. “Our intent is not to have these pending cases proceed. We’re working as expeditiously as possible on resolving individual outstanding cases.”
Johnson says she’s been told that the lawsuit Southeastern Emergency Physicians filed against her will be dropped — but that she still owes the $2,700 bill.
Hospitals as medical debt litigators
Tax-exempt hospitals are again raising eyebrows over how they harass patients, often the poorest, in court by trying to recoup medical debts, my colleague Bob Herman writes.
Driving the news: ProPublica and MLK50 published a deep dive yesterday on Methodist Le Bonheur Healthcare, a $2 billion not-for-profit and faith-based hospital system in Tennessee that has filed more than 8,300 lawsuits against patients over the past 5 years.
- One of the patients featured in the story made less than $14,000 last year, and Methodist is suing her for more than $33,000. The hospital operates in the second-poorest large metropolitan area in the nation.
- Methodist obtained wage garnishment orders in almost half of the cases it filed between 2014 and 2018, meaning that the debtor’s employer was required to send the court a portion of the worker’s after-tax income.
Between the lines: As we wrote this week, hospitals taking patients to court is both common and longstanding.
- And when hospitals don’t get what they want from collections or the courts, they occasionally seize patients’ tax refunds.
The bottom line: Not-for-profit hospitals market themselves as charities, but they act more like for-profit peers — renewing questions of whether those organizations’ tax exemptions are justified.
- Coincidentally, the American Hospital Association released a paper Thursday touting hospitals’ community benefits, but the paper has some of the same flaws as prior analyses.
What we’re watching: These practices have drawn the ire of Sen. Chuck Grassley, who is now chairman of the powerful Finance Committee.
- “Such hospitals seem to forget that tax exemption is a privilege, not a right. In addition to withholding financial assistance to low-income patients, they give top executives salaries on par with their for-profit counterparts,” Grassley wrote in a 2017 op-ed.

